Comparison of Succinylcholine and Rocuronium for Rapid Sequence Induction in Pediatrics Age Group
Comparison of Succinylcholine and Rocuronium for Rapid Sequence Induction in Pediatrics Age Group
Dr Mansi Shukla *1, Dr Pauravi Bhatt 2, Dr Meet Patel 3
1.3rd Year Anaesthesiology resident doctor, SVP Hospital and Smt. NHL Medical college, Ellisbridge, Ahmedabad, Gujarat.
2.Associate Professor, SVP Hospital and Smt. NHL Medical college, Ellisbridge, Ahmedabad, Gujarat.
3. First Year Anaesthesiology resident doctor, SVP Hospital and Smt. NHL Medical college, Ellisbridge, Ahmedabad, Gujarat.
*Correspondence to: Dr Mansi Shukla, 3rd Year Anaesthesiology resident doctor, SVP Hospital and Smt. NHL Medical college, Ellisbridge, Ahmedabad, Gujarat.
Copyright
© 2024: Dr Mansi Shukla. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 26 July 2024
Published: 06 August 2024
Abstract
Background: Succinylcholine has been the agent of choice for neuromuscular block when clinical conditions require emergency airway protection during a rapid-sequence induction of anaesthesia. Succinylcholine does have rapid onset but unfortunately there are many side-effects some of them are life threatening. Rocuronium bromide, non-depolarising muscle relaxants with a brief onset of action, but devoid of such side effects may be used as alternative to succinylcholine
Objective: The purpose of our study was to assess the onset and quality of muscle paralysis, the intubation condition of succinylcholine with Rocuronium.
Material and Method: Study was conducted in 80(n=80) ASA grade 1 children of age 5-10 years. Patients were given either Rocuronium 0.6mg/kg iv (n=40) or Succinylcholine 1 mg/kg (n=40). Neuromuscular blockade was quantified by assessing twitch response of adductor pollicis evoked after supramaximal stimulus of the ulnar nerve. Tracheal intubating conditions were assessed at 60 seconds by the Cooper scoring system for both groups. The neuromuscular block was assessed by using the single twitch stimulation. Onset of time was slightly more in Rocuronium (75.3±29.4sec) as compared to Succinylcholine (61.2±11.5sec). With Rocuronium 36 patients (95%) could have clinically acceptable intubating conditions at 60sec, while all were intubated at 60sec with Succinylcholine (100%).
Conclusion: We concluded that Rocuronium provides a good intubating condition at the same time as compared to succinylcholine. Thus its use is beneficial in patients requiring rapid tracheal intubation without any side effects.
Keywords: Neuromuscular relaxant: Rocuronium, Succinylcholine; Pediatric patients; neuromuscular monitoring, Rapid sequence induction.
Comparison of Succinylcholine and Rocuronium for Rapid Sequence Induction in Pediatrics Age Group
Introduction
The anatomy and physiology of neonates and infants are different from those of adults, creating challenges for anesthesiologists. Among them, of particular concern is the airway. Pediatric airways can be classified as 'normal', 'impaired normal', and 'known abnormal'.[1] The incidence of unanticipated difficult airways is higher in pediatric age groups than adults due to different airway anatomy, difficulty in airway examination, and congenital malformations.[2] Securing the airway of a pediatric patient in the operating theater is a real challenge for anesthesiologists. Controlled rapid-sequence intubation without cricoid pressure is a safe alternative for pediatric patients to manage a difficult airway.3 Succinylcholine, with rapid onset time and good intubating condition is still the drug of choice for rapid sequence endotracheal intubation. However, it falls short of the ideal muscle relaxants due to its potentially hazardous side effects. [4,5]
The time interval between the suppression of the protective reflexes by induction of anesthesia and development of satisfactory intubating conditions is the critical period for anesthetists. It is desirable therefore, that this period should be as short as possible. Ever since the advent of anaesthesia, anaesthesiologists have been in search of an ideal muscle relaxant, which can provide ideal intubating conditions in an ultra short duration with minimal side effects.
Succinylcholine has been the drug of choice for intubation since its introduction; doses of 1-1.5mg/kg provide an excellent intubating condition with short duration of action. But its use is strongly opposed in children because of multiple complications like an increase in intra- gastric, intracranial and intraocular pressure, risk of malignant hyperthermia in susceptible individuals, risk of rhabdomyolysis, recent burns injury, upper motor neuron diseases, septicemia, hyperkalemia due to any cause.[6,7,8] There are reports of rare but life-threatening malignant hyperpyrexia, hyperkalaemia, and cardiac arrests in young boys with undiagnosed muscular dystrophy. Considering these side effects and contraindications, efforts were made to find out a newer neuromuscular blocking agent with a comparable fast onset and shorter duration of action but without associated side effects of Succinylcholine.[9] Thus, in search for a newer neuromuscular blocking agent with rapid onset, brief duration of action and minimal side effects lead to the discovery of Rocuronium.[10,11] The works carried out by various workers [12] have confirmed the long held belief that a rapid onset of action can by the compounds of relatively low potency.
Rocuronium bromide is a steroidal (ORG 9426) non-depolarizing neuromuscular blocking drug, related structurally to Vecuronium. It was introduced in 1988 at the 9th World Conference of Anaesthesiologists in Washington.[13]
The rapid onset of action of Rocuronium was subject of several investigations determining if this compound allows rapid sequence.
The purpose of our study was to compare the onset of times as well as intubating conditions of succinylcholine and Rocuronium for endotracheal intubation at 60 sec in pediatric patients aged 5-10 years for an elective surgery.
Material and Method
After informed consent of parents, and institutional approval, the present study was conducted in 80(n=80) patients who were scheduled for a planned surgery. The intubating conditions were assessed at 60 sec using Succinylcholine and Rocuronium bromide.
Accordingly, patients were divided into two groups.
GROUP-A (n=40): Succinylcholine 1.0mg/kg at 60 sec.
GROUP-B (n=40): Rocuronium 0.6mg/kg at 60 sec.
Inclusion criteria:
Patients between 5-10 years of age of ASA-1. The current study was conducted in patients who were supposed to undergo elective surgery.
Exclusion criteria:
Patients who were known to have neuromuscular diseases or receiving medications known to influence neuromuscular functions and anticipated airway problem
A day before the surgery, all the patients were thoroughly assessed and examined systematically. Weight and height of the patient were recorded. All routine investigations were done. Vital data were noted and the patient was kept nil by mouth 6 hours before the surgery.
In the operating theater, standard monitoring (ECG, non invasive blood pressure, pulse oximetry and capnography) surface electrode of TOF (peripheral nerve locator) was applied to the opposite forearm, to the one that was used for intravenous line, to stimulate ulnar nerve. The two surface electrodes were placed over the volar side of the wrist, 2-3 cm apart from each other. Baseline measurements were recorded and an intravenous line was secured.
Total Score for intubation condition:
|
Score |
|
|
|
8-9 |
Excellent |
clinically acceptable |
|
6-7 |
Good |
|
|
3-5 |
Poor |
clinically unacceptable |
|
0-2 |
Bad |
Statistical analysis
The significance of difference between the two groups was assessed by chi-square test and unpaired 't' test. Significance was assured at P<0.05.
Result
80(n=80) patients of either sex aged 5-10 years, belonging to ASA grade 1 were included in the study. All the groups were comparable demographically.
In Rocuronium 36 patients had 100% suppression of a single twitch height and other 4 had 90%, while with succinylcholine only 24 patients developed 100% suppression and remaining 16 in the range of 92-95%. Slight diaphragmatic movement was noticed in 6(n=6) patients (15%) in group B as compared to 0% in group A , while coughing was present in 2(n=2) patients (5%) in group B.
INTUBATING CONDITIONS
All the patients in Group - A had excellent intubating conditions.
- In group-B, 32(n=32) patients (75%) had excellent intubating conditions, 6(n=4) patients (15%) had good intubating conditions and another 2(n=2) patients (5%) had poor intubating conditions.
- Thus in Group-B 38(n=38) patients (95%) had clinically acceptable intubating conditions.
All the patients were pre-medicated with Inj.Glycopyrrolate 0.004mg/kg and Inj.Fentanyl 1µg/kg intravenously.
All the patients were ventilated with 100% oxygen by a facemask. Before administration of a muscle relaxant the supramaximal stimulus was determined by observing the contraction of adductor pollicis; the maximum response was considered as the control height to compare further responses. After giving the intubating dose of muscle relaxants, a supramaximal set of Train of Four(TOF) stimuli was applied over the ulnar nerve at the wrist through surface electrodes and repeated every 10 sec and assessed for visual loss of adduction of the thumb and the disappearance of T1 of TOF stimuli. The time interval between the intubating dose and loss of T1 of TOF stimuli was considered as "onset time of intubation". And the time interval from injection of the muscle relaxants to 100% suppression of the control twitch, height was noted. Intubating conditions were assessed by an experienced anesthesiologist at 60 seconds after the administration of muscle relaxants for both groups. Intubating conditions were graded accordingly Cooper et al criteria.
|
Score |
Jaw relaxation |
Vocal cord position |
Response to Intubation |
|
0 |
Impossible to open |
Closed (adducted) Bucking |
Severe coughing |
|
1 |
Opens with difficulty |
Closing |
Mild coughing |
|
2 |
Moderate opening |
Moving movement |
Slight diaphragmatic |
|
3 |
Easy opening |
Open (relaxed) |
No movement |
|
|
GROUP A |
GROUP B |
|
Gender (M/F) |
30/10 |
25/15 |
|
Age (yrs) |
4.6±2.6 |
5.5±3.2 |
|
Weight (kg) |
20.3±8.9 |
33.0±10.0 |
|
TYPE OF SURGERY |
|
|
|
Orchidopexy |
9 |
8 |
|
Appendicectomy |
11 |
12 |
|
Tendon injury |
3 |
2 |
|
Hernia |
12 |
14 |
|
V.P.Shunt |
3 |
2 |
|
Burns Dressing |
2 |
2 |
TABLE 2: Demographic Data
|
|
Rocuronium |
Succinylcholine |
P value |
|
Onset time (sec) |
75.3±29.47 |
61.2±11.57 |
<0.001 |
The onset time was significantly shorter with succinylcholine than with rocuronium.
TABLE 3: Time course of action
RESPONSE TO INTUBATION
|
Response to Intubation |
Group A |
Group B |
|
None |
40(100%) |
32(75%) |
|
Slight diaphragmatic Movement |
- |
6(15%) |
|
Mild coughing |
- |
2(5%) |
|
Severe bucking or coughing |
- |
- |
TABLE 4: Comparison of response to Intubation between age group A and B
HEART RATE VARIATION
|
Time |
Group A |
Group B |
P value |
|
Before Induction |
116.50±7.24 |
114.70±8.39 |
>0.05 |
|
T1 |
126.95±6.61 (8.97%) |
123.45±8.90 (7.63%) |
>0.05 |
|
T2 |
119.75±6.73 (2.79%) |
120.10±7.16 (4.71%) |
>0.05 |
|
T3 |
116.40±6.79 (0.86%) |
116.70±7.00 (1.74%) |
>0.05 |
Maximum rise in heart rate was at 1 min after intubation (8.97%) in Group A and (7.63%) in Group B. But rise in heart rate was not clinically significant.(P>0.05)
TABLE 5: Comparison of mean heart rate between Group A and B
SYSTOLIC BLOOD PRESSURE VENTILATION
|
Time |
Group A |
Group B |
P value |
|
Before Induction |
98.20±7.20 |
101.15±8.89 |
>0.05 |
|
T1 |
106.75±6.29 (8.71%) |
108.35±8.73 (7.21%) |
>0.05 |
|
T2 |
104.10±5.45 (6.00%) |
106.40±7.92 (5.19%) |
>0.05 |
|
T3 |
99.90±6.77 (1.73%) |
102.35±8.64 (1.19%) |
>0.05 |
TABLE 06: Comparison of mean systolic blood pressure between Group A and B
Maximum rise in systolic blood pressure was at 1 min after intubation (8.7%) in Group A and (7.21%) in Group B. But the rise in systolic blood pressure was not clinically significant. (P >0.05)
COMPLICATIONS AT THE TIME OF LARYNGOSCOPY
|
Complication |
Group A |
Group B |
|
Bradycardia |
- |
- |
|
Laryngospasm |
- |
- |
|
VPB* |
4(10%) |
2(5%) |
|
Other |
- |
- |
|
Nil |
36(90) |
38(95%) |
*Ventricular premature beats.
TABLE 7: Comparison of complications at the time of laryngoscopy between Group A and B
This table shows that only 2 patients (100%) in Group A and only 1 patient (5%) in group B had ventricular premature beats during laryngoscopy.
Discussion
Provision of muscle relaxation for endotracheal intubation of patients, especially in an emergency surgery demands a relatively safer drug than Succinylcholine, that can provide good intubating conditions as early as possible with minimal side effects and a stable hemodynamic profile. Rocuronium has been introduced with low potency, with relatively shorter onset of action.
Neuromuscular blocking agents are required for smooth endotracheal intubation during general anesthesia. There are maximum chances of hypoxia, regurgitation and aspiration after induction of anaesthesia and before tracheal intubation. So, muscle relaxant should be such that it facilitates early intubation to decrease the chances of regurgitation.
Succinylcholine is a depolarizing neuromuscular blocking agent, which has been the gold standard since its introduction. Unfortunately it has many side effects. The United States and Germany have strongly advised discontinuation of it.
Unlike adults, pediatric patients are more sensitive to the side effects occurring following the use of succinylcholine. Accordingly its use has been decreased.[14]
The dose of rocuronium was chosen based on the best evidence available at the time of the design of the trial, that is, the Cochrane Review of 2003: For the outcome acceptable versus suboptimal intubating conditions, this review revealed no significant difference between succinylcholine and rocuronium at a dose of 0.6 to 0.7 mg/kg. Moreover, a sensitivity analysis within the propofol induction group (n = 640) for dose of rocuronium used (0.6 to 0.7 mg/kg versus 0.9 to 1.0 mg/kg) demonstrated that dose did not alter intubating conditions. Weighing the risk of prolonged neuromuscular blockade associated with higher doses of rocuronium against the lack of convincing evidence of better intubating conditions, we chose the smallest dose proven to be effective, that is, 0.6 mg/kg. However, the 2008 update of the Cochrane Review demonstrated an advantage of succinylcholine against lower (0.6 to 0.7 mg/kg), but not against higher (> 0.9 mg/kg), doses of rocuronium for the outcome acceptable versus suboptimal intubating conditions.[15] As the difference is small (risk ratio 0.95, 95% confidence intervals 0.90 to 0.99) and, as extensively discussed above, appeared to be mainly caused by the response to intubation[16], we decided not to modify the protocol of our ongoing trial.
Our study was conducted to compare the onset and the intubation condition between Rocuronium 0.6 Mg/kg and succinylcholine 1 mg/kg and to confirm that rocuronium is a suitable alternative even in pediatric patients because the onset of time and duration of neuromuscular blocking agent are somewhat different in children compared with adults.[17] Rocuronium Bromide is a steroidal non- depolarizing muscle relaxant that is useful to produce a rapid onset of action. Studies comparing Rocuronium and Succinylcholine in the onset time and quality of intubation have yielded varying results.
In the study conducted by SussanWoelfel et al[11] in pediatric patients aged 1-5 years, ED95 of rocuronium was determined to be 0.6mg/kg. O Kelly B et al[18] studied pharmacokinetics of rocuronium in pediatric patients and concluded that the weight rather than the body surface area is more useful for the calculation of pediatric dose of rocuronium. Based upon these guidelines rocuronium was given in a bolus dose of 0.6mg/kg in the present study.
Stoddart et al [19] compared intubating condition of Rocuronium 0.6mg/kg with Succinylcholine 1mg/kg in 60 children undergoing tonsillectomy, which showed that a clinically acceptable intubating condition was faster due to the use of opioids in their induction. In our study all the patients were given injection Fentanyl 1ug/kg.
In the present study, a standardized intubation technique has been used in which the intubation was attempted at 60 sec intervals, after administration of muscle relaxants and completed only when the intubating conditions were judged Clinically acceptable by using the CCC Rating scale. The observer was unaware about the twitch response. We observed that the intubating condition and paralysis of adductor pollicis muscle were poorly correlated. Our data supports the view that a suitable clinical intubating condition can be present with partial depression (75-80%) of the twitch response at wrist due to faster action of Rocuronium at the adductor muscle of the larynx.
The average clinical duration of the intubating dose of Rocuronium in pediatric patients is shorter than in adults (26+7 min observed by J Viby-Mogenson).[20] It may be due to the larger volume of distribution of the central compartment in pediatrics than in adults and more dynamic circulation.
Time Course of Action:
Singh et al21 had shown that with 0.6mg/kg Rocuronium and 1.5mg/kg Succinylcholine, the time to achieve maximum blockage was 87.94 and 65.59 sec respectively.
Stephan C Marsch et al22 showed that The duration of the intubation sequence was shorter after succinylcholine than after rocuronium (81 ± 38 sec versus 95 ± 48 sec; P = 0.002).
This is similar to our study that the onset of time was more with Rocuronium (75.329.4sec) than with Succinylcholine (61.2+11.5sec); the quality of neuromuscular block at larynx was comparable with an intubation score of 7-9 in both the group.
Response to Intubation:
Cooper et al23 assessed the intubating condition after administering Rocuronium bromide 0.6mg/kg at 60 and 90 sec and compared it with the intubating condition after Succinylcholine 1 mg/kg by using Cooper et al criteria. Intubating conditions were found to be clinically acceptable (good,excellent) in 95% of patients at 60 sec and in 100% of patients at 90 sec and in all the patients at both times after Succinylcholine.
Dr. MadhaviBarve24 compared the intubating condition between Succinylcholine 1 mg/kg and Rocuronium 0.6mg/kg in 40 ASA grade I-II children aged one to five years and observed no significant difference in intubating conditions or percentage of block in twitch height. concluded that with Rocuronium 13 patients (65%) of patients could be intubated at 60 sec and 20 (100%) at 90 seconds , while all were intubated at 60 sec with Succinylcholine.
Dr. AparnaShukla et al25 compared the intubating condition between Succinylcholine 1.5mg/kg and Rocuronium 0.6mg/kg and found that the intubating condition was clinically acceptable in all patients receiving Succinylcholine while 85% of patient had a clinically acceptable intubating condition with Rocuronium at 60 sec.
Stoddart et al19 conducted a blind, randomized study in 60 children undergoing elective tonsillectomy and compared intubating conditions at one minute with succinylcholine 1.0 mg/kg and rocuronium 0.6 mg/kg. They found that there was no difference in the intubating conditions at one minute, with 25 excellent and five good scores in the succinylcholine group and 27 excellent and three good scores in the rocuronium group.
In the present study, all the patients in group-A had excellent intubating conditions and in Group-B 32 patients (75%) had excellent intubating conditions. 6 patients (15%) had a good intubating condition and 2 patients (5%) had poor intubating condition. Thus 38 patients (95%) had a clinically acceptable intubating condition.
Vital Parameters:
There were no significant haemodynamic changes in both the groups. This may be due to prior administration of fentanyl. Slight increase in heart rate and mean pressure at 1 min post-intubation may be due to a stress response to intubation.
Complication at the Time of Laryngoscopy:
Only 2 patients (10%) in Group-A showed ventricular premature bets during laryngoscopy
Our study has several limitations. No control group was studied. Monitoring the adductor pollicis is not a useful measure for evaluating the neuromuscular block at larynx. Our results were obtained in normal healthy patients.
Conclusion
We concluded that though the succinylcholine is ideal muscle relaxants for rapid sequence induction, but in a scenario where anticipated difficult intubation and contraindication of Succinylcholine co-exist due to its own adverse effects, Rocuronium bromide, at a dose of 0.6mg/kg, an intermediate acting non depolarizing muscle relaxant with a brief onset of action but devoid of the adverse reactions that occur with Succinylcholine, may be a suitable alternative to Succinylcholine for rapid tracheal intubations at 60 sec in pediatric age groups.
References
1. Schmidt AR, Weiss M, Engelhardt T The paediatric airway: basic principles and current developments.. Eur J Anaesthesiol. 2014;31:293–299.
2. Amaha E, Haddis L, Aweke S, Fenta E The prevalence of difficult airway and its associated factors in pediatric patients who underwent surgery under general anesthesia: an observational study.. SAGE Open Med. 2021;9
3. Newton R, Hack H Place of rapid sequence induction in paediatric anaesthesia.. BJA Educ. 2016;16:120–123.
4. Rosenberg H. Gronert G.A.: Intractable cardiac arrest in children given succinylcholine. Anaesthesiology 1992:77,1054
5. Cooperman L.H. Strobel G.E.J. Kennel E.M: Massive hyperkalemia after administration of succinylcholine. Anaesthesiology 1970:32,161
6. Gerardi M. Alfred D.S, Richard C: Rapid sequence intubation of paediatric patients Emerg.Med 1996:55,74
7. C.L. Chiu, F. Jaais & C.Y. Wang: Effect of Rocuronium compared with Succinylcholine on intraocular pressure during rapid sequence induction of anaesthesia. B.J.A. 1999:82, 757-760.
8. MC Court K.C, L Salmela, R.K. Mirakhur et al: Comparison of Rocuronium and Suxamethonium for use during rapid sequence induction of Anaesthesia 1998:53,867-871
9. Rosenberg H, Gronert GA Intractable cardiac arrest in children given succinylcholine.. Anesthesiology. 1992;77:1054.
10. Fuchs Buder T. & E. Tassonyi: Intubating conditions and time course of Rocuronium,induced neuromuscular block in children. B.J.A. 1996:77,335-338.
11. Woelfel K. Susan: Effects of bolus administration of ORG-9426 in children during nitrous oxide-haloethane anaesthesia. Anaesthesiology 1992:76,939-942.
12. Ramzan J.M. : Molecular weight of cation as a determinant of speed of onset of neuromuscular blockade. Anesthesiology 1982:57,247-248
13. Khuenl Brady K.S. Castogonoli K.P: The neuromuscular blocking effects and pharmacokinetics of ORG 9426 and ORG 9616 in cat. Anaesthesiology 1990:72,669-674.
14. Mohamed N., Cynthia Al Pharmacology of muscle relaxants and their antagonist. In Miller RD, editor, Miller anesthesia 6** edition.
15. Perry JJ, Lee JS, Sillberg VA, Wells GA: Rocuronium versus succinylcholine for rapid sequence induction intubation. Cochrane Database Syst Rev 2008, 2: CD002788.
16. Sluga M, Ummenhofer W, Studer W, Siegemund M, Marsch SC: Rocuronium versus succinylcholine for rapid sequence induction of anesthesia and endotracheal intubation: a prospective, randomized trial in emergent cases. Anesth Analg 2005, 101: 1356-1361.
17. G. Scheiber F.C Ribero A Marichat et al: Intubating conditions and onset of action after Rocuronium, Vecuronium and Atracurium in young children. Anesth-Analg 1996:83,320-324.
18. O' Kelly B.P Fiset, C. Meistelman et al: Pharmacokinetics of Rocuronium bromide in paediatric patient. European Journal of Anaesthesiology 1994:11(9), 57-58.
19. Stoddart P.A.: Onset of neuromuscular blockage and intubating conditions one minute after administration of Rocuronium in children. Paediatric anaesthesia, France 1998:8,37-40.
20. J. Viby-Magensan: Dose response relationship and time course of action of Rocuronium in perspective. European journal of Anaesthesiology 1994:11(9),28-32.
21. Singh et al: Comparison of onset time, duration of action and intubating condition achievedwith succinylcholine and Rocuronium. Indian journal of Anaesthesia 2004:48(2), 129-133.
23. Cooper R.,R.k Mirrakhur: comparison of intubating condition after administration of ORG-9426(Rocuronium) and Suxamethonium. B.J.A 1992:69,269-273.
24. Dr. Madhvi Barve (Indian journal of anaesthesia 2002):Assessed intubating condition at 60 seconds and after every 30 seconds later until patient could be intubated with good or excellent condition.
25. Aparna Shukla, Dubey KP, Sharma M.S.N: Comparative evaluation of haemodynamic effects and intubating condition after administration of ORG-9426 and succinylcholine. Indian journal of anaesthesia 2004:48(6), 476-479.
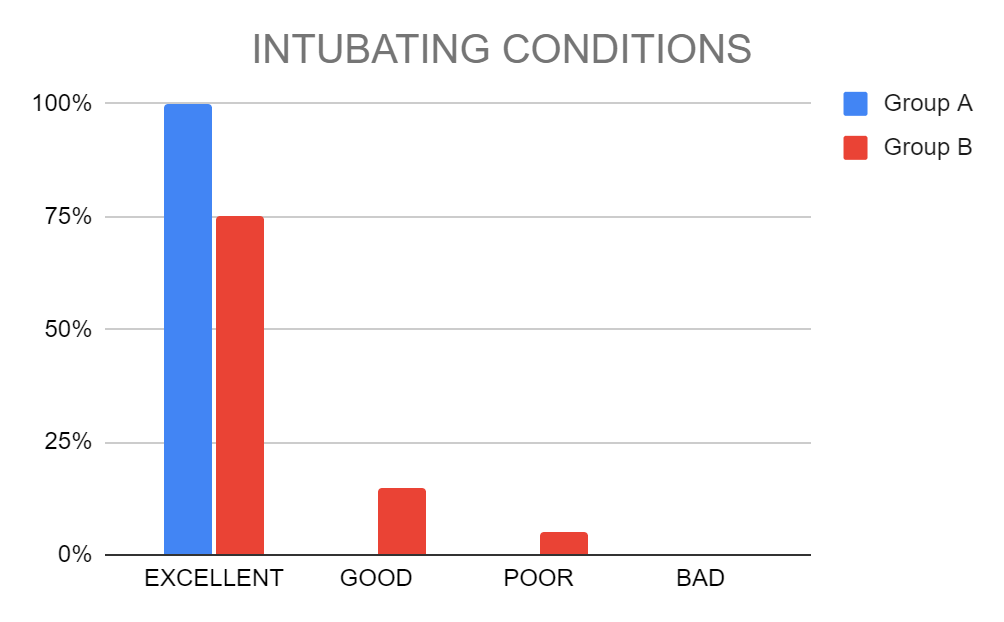
Figure 1
