A Study between Two Different Doses of Intravenous Dexmedetomidine during Spinal Anaesthesia
A Study between Two Different Doses of Intravenous Dexmedetomidine during Spinal Anaesthesia
Dr. Denika Patel1*, Dr. Darshana Shah2, Dr. Happy Patel3
1. 3rd Year Resident Department of Anaesthesiology at SVP Hospital , Ahemdabad.
2 Associate Professor in Department of anaesthesia at SVP Hospitals, Ahemdabad.
3. Consultant ENT surgeon Ahemdabad.
*Correspondence to: Dr. Denika Patel, 3rd Year Resident Department of Anaesthesiology at SVP Hospital , Ahemdabad.
Copyright
© 2023 Dr. Denika Patel. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 11 July 2024
Published: 25 July 2024
Abstract
Background: Spinal anaesthesia, considered the gold standard for lower abdominal and lower limb surgeries, can cause patient discomfort and anxiety. Sedation is commonly used to improve patient satisfaction. This study compares the effects of two doses of intravenous dexmedetomidine for sedation during spinal anesthesia.
Aim: To assess the effects of two different doses of intravenous dexmedetomidine on sedation, duration of analgesia, hemodynamic stability, and perioperative adverse effects during spinal anaesthesia.
Material and methods: Sixty adult patients, ASA I-II, scheduled for lower abdominal and lower limb surgeries were divided into two groups. Group I received dexmedetomidine at 0.25 μg/kg/hr, while Group II received 0.45 μg/kg/hr. Both groups were given a loading dose of 0.5 μg/kg IV dexmedetomidine before spinal anaesthesia. Sedation levels, hemodynamic parameters, and the time to the first analgesic request were recorded intraoperatively and postoperatively.
Result: Both groups achieved satisfactory sedation levels with no significant differences in hemodynamic parameters. Group II experienced a significantly longer duration of analgesia (318.5 ± 16.63 minutes) compared to Group I (267 ± 12.18 minutes). No significant perioperative adverse effects were noted in either group.
Conclusion: Both doses of intravenous dexmedetomidine effectively provide sedation and maintain hemodynamic stability during spinal anesthesia. The higher dose of 0.45 μg/kg/hr prolongs the duration of analgesia, enhancing postoperative pain management. Dexmedetomidine is a valuable adjunct for improving patient comfort and satisfaction during spinal anesthesia. Further research is recommended to optimize dosing strategies.
A Study between Two Different Doses of Intravenous Dexmedetomidine during Spinal Anaesthesia
Introduction
Spinal anaesthesia/Subarachnoid block (SAB) is considered the gold standard method for anaesthesia in lower abdominal and lower limb surgery because it is economical, easy to perform, offers excellent operating conditions, and has a reasonable safety-effectiveness profile. Many spinal and epidural anaesthetics have failed more because of insufficient sedation and anxiolysis than because of technically defective blocks [1]. The intrathecal local anaesthetic 0.5% bupivacaine is frequently used for surgeries lasting for 2- 2.5 hours. Adjuvants from different pharmacological classes of drugs are used to prolong the action of analgesia and enhance the efficacy of spinal anaesthesia.
However, many patients also experience discomfort and fear due to the severe sensory and motor paralysis, ongoing supine position, and immobility
Regional anaesthesia undoubtedly has the benefit of allowing a patient who is conscious, spontaneously breathing, and able to maintain a patent airway during the surgical process. However, the same "consciousness" that occurs during surgery could be a cause in the anxiety and dissatisfaction of the patient. Fear of being awake during surgery, fear of needles, and fear of numbness wearing off early were expressed as major factors for refusal of spinal anaesthesia by patients. Multiple other reasons such as cold operating environment, new people, awkward positioning and need to lie down in the supine position for longer periods may increase patient anxiety and reduce patient satisfaction (PS) with anaesthesia care.Sedation has been shown to improve patient satisfaction during regional anaesthesia[2] .
A patient under conscious sedation is one who is deliberately responding to verbal commands while experiencing a drug-induced state of depression of consciousness, either alone or accompanied by minimal tactile stimulation. Intervention is not necessary to maintain a patent airway and cardiovascular stability. In the past, people referred to this type of sedation as conscious sedation.
To obtain the goals of adequate sedation for patients under spinal anaesthesia, many drugs have been studied, such as Midazolam, Propofol, Midazolam-Remifentanil combination, Clonidine and Dexmedetomidine. With Midazolam, respiratory depression was a concern. With Propofol, hemodynamic instability and respiratory depression were to be managed. Higher incidence of bradycardia with Clonidine was a drawback.[3-6].
Dexmedetomidine, a selective alpha2-adrenergic agonist, affects the locus caeruleus area, which is related to the modulation of sleep regulation and respiratory control, and has a sedative effect. The analgesic effect is due to the activation of the alpha2-adrenergic receptors of the central nervous system [7,8]. Dexmedetomidine reduces biological stress responses and reduces the heart rate and blood pressure to moderate levels by lowering catecholamine secretion. It also has minimal or no effect on the respiratory rate and tidal volume [9]. However, the use of dexmedetomidine can cause prolonged recovery [10,11]. It is well suited for the patient and surgeon’s perspective on satisfaction with the anaesthetic care is an important indicator of the quality of perioperative care. Intravenous Dexmedetomidine, prolongs the duration of spinal anaesthesia by inducing sedation and increasing post-operative analgesia with minimal effect on cardiovascular and respiratory systems.
Taking the advantage of these properties, we decided to study the effects of Dexmedetomidine by administering it intravenously in association with the spinal anaesthesia.
Aims and Objectives
Aim:
To study two different doses of Dexmedetomidine for sedation during spinal anaesthesia
Objectives:
Degree of sedation by Ramsay Sedation Scores
Duration of analgesia among the groups
Perioperative hemodynamic stability.
Perioperative adverse effects and complications.
Method
Following informed consent from the patients and their families, 60 adult patients, aged 18 to 60 years, with physical statuses of ASA grades I and II who were scheduled for lower abdominal and lower limb surgeries were included in this prospective observational study.
Inclusion criteria:
Age between 18 to 60 years of either gender
ASA grade 1 and 2 patients.
Exclusion criteria
ASA grade 3 and 4 patients.
Patients allergic to any drugs.
Any contraindication to spinal anaesthesia like Local site infection & coagulation abnormalities
Patients on treatment with adrenergic blockers, calcium channel blockers or with a history of alcohol, opioid or sedative abuse.
Patients were randomly divided into two groups.
GROUP I : who received INJ. infusion dexmedetomidine IV 0.25 μg/kg/hr, and
GROUP II:who received INJ. infusion dexmedetomidine IV 0.45 μg/kg/hr.
Pre-anesthetic evaluation including history taking, systemic examination and local examination were carried out a day before surgery. On the day of surgery an 18G intravenous (IV) cannula was secured and preloaded with 15 ml/kg of Ringer's lactate. On the operation table monitors like ECG , non invasive blood pressure , and pulse oxymeter were connected and baseline parameters recorded.
Both the groups received a loading dose of INJ.dexmedetomidine 0.5 mcg/kg IV over 10 minutes before performing subarachnoid block.
The SAB method was standardized in both groups by selecting the patient in the seated position for the administration of SAB, L3-L4 interspace, standard midline access using a 25G Quincke’s needle. 3 ml to 3.5 ml of 0.5% hyperbaric bupivacaine was administered intrathecally and immediately after completion of the injection the patients were placed in supine position. Immediately after positioning, the study participants were given the study drug as per the group allocation.IV Inj. infusion dexmedetomidine of 0.25 mcg/kg/hr was started in patients included in Group I and 0.45mcg/kg/hr was started in patients included in Group II. Intraoperative infusion of IV dexmedetomidine administration in both groups was discontinued as soon as the surgeon started suturing the skin.
Sedation using OASS , heart rate (HR), mean arterial pressure (MAP), respiratory rate (RR), Spo2 and and time for first analgesic request were recorded baseline before loading dose of IV Inj. dexmedetomidine at regular interval till the end of the surgery and postoperatively every 30 min for 2 hours and every hour for the next 3 Hours.
MODIFIED OBSERVER’S ASSESSMENT OF ALERTNESS/SEDATION SCALE (OASS) (12):
• 5 -Reacts quickly when name is said in a normal tone
• 4 - lethargic response when name is said in a normal tone
• 3 -Reacts only when name is called loudly and/or repeatedly
• 2 -Reacts only to gentle poking or shaking
• 1--Does not react to unpleasant stimuli
The time for the first request for analgesia, which was considered to be the duration of analgesia was noted.
Fall in systolic blood pressure to less than 90 mm Hg or less than 20% of baseline value was defined as hypotension and was treated with Inj. Mephentermine 3 mg bolus doses in increments. Similarly, bradycardia was defined as fall in heart rate to less than 60 beats per minutes and treated with Inj. Atropine 0.6 mg bolus doses.
For Statistical analysis collected data was entered in the excel data sheet and data analysis was done . Data were compiled using Microsoft excel and were statistically described in terms of mean + standard deviation (SD) or frequencies (number of cases) and percentage accordingly. For comparing categorical data Chi square test was performed. Unpaired t test was used to compare two population means. P value < 0.05 was considered statistically significant.
Results
60 adult patients, aged 18 to 60 years, with physical statuses of ASA grades I and II who were scheduled for lower abdominal and lower limb surgeries were included in this study.
Table-1: Demographic Characteristics
|
Parameters |
Group D1 |
Group D2 |
p Value |
|
Age in Years |
35.55 ± 6.52 |
35.95 ± 9.07 |
0.87 |
|
Weight in Kg |
57.65 ± 3.31 |
59.70 ± 4.19 |
0.97 |
|
Height in cm |
157.80 ± 4.82 |
159.35± 4.28 |
0.29 |
|
Male: Female |
12:8 |
11:9 |
0.74 |
|
ASA Grade I: II |
8:12 |
11:9 |
0.34 |
|
Duration of Surgery in Hrs |
2.06 ± 0.32 |
1.95 ± 0.24 |
0.23 |
Table-2: Pre-Operative Hemodynamic Parameters (Mean+ Sd)
|
Parameter |
Group D1 |
Group D2 |
p Value |
|
Pulse (beats / min) |
83.60 + 6.01 |
84.70 + 5.60 |
0.55 |
|
Blood pressure (Systolic/Diastolic) (mm Hg) |
125.10 + 5.82 |
125.90+ 5.71 |
0.66 |
|
77.00 + 4.88 |
78.50 + 3.94 |
0.29 |
|
|
SpO2 % |
98.80 + 0.41 |
99.00 + 0.56 |
0.60 |
|
Respiratory rate (per min.) |
14.30 + 1.03 |
14.45 + 0.76 |
0.21 |
Graph 1 : Heart rate monitoring (mean) in beats per minute
It shows that there was no statistically significant difference between two groups with regards to heart rate intra operative and post operative period in both the groups(P > 0.05).
Graph 2 : Comparison systolic blood pressure (in mm hg)
It shows that there was no statistically significant difference between two groups with regards to SBP in intra operative and postoperative period in both the groups(P > 0.05).
Graph 3 : Comparison of intraoperative diastolic blood pressure (in mm hg) (mean)
It shows that there was no statistically significant difference between two groups with regards to DBP in intra operative and postoperative period in both the groups(P > 0.05).
Graph 4: Comparison mean arterial pressure (in mm hg) (mean)
It shows that there was no statistically significant difference between two groups with regards to MAP in intra operative and postoperative period in both the groups (P > 0.05).
Graph 5: Comparison of spo2
Graph 6 : Comparison of RR
It shows that there was no statistically significant difference between two groups with regards to SPO2 and RR in intra operative and postoperative period in both the groups(P > 0.05).
Table 3- Sedation score (according to OASS)
|
Sedation score |
No. (%) of patients |
|
|
|
GROUP I |
GROUP II |
|
5 |
0 |
0 |
|
4 |
7(21%) |
6(18%) |
|
3 |
20(60%) |
19(57%) |
|
2 |
3(9%) |
5(15%) |
|
1 |
0 |
0 |
Table 4: Time to First Rescue Analgesia in Minutes
|
Time To First Rescue Analgesia |
Mean(Min) |
P Value |
|
|
GROUP I |
267 + 12.18 |
GROUP I VS GROUP II = <0.05 |
|
|
GROUP II |
318.5 + 16.63 |
TABLE 4 shows, the time for the first rescue analgesia in a postoperative period was significantly longer in dexmedetomidine group II compared to the control group I
Discussion
This study investigated the sedative and analgesic effects of two different doses of intravenous dexmedetomidine administered during spinal anaesthesia in lower abdominal and lower limb surgeries. The findings provide significant insights into the optimization of sedative protocols to enhance patient comfort and satisfaction while maintaining hemodynamic stability.
Sedation Levels
Dexmedetomidine is known for its sedative properties without causing significant respiratory depression. In this study, sedation levels were assessed using the Modified Observer’s Assessment of Alertness/Sedation Scale (OASS). The results indicated that both groups achieved satisfactory sedation levels during the procedure, with the majority of patients in both groups falling into the categories of OAS/S 3 and 4. This suggests that dexmedetomidine, at both dosages, effectively provided the desired level of sedation. However, there was no significant difference between the two groups regarding sedation scores, indicating that increasing the dose from 0.25 μg/kg/hr to 0.45 μg/kg/hr did not substantially alter the depth of sedation.
Hemodynamic Stability
Hemodynamic stability is a crucial aspect of anaesthesia management. The study monitored heart rate, systolic and diastolic blood pressure, mean arterial pressure, respiratory rate, and SpO2 levels. The findings revealed no statistically significant differences between the two groups in any of these parameters. This indicates that both dosages of dexmedetomidine maintained stable hemodynamic conditions intraoperatively and postoperatively. The minimal impact on cardiovascular and respiratory systems underscores the safety profile of dexmedetomidine in the doses studied.
According to the observations of a study by Jai Song and co-workers [14], they suggested a dexmedetomidine loading dose of 1 μg/kg followed by a maintenance infusion of 0.25 μg/kg/hr as the most appropriate dose for continuous administration.
Postoperative Analgesia Duration
Primary analgesic effect could be attributed to the inhibitory effect of dexmedetomidine on the release of substance P from the dorsal horn of the
spinal cord [13]. One of the primary objectives was to compare the duration of analgesia between the two groups. The results showed a significant difference in the time to first rescue analgesia, with Group II (0.45 μg/kg/hr) experiencing a longer duration of analgesia compared to Group I (0.25 μg/kg/hr). This suggests that a dose of 0.45 mcg/kg dexmedetomidine not only provides effective sedation but also extends the analgesic effects, potentially enhancing postoperative comfort and reducing the need for additional analgesics.
Adverse Effects
Both groups were monitored for perioperative adverse effects and complications. There were no reports of significant adverse events such as severe hypotension, bradycardia, or respiratory depression. This aligns with previous studies highlighting the favourable safety profile of dexmedetomidine when used in appropriate doses.
Conclusion
The study concludes that intravenous dexmedetomidine, at both 0.25 μg/kg/hr and 0.45 μg/kg/hr, is effective in providing sedation during spinal anaesthesia without compromising hemodynamic stability. The higher dose of 0.45 μg/kg/hr offers the added benefit of prolonged analgesia, which can improve postoperative pain management. These findings support the use of dexmedetomidine as a valuable adjunct in spinal anaesthesia, enhancing patient satisfaction and overall perioperative care quality.
Reference
1. Brown DL. Spinal, epidural and caudal anaesthesia. In: Miller RD, editor. Miller's Anesthesia. 7th ed. Philadelphia:Churchill-Livingstone; 2000. pp. 1492
2. De Andres J, Valia JC, Gil A, Bolinches R. Predictors of patient satisfaction with regional anesthesia. Reg Anesth 1995; 20: 498-505.
3. Pratibha Jain Shah, Kamta Prasad Dubey, Kamal Kishore Sahare, Amit Agrawal. Intravenous dexmedetomidine versus Propofol for intraoperative moderate sedation during spinal anaesthesia: A comparative study. 2016;32(2):245-9.
4. Heo-Gyeong Ok, Seung-HoonBaek, Seong-Wan Baik, Hae-Kyu Kim, Sang-Wook Shin, and Kyung-Hoon Kim. Optimal dose of Dexmedetomidine for sedation during spinal anaesthesia. Korean J Anesthesiol. 2013 May; 64(5): 426–31.
5. Do?an Ö, Ünver S, Tunçer Y?, et al. Comparison of Dexmedetomidine versus Midazolam/Remifentanil combination for monitored anaesthesia care. Turk AnesthesiolReanim J. 2011;39(6):292–301.
6. Sindhu J, Nirmala B.C. Narasimha Reddy B & Sowmya G. A Comparative study of intravenous Dexmedetomidine and intravenous Clonidine for prolongation of bupivacaine spinal anaesthesia. IJGSACR. 2016 Dec;1(1): 5-16.
7. Kamibayashi T, Maze M. Clinical uses of alpha 2-adrenergic agonists. Anesthesiology 2000; 93: 1345-9.
8. Issa FG. Effect of clonidine in obstructive sleep apnea. Am Rev Respir Dis 1992; 145: 435-9.
9. Hsu YW, Cortinez LI, Robertson KM, Keifer JC, Sum-Ping ST, Moretti EW, et al. Dexmedetomidine pharmacodynamics: part I:crossover comparison of the respiratory effects of dexmedetomidine and remifentanil in healthy volunteers. Anesthesiology 2004; 101:1066-76.
10. Zeyneloglu P, Pirat A, Candan S, Kuyumcu S, Tekin I, Arslan G. Dexmedetomidine causes prolonged recovery when compared with midazolam/fentanyl combination in outpatient shockwave lithotripsy. Eur J Anaesthesiol 2008; 25: 961-7.
11. Makary L, Vornik V, Finn R, Lenkovsky F, McClelland AL, Thurmon J,
et al. Prolonged recovery associated with dexmedetomidine when used as a sole sedative agent in office-based oral and maxillofacial surgery procedures. J Oral Maxillofac Surg 2010; 68: 386-91.
12.Archives of Anesthesiology and Critical Care (Autumn 2023); 9(Supplement 2): 488-494.
13.COMPARATIVE EVALUATION OF TWO DIFFERENT DOSES OF INTRAVENOUS DEXMEDETOMIDINE INFUSION FOR SEDATION IN ISSN 2466-488X (Online) doi: 10.5937/sjait2204063R
14.7.Grant SA, Breslin DS, MacLeod DB, Gleason D, Martin G. Dexmedetomidine infusion for sedation during fiberoptic intubation: a report of three cases. J Clin Anesth. 2004 Mar;16(2):124-6. Doi: 10.1016/j.jclinane.2003.05.010. PMID: 15110375.
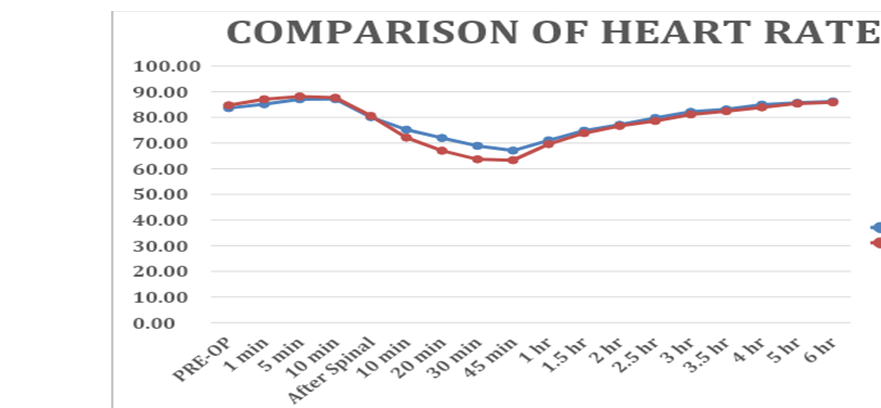
Figure 1
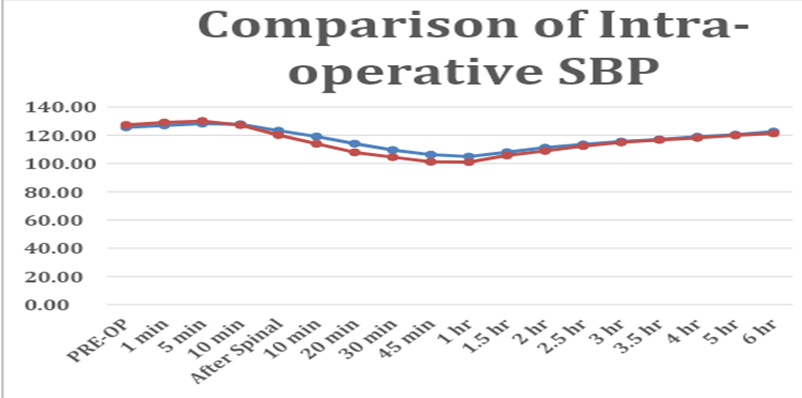
Figure 2
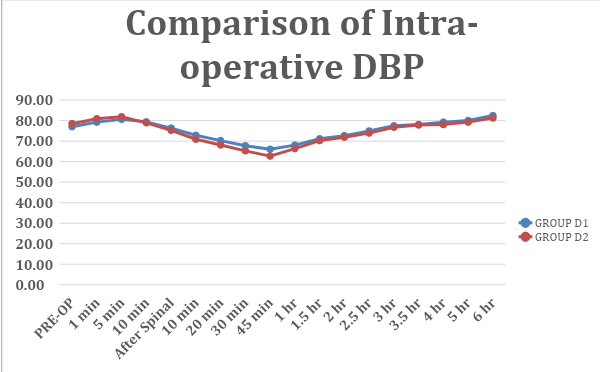
Figure 3
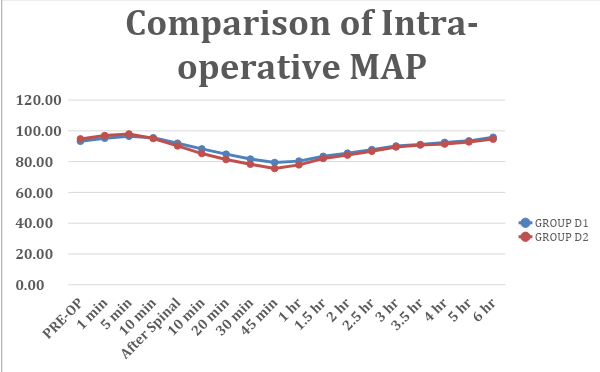
Figure 4
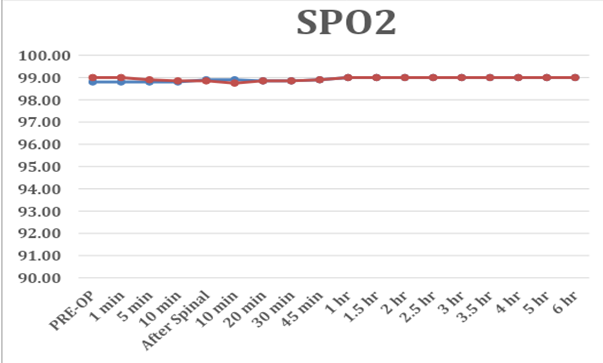
Figure 5
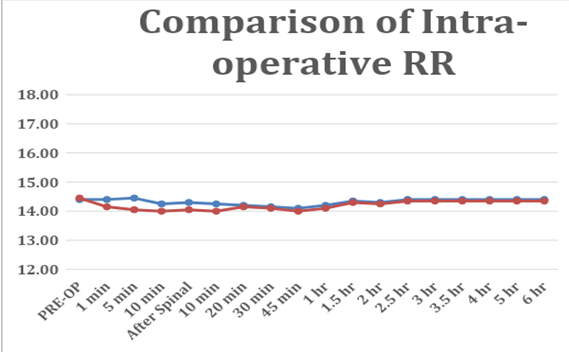
Figure 6

 Sd
Sd