Acute Pancreatitis an Unusual Complication of Influenza AH3 N2: A Case Report
Acute Pancreatitis an Unusual Complication of Influenza AH3 N2: A Case Report
Dr. Rasha Jarad
Correspondence to: Dr. Rasha Jarad, Pediatrics, Qatar.
Copyright
© 2024: Dr. Rasha Jarad. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 05 July 2024
Published: 01 Aug 2024
Abstract
Acute pancreatitis is an inflammatory disease of the pancreas, characterized by abdominal pain and high level of pancreatic enzymes. Pancreatitis is the most common disease of pancreas in children and adults. For the diagnosis we need 2 of 3 characteristics: abdominal pain characteristic of acute pancreatitis, amylase and/or lipase 3 times higher than the normal upper limit and characteristic findings in images. This case of 11 year old is associated with H3N2 Influenza virus were reported with uncomplicated features.
Key words: pancreatitis, acute necrotizing pancreatitis, Infuenza Virus
Acute Pancreatitis an Unusual Complication of Influenza AH3 N2: A Case Report
Introduction
Acute pancreatitis (AP), whose incidence in the pediatric population is increasing, it is defined such as the histological presence of inflammation within the pancreas. It is an inflammatory disease of the pancreas characterized by abdominal pain and elevated levels of pancreatic enzymes. The etiology of PA varies according to age. pediatric: poisoning, trauma, metabolic diseases and infections. Between The latter have been described in association with malaria, leptospirosis, HIV, mumps, ascaris, coxsackie, mycoplasma, myxovirus, hepatitis A and B, cytomegalovirus, chickenpox, herpes simplex 1 and 2, biliary or periampullary obstruction, drugs, vascular causes, post C-reactive protein (CRP), here ditary pancreatitis, cystic fibrosis (CF) and Reye syndrome.1,2 Although the association with the virus is known of influenza A, H3N2 influenza, in a child and all classified as mild due to their severity.2-4
Influenza A is a subtype of the influenza virus that can cause acute respiratory illness in humans and various animals, including birds and pigs. It is a single-stranded RNA virus belonging to the Orthomyxoviridae family. Influenza A viruses are characterized by their ability to mutate rapidly, leading to the emergence of new strains that can evade the immune system. This high mutation rate is due to the virus's segmented genome, which allows for genetic reassortment when two different strains infect the same host.
Influenza A viruses are categorized based on two surface proteins: hemagglutinin (H) and neuraminidase (N). There are 18 known hemagglutinin subtypes and 11 neuraminidase subtypes, leading to various combinations such as H1N1 and H3N2, which are common in seasonal flu outbreaks. Some strains of Influenza A, like H5N1 and H7N9, are of particular concern due to their potential to cause severe illness and pandemics.
Transmission of Influenza A occurs through respiratory droplets from coughing and sneezing, as well as through contact with contaminated surfaces. Symptoms typically include fever, cough, sore throat, body aches, and fatigue. In some cases, especially among the very young, elderly, or those with weakened immune systems, complications such as pneumonia can occur, potentially leading to severe illness or death.
Prevention of Influenza A includes annual vaccination, good hygiene practices like frequent hand washing, and the use of antiviral medications for treatment and prophylaxis in high-risk groups. Public health measures such as surveillance and rapid response to outbreaks are crucial in managing the spread of the virus.
Influenza A (H3) is a subtype of the Influenza A virus, characterized by the presence of hemagglutinin type 3 on its surface. H3 viruses are a significant cause of seasonal influenza in humans and have been responsible for several notable influenza outbreaks.
Characteristics of Influenza A (H3)
1. Hemagglutinin and Neuraminidase:
- The H3 subtype refers to the specific type of hemagglutinin protein found on the virus surface, which plays a crucial role in the virus's ability to bind to and enter host cells.
- Influenza A (H3) viruses can be paired with different neuraminidase (N) subtypes, but H3N2 is the most common combination found in humans.
2. Seasonal Influenza:
- H3N2 strains are commonly associated with seasonal flu outbreaks and tend to cause more severe illness, particularly in the elderly and young children.
- These strains often result in higher hospitalization and mortality rates compared to other subtypes like H1N1.
3. Mutation and Antigenic Drift:
- H3N2 viruses undergo frequent genetic changes, a process known as antigenic drift, leading to the emergence of new variants.
- This necessitates annual updates to the flu vaccine to ensure it remains effective against the most current strains.
4. Historical Impact:
- The H3N2 subtype first emerged in humans in 1968, causing the Hong Kong flu pandemic, which resulted in a significant number of deaths worldwide.
- Since then, H3N2 has been a recurring cause of seasonal flu epidemics.
Transmission and Symptoms
- Transmission: Similar to other influenza viruses, H3N2 spreads through respiratory droplets when an infected person coughs or sneezes, as well as through contact with contaminated surfaces.
- Symptoms: Include fever, cough, sore throat, runny or stuffy nose, body aches, headache, chills, and fatigue. In severe cases, it can lead to complications such as pneumonia.
Prevention and Treatment
- Vaccination: Annual flu vaccines are designed to protect against the most prevalent strains of Influenza A, including H3N2. The effectiveness of the vaccine can vary depending on how well it matches the circulating strains.
- Hygiene Practices: Regular hand washing, using hand sanitizers, and avoiding close contact with sick individuals can help reduce the spread of the virus.
- Antiviral Medications: Antiviral drugs like oseltamivir (Tamiflu) and zanamivir (Relenza) can be used to treat influenza and reduce the severity and duration of symptoms, especially if administered early in the course of the illness.
Public health surveillance and rapid response are critical in managing the impact of H3N2 outbreaks, along with ongoing research to develop more effective vaccines and treatments.
Case Report and Diagnosis
11 years old boy with history of allergic rhinitis on Montelukast. Presented to the end with the symptoms of on the last 10 days started to have fever reaching 39 partial responds to antipyretic associated with cough, runny nose and sore throat and 5 days of abdominal pain diffuses poorly localized severity 8/10 not no urinary symptoms no rash, no joint pain, no vomiting. Chest X ray was done showed Bronchitis.
The patient's physical examination was positive, with no acute distress, normal conjunctivae and lungs, and no lymphadenopathy. The chest showed equal air entry bilaterally, no crepitation or wheezes. The cardiovascular examination was normal, with no murmur or gallop. The abdomen showed soft tenderness, and the gastrointestinal examination was normal. The extremities and spine were symmetrical, and the skin was not rash-free. The neurological examination was grossly intact.
The patient is vitally stable, without respiratory distress, pain, or vomiting. He has a positive influenza A virus panel and a high lipase level. His CMP shows a picture of pancreatitis, and the GI team is contacted to maintain full maintenance of NPO and IV fluid.
A patient with pancreatitis was diagnosed with a positive result for nucleic acid from the target organism. The patient was prescribed medication, including PPL 40mg IV daily and Mometasone 50 mCg/inh, and was stable and pain-free. They had normal chest contour, movement, and no signs of respiratory distress. The abdomen was soft lax, with no tenderness or organomegaly. The patient's MSK showed no tenderness, redness, swelling, or stiffness, and no spinal abnormalities. The neuron was conscious and oriented, with normal power, tone, sensation, coordination, and cranial nerve exam. No clonus or Babinski was found.
Figure 1, Figure 2, Figure 3, Figure 4, Figure 5, Figure 6
Discussion & Conclusion
Influenza A (H3) is a significant cause of seasonal influenza in humans and have been responsible for several notable influenza outbreaks. H3N2 viruses can be paired with different neuraminidase (N) subtypes, but H3N2 is the most common combination found in humans. Seasonal influenza outbreaks often result in more severe illness, particularly in the elderly and young children, leading to higher hospitalization and mortality rates compared to other subtypes like H1N1.
The H3N2 subtype first emerged in humans in 1968, causing the Hong Kong flu pandemic, which resulted in a significant number of deaths worldwide. Since then, H3N2 has been a recurring cause of seasonal flu epidemics.
Transmission and symptoms of H3N2 include fever, cough, sore throat, runny or stuffy nose, body aches, headache, chills, and fatigue. In severe cases, it can lead to complications such as pneumonia.
Prevention and treatment include annual flu vaccines designed to protect against the most prevalent strains of Influenza A, including H3N2. Hygiene practices, such as regular hand washing, using hand sanitizers, and avoiding close contact with sick individuals, can help reduce the spread of the virus. Antiviral drugs like oseltamivir (Tamiflu) and zanamivir (Relenza) can be used to treat influenza and reduce the severity and duration of symptoms, especially if administered early in the course of the illness.
Public health surveillance and rapid response are critical in managing the impact of H3N2 outbreaks, along with ongoing research to develop more effective vaccines and treatments.
Although the most common complication of influenza infection is pneumonia, there is a rare viral factor in the etiology of acute pancreatitis.
References
1. Paljarvi T, Forton J, Luciano S, et al. Analysis of neuropsychiatric diagnoses after montelukast initiation. JAMA Netw Open. 2022;5(5):e2213643. PubMed CrossRef
2. Urdaneta E. Neuropsychiatric adverse drug reactions in children initiated on montelukast in real-life practice. Eur Respir J. 2017;50(5):1701984. PubMed CrossRef
3. Merck & Co., Inc. Singulair Package Insert. Accessed September 5, 2024. https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/021409s036lbl.pdf
4. Marschallinger J, Schäffner I, Klein B, et al. Structural and functional rejuvenation of the aged brain by an approved anti-asthmatic drug. Nat Commun. 2015;6:8466. PubMed CrossRef
5. Wilbur C, Bitnun A, Kronenberg S, et al. PANDAS/ PANS in childhood: controversies and evidence. Paediatr Child Health. 2019;24(2):85–91. PubMed CrossRef
6. Umetsu R, Tanaka M, Nakayama Y, et al. Neuropsychiatric adverse events of montelukast: an analysis of real-world datasets and drug-gene interaction network. Front Pharmacol. 2021;12:764279. PubMed CrossRef
7. Haarman MG, van Hunsel F, de Vries TW. Adverse drug reactions of montelukast in children and adults. Pharmacol Res Perspect. 2017;5(5):e00341. PubMed CrossRef
8. Eriksson Y, Boström M, Sandelius Å, et al. The anti asthmatic drug, montelukast, modifies the neurogenic potential in the young healthy and irradiated brain. Cell Death Dis. 2018;9(7):775. PubMed CrossRef
9. Naranjo CA, Busto U, Sellers EM, et al. A method for estimating the probability of adverse drug reactions. Clin Pharacol Ther. 1981;30:239–245. PubMed CrossRef
10. Pediatric Advisory Committee. FDA Briefing Document. Accessed September 5, 2024. Page 14. https://www.fda.gov/media/131035/download.
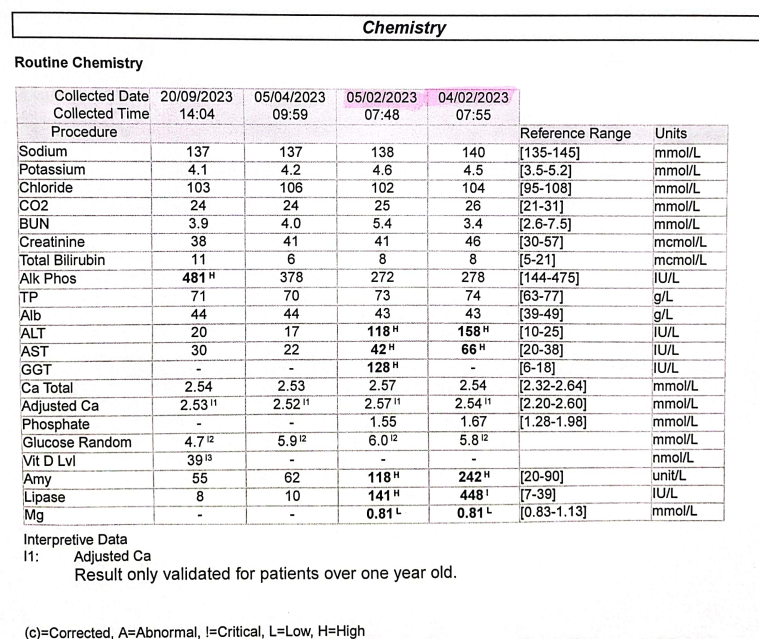
Figure 1
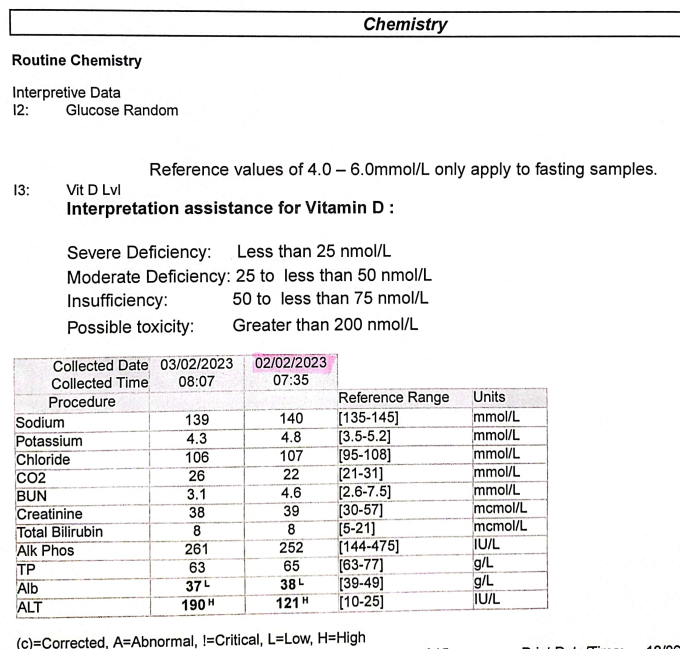
Figure 2
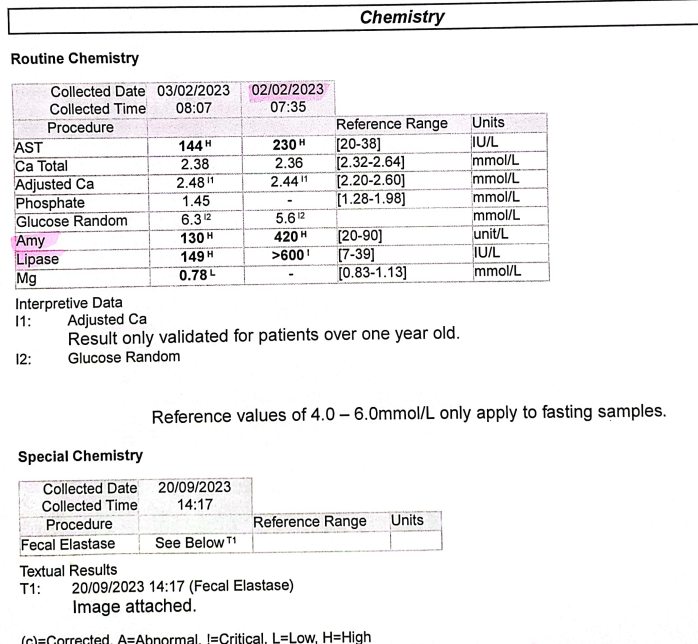
Figure 3
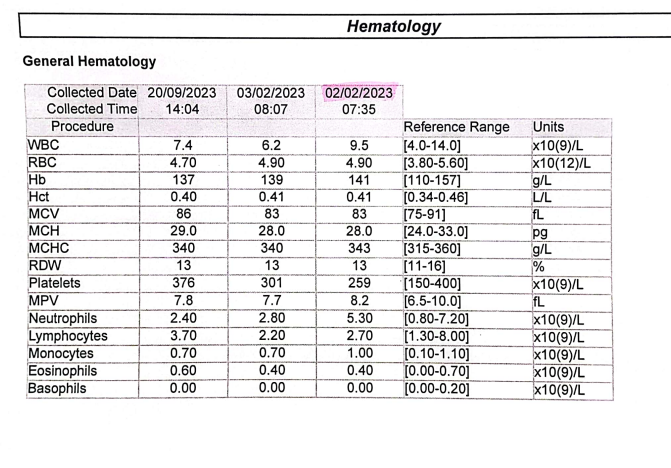
Figure 4
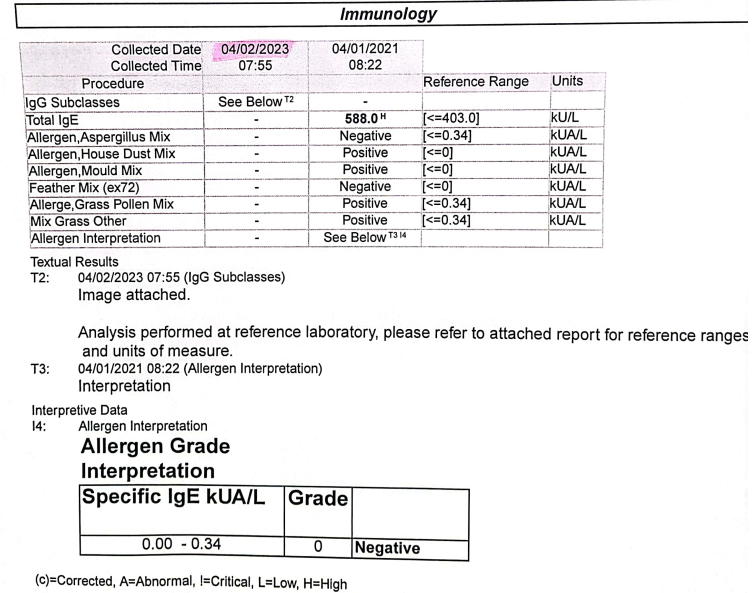
Figure 5
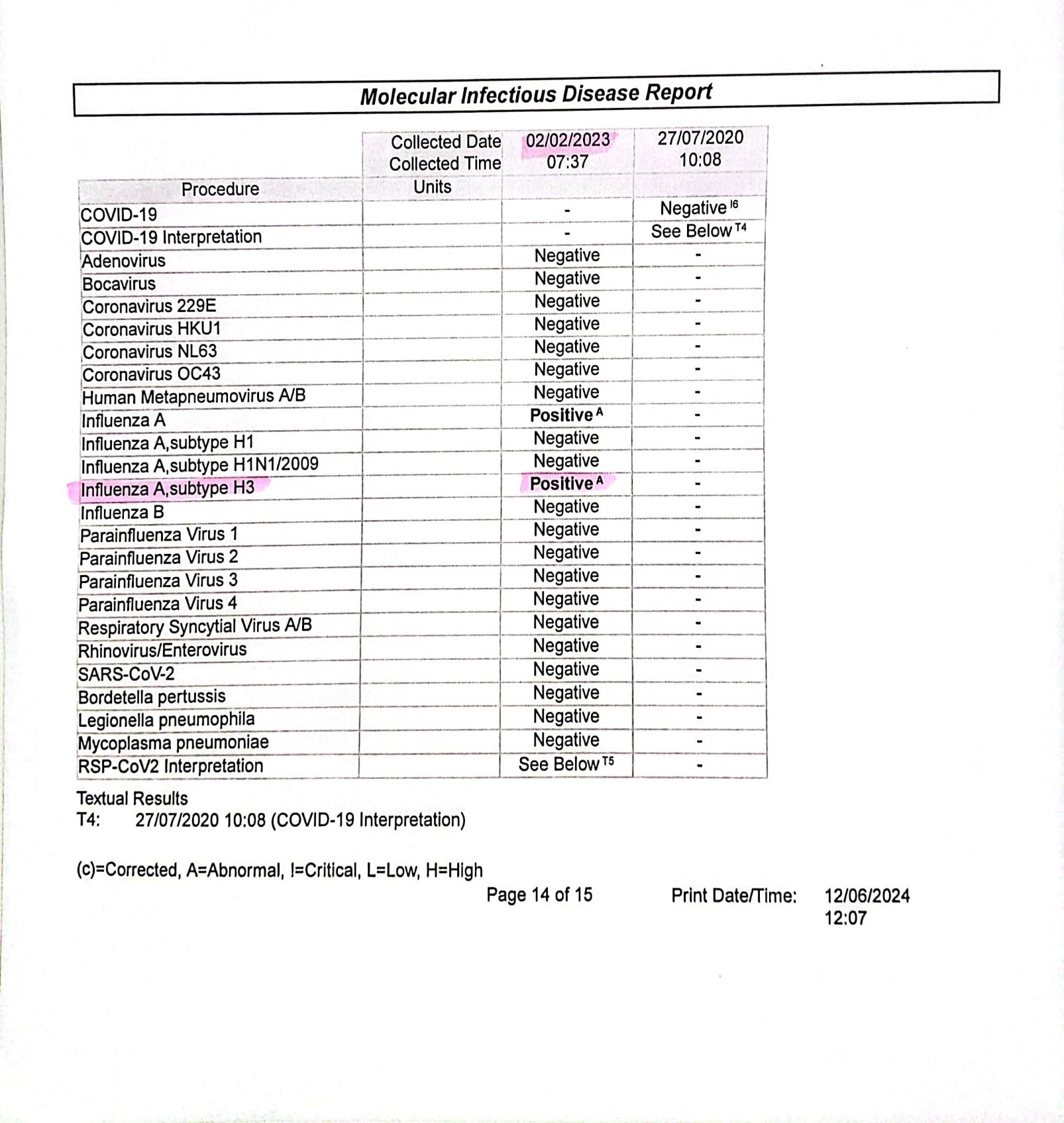
Figure 6
