Double Culprit in A Patient who Presented in Coma: A Perlexing but Rewarding Case.
Double Culprit in A Patient who Presented in Coma: A Perlexing but Rewarding Case.
Dr Anand R Shenoy *1, Dr Kishan Raj K 2, Dr Suraj Sudhish Palavilayil 3
1. Dr Anand R Shenoy, MBBS, MD, DM, FICC, FSCAI, MEAPCI, FESC, FACC, and FRCP (ED), Dept Of Cardiology, Consultant Intervventional Cardiology, Manipal Hospitals, Old Airport Road, Bengaluru, Karnataka, India- 560017.
2. Dr Kishan Raj K, MBBS, MD, DrNB Cardiology Resident, Manipal Hospitals, Old Airport Road, Bengaluru, Karnataka, India- 560017.
*Correspondence to: Dr Anand R Shenoy, MBBS, MD, DM, FICC, FSCAI, MEAPCI, FESC, FACC, and FRCP (ED), Dept Of Cardiology, Consultant Intervventional Cardiology, Manipal Hospitals, Old Airport Road, Bengaluru, Karnataka, India- 560017.
Copyright
© 2024 Dr Anand R Shenoy. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 18 June 2024
Published: 01 July 2024
Abstract
Acute thrombotic occlusion of more than one coronary artery causing STEMI is a rather rare finding in coronary angiography during primary angioplasty in myocardial infarction (PAMI). We present a case of a 72 year old male, with no known comorbidities who presented with acute anterior wall myocardial infarction (AWMI) in comatose condition. Coronary angiography showed thrombotic occlusion in Left anterior descending (LAD) and circumflex (LCx) arteries. Clinical condition improved after percutaneous transluminal coronary angioplasty (PTCA) of both arteries. Given this unique presentation, the best management is not standardized. However, quick decision making and proper timely revascularisation helps patients to achieve a full and excellent recovery post revascularisation. We further emphasise need for guideline directed therapy in patients presenting with such multiple culprit vessel lesions in STEMI.
KEY WORDS: Double culprit vessels, Acute myocardial infarction, coma.
Double Culprit in A Patient who Presented in Coma: A Perlexing but Rewarding Case.
Introduction
In spite of availability of therapeutic and preventative interventions, acute myocardial infarction (MI) with or without ST-segment elevation is one of the global leading causes of mortality. ST-elevation myocardial infarction (STEMI) causes epicardial coronary artery occlusion leading to localized infarction and myocardial necrosis due to atherothrombosis.1 Evidence has shown that STEMI typically occurs with a single culprit vessel; however, multi-vessel thrombosis is a rare condition associated with poor outcomes and a high fatality rate.2 Only 2.5% of STEMI patients encountered during percutaneous coronary intervention (PCI) are noted to have multiple acute coronary artery thromboses.3 Prevalence of dual culprit lesions in left coronaries during an ACS is a rarity reported in literature.
In prior studies, the most frequent angiographic outcome involved simultaneous thrombosis in both the left anterior descending (LAD) and right coronary arteries (RCA), treated with PCI and an intra-aortic balloon pump.2 Multi vessel coronary thrombosis can arise secondary to coronary vasospasm.4 Although most often cause remain unidentifiable. Currently, no guideline define the best management of STEMI with multiple culprit lesions.
In STEMI patients with hyperacute MI, and rapidly worsening hemodynamics, urgent PTCA to the culprit artery becomes necessary after an angiogram to save the patient’s life. Similar patients presenting with shock, LVF, arrhythmias and sometimes with coma/ syncope may have multiple responsible culprit arteries. Detection of this possibility of multivessel thrombosis is important. We present a rare case of acute MI due to multiple thrombotic occlusions highlighting the presentation, management, and outcome of the patient.
Case Report
72 Year old male with no comorbidities, was brought to ER in a state of unresponsiveness since 1 hour. Initial evaluation revealed normal vitals signs, GCS: E1V1M1, GRBS of 180mg/dL. ABG was also normal. He was intubated for airway protection. ECG changes (FIG1) were present as shown in the figure. ECHO done showed apical hypokinesia with LVEF 20%. He underwent a CT brain which revealed no acute infarct/ bleed. Troponin was elevated. He was taken up for primary PCI which revealed LAD and LCx having 100% thrombotic occlusions (FIG 2) which were successfully treated by 1X DES in LAD and 1xDES in LCx achieving TIMI 3 flow (FIG3) . Patient was extubated the following day as he regained consciousness with no end organ damage or shock. Timely intervention and inclusion of two arteries as culprit vessels, with such peculiar presentation as well as the ECG changes makes it a case of rarity. It also signifies the importance of treating the condition on an emergent basis to aid in complete recovery.
FIG 1: ECG AT EMERGENCY ROOM
FIG 2 : CORONARY ANGIOGRAM SHOWIN LAD AND LCX 100% THROMBOTTIC OCCLUSION
FIG 3: POST PCI
Discussion
The primary mechanism of STEMI is the rupture of the susceptible plaque with thrombus development. STEMI is often triggered by a single artery thrombosis and rarely caused by more than one culprit artery. In 50% of STEMI patients, this mechanism was discovered during an autopsy examination.6 However, plaque rupture with thrombus formation is seen only in 1.7 to 4.8% cases in STEMI patients undergoing PAMI.3 A possible explanation for this disparity is that majority of patients developing STEMI due to multiple culprit arteries die because of massive MI and related complications before reaching the hospital. Above incidence is not observed in patients undergoing PAMI. This may partly be due to clinicians’ unawareness leading to missing culprit lesions in other coronaries or tiny plaque ruptures causing inconspicuous angiographic findings. Kanei et al determined heightened inflammatory response with catecholamine surge due to acute blockage in one coronary artery leading to plaque rupture in other coronaries.7 Other possible mechanisms are coronary spasm, hypercoagulable state, coronary embolism or hemodynamic instability.6 Similar to the various factors explored by Mahmoud et al., our case contributes to the STEMI literature by presenting a scenario involving multiple coronary thromboses.2 Our case had multiple risk factors such as DM, hypertension, and smoking. Moreover, in our case, our patient had LVF associated with CHB which further accounted for simultaneous coronary thrombosis. Overall, acute MI cases are discovered to have multivessel obstructive coronary artery disease, and recommendations have addressed the benefits of culprit lesion alone PCI versus total revascularization of non infarct related arterial lesions.5 A complete revascularization guided by fractional flow reserve significantly lowered the risk of future events in STEMI patients with multivessel disease when compared to initial PCI without invasive procedures. Due to no differences in all-cause mortality, patients could safely have all lesions treated during the index hospitalization to prevent further revascularization.8 Multiple culprit lesions are not addressed in the 2015 ACC guidelines on primary PCI for STEMI; instead, it states that PCI of non-culprit lesions is reasonable in the STEMI. Additionally, hemodynamically stable multivessel diseases can be managed during primary PCI or as a planned stage procedure.5
In conclusion, our case study highlights the importance of complete revascularisation in cases with multiple vessel athero-thrombosis in order to provide optimal clinical outcomes to our patients with STEMI.
Reference
1. Assamti M, Benahmed I, Ismaili N, El Ouafi N. Acute double coronary occlusion and its misleading presentation: An unusual case report. Ann Med Surg (Lond). 2021;73:103133.
2. Mahmoud A, Saad M, Elgendy IY. Simultaneous multi-vessel coronary thrombosis in patients with ST-elevation myocardial infarction: a systematic review. Cardiovasc Revasc Med. 2015;16(3):163-6.
3. Pollak PM, Parikh SV, Kizilgul M, Keeley EC. Multiple culprit arteries in patients with ST segment elevation myocardial infarction referred for primary percutaneous coronary intervention. Am J Cardiol. 2009;104(5):619-23.
4. Yamazaki K, Funayama N, Okabayashi H, Myojo T, Gima M, Tanaka H, Sakamoto N, Kikuchi K. [Acute coronary syndrome due to coronary thrombus formed by severe coronary spasm: a case report]. J Cardiol. 2007;50(3):205-12.
5. Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al. 2015 ACC/AHA/SCAI Focused Update on Primary Percutaneous Coronary Intervention for Patients With ST-Elevation Myocardial Infarction: An Update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention and the 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction. J Am Coll Cardiol. 2016;67(10):1235-50.
6. Derian W, Hertsberg A. Acute myocardial infarction from simultaneous total occlusion of the left circumflex and right coronary artery. A case report. Int J Cardiol. 2007;119(2):e65-7.
7. Kanei Y, Janardhanan R, Fox JT, Gowda RM. Multivessel coronary artery thrombosis. J Invasive Cardiol. 2009;21(2):66-8.
8. Engstrøm T, Kelbæk H, Helqvist S, Høfsten DE, Kløvgaard L, Holmvang L, et al. Complete revascularisation versus treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANAMI-3—PRIMULTI): an open-label, randomised controlled trial. Lancet. 2015;386(9994):665-71.
9. Benjelloun Bennani H, Boukili Makhoukhi Y, Champagne S, Dubois-Randé JL. A case report of an acute myocardial infarction with simultaneous occlusion of circumflex and right coronary artery. Ann Cardiol Angeiol (Paris). 2010;59:238-42.
10. Wu L, Huang G, Yu X, Ye M, Liu L, Ling Y, et al. Deep Learning Networks Accurately Detect ST Segment Elevation Myocardial Infarction and Culprit Vessel. Front Cardiovasc Med. 2022;9:797207.

Figure 1
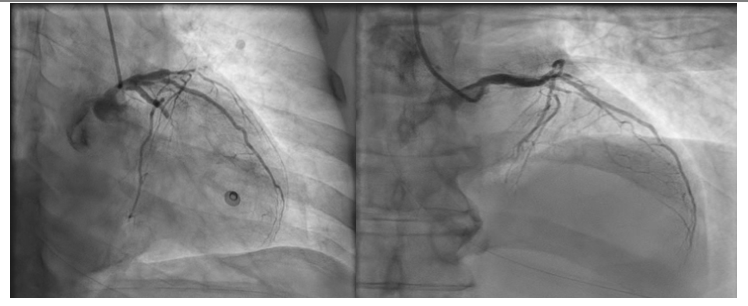
Figure 2

Figure 3
