A Comparative Study on Effect of Bupivacaine and Bupivacaine with Fentanyl in Subarachnoid Block for Cesarean Section
A Comparative Study on Effect of Bupivacaine and Bupivacaine with Fentanyl in Subarachnoid Block for Cesarean Section
Dr. Yagnik P Ramani*1, Dr. Akruti U Patel 2, Dr. Sejal D Shelat 3
1.3rd Year Resident Doctor, Department of Anaesthesiology, Smt. NHL Municipal Medical College, Ellisbridge, Ahemdabad, Gujarat, India.
2.Consultant Anaesthesiologists at Zydus Hospital, Anand, Ahmedabad, Gujarat.
3.Assistant Professor, Department of Anaesthesiology, Smt. NHL Municipal Medical College, Ellisbridge, Ahemdabad, Gujarat, India.
*Correspondence to: Dr. Yagnik P Ramani, 3rd Year Resident Doctor, Department of Anaesthesiology, Smt. NHL Municipal Medical College, Ellisbridge, Ahemdabad, Gujarat, India.
Copyright
© 2024: Dr. Yagnik P Ramani. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 28 July 2024
Published: 13 August 2024
Abstract
Background: Spinal anesthesia is a popular technique and has become the preferred method of anesthesia with minimal complications. Bupivacaine is a commonly used drug for subarachnoid block for caesarean delivery because of less neurotoxicity and Fentanyl is preferred opioid adjuvant with fewer maternal and foetal side effects. This study was planned to observe the usefulness and efficacy of Fentanyl as an adjuvant with Bupivacaine in subarachnoid block for caesarean section.
Materials and Methods: An observational study was carried out among 50 female patients with ASA grade I/II presenting for caesarean section at NHL Medical college, Ahemdabad. Out of 50 women, 25 were received only bupivacaine and another 25 were received bupivacaine with fentanyl as a subarachnoid block. Sensory and motor block were assessed and after the block was achieved, pulse, blood pressure, SpO2, respiratory rate was monitored every two minutes for the first 5 minutes, and every 10 minutes for 1 hour, then every 15 minutes for the next 1 hour.
Results: All the females were belonging to the age group of 18-35 years. Time for sensory regression to S2 level was longer in patients with bupivacaine with fentanyl than patients received only bupivacaine and this was found to be statistically significant. There was no statistically significant difference was observed with regards to onset of sensory and motor block and time for grade 3 to grade 0 between two groups. Duration of effective analgesia was significantly prolonged in patients with bupivacaine with fentanyl. Higher incidence of nausea, vomiting and shivering was found in patients receiving bupivacaine.
Conclusion: Combined effect of Fentanyl Bupivacaine is superior over Bupivacaine alone as Fentanyl reduces the doses of Bupivacaine too.
Keywords: Bupivacaine, Bupivacaine with fentanyl, Subarachnoid block.
A Comparative Study on Effect of Bupivacaine and Bupivacaine with Fentanyl in Subarachnoid Block for Cesarean Section
Introduction
Caesarean section is one of the most common operations in childbearing age of a woman. If the baby is in distress in the later stage of pregnancy, Caesarean section is the way to ensure the safety of baby[1]
Regional anaesthesia has become more widely practiced anaesthetic technique because[2]
1.It is simple to perform, has rapid onset, and low failure rate.
2.Complete analgesia and involves lesser drug doses.
3.Aspiration pneumonia which is the most common complication can be avoided by regional anaesthesia.
4.Better suppression of neuroendocrine stress response and maternal mortality than general anaesthesia[3]
5.Reduce the risk of fetal respiratory suppression induced by the systemic administration of anaesthetics in general anaesthesia.
6.Early feeding and ambulation of mother, also allows her to take care of neonate.
Spinal anaesthesia was first produced by Corning in 1885 and first used deliberately by BIER in 1898.[4] Glucose containing solution for spinal anaesthesia was introduced by A. E. Barker in 1907.[4] Since then hyperbaric solutions are in use for spinal anaesthesia. Resurgence of spinal anaesthesia as a popular technique was possible due to development of small bore needles with pencil point tips and has become the preferred method of anaesthesia.
Bupivacaine hydrochloride an amide type of local anaesthetic, had high potency, slow onset and long duration of action.[5] Bupivacaine is a commonly used drug for subarachnoid block for caesarean delivery because of less neurotoxicity.
Caesarean delivery requires traction of peritoneum and manipulation of intraperitoneal organs, resulting in intraperitoneal visceral pain.[6] Effective postoperative analgesia permits improved mother child bonding, early ambulation and discharge, greater patient satisfaction and early breast feeding.[1]
In 1979, clinical efficacy of intrathecal and epidural opioids used to control the pain following a wide variety of surgical procedures as sole analgesic agents or in combination with low doses of local anaesthetic agents was checked.[4]
Fentanyl citrate is a short acting opioid and has rapid onset of action[5] Intrathecal Fentanyl acts as mu receptor agonist at supraspinal site leading to analgesia that is greater than Morphine and Pethidine. Fentanyl, a lipophilic opioid, after intrathecal administration diffuses into epidural space and subsequently into the plasma suggesting that it acts not only through spinal opioid receptors but also systemically. Such as Fentanyl is a preferred opioid adjuvant. Opioids and local anaesthetics administered together intrathecally have a potent synergistic analgesic effects.[7] Intrathecal opioids enhance analgesia from subtherapeutic doses of local anaesthetic, thus opioids reduce the incidence of higher blocks and local anaesthetic related side effects by reducing their doses.
The present study is to observe the usefulness and efficacy of Fentanyl as an adjuvant with Bupivacaine in subarachnoid block for caesarean section to prevent hypotension and other complications while maintaining prolonged duration of anaesthesia.
Materials and Methods
An observational study was conducted among fifty women presenting for caesarean section belonging to American Society of Anaesthesiologist (ASA) grade I or II.
Study groups of 25 patients each:
Group B (Patients receiving bupivacaine): receiving 1.8 ml of 0.5% injection Bupivacaine hydrochloride (hyperbaric) with 0.4ml of normal saline.
Group BF (Patients receiving bupivacaine with fentanyl): receiving 1.8 ml of 0.5% Bupivacaine hydrochloride with 0.4 ml (20 mcg) of injection Fentanyl citrate.
Total volume of the drug is 2.2ml.
Patients who refused to participate in the study, with foetal abnormality, gross spinal deformity or peripheral neuropathy, coagulation disorder, hypersensitivity to study drugs, history of chronic headache / backache, drug or alcohol abuse, local infection at the site and hemodynamically unstable patients were excluded from the study.
All patients were evaluated preoperatively with detailed history, general and systemic examination. Vital parameters were noted (P, BP, RR, SPO2 at room air). Patients were explained about the procedure and Visual Analogue Score (VAS) for assessment of analgesia. Informed written consent was obtained from each patient. During preoperative preparation patients were nil by mouth overnight and baseline values of vital parameters were noted. Injection ondansetron 4 mg i.v. given as an antiemetic and all patients were routinely catheterized.
Patients are placed in left lateral position, under all strict aseptic and antiseptic precautions after infiltration of the skin with local anaesthetic solution 2 ml of 1% injection lignocaine, lumbar puncture was performed at L2-L3 or L3-L4 space in left lateral position with 23 G quincke spinal needle and after confirming free flow of CSF the study drug was injected and time and vitals at that time were noted. After injecting the study drug, immediately patients were placed in supine position with left tilt. Supplemental oxygen with a face mask was given at the rate of 2L/min. Continuous monitoring of vital parameters was carried out and noted throughout the surgery.
Sensory blockade was assessed by pin prick method and the onset of sensory block, level of highest sensory block level, and the time to attain highest level were noted. Motor block was assessed with use of Bromage scale and its onset of time was noted, onset of time is defined as the Time of grade 0 to reach grade 3 of Bromage scale. Duration of grade 3 of bromage scale was noted and time to recover to grade 0 was noted. After the targeted level of sensory and motor block was achieved, surgery was started and corresponding time and vitals noted. Intra operatively pulse, blood pressure, spo2, respiratory rate were monitored every 2 minutes for the first 5 minutes, and every 10 minutes for 1 hour, then every 15 minutes for the next 1 hour.
Hypotension, Bradycardia, Nausea and vomiting, Respiratory depression, Sedation, Pruritus, Shivering, Urinary retention, Post dural puncture headache (PDPH), Duration of surgery and the level of motor and sensory block was noted. Duration of analgesia was evaluated from the time of spinal injection to the time when the patient had discomfort or pain. Pain was assessed by visual analog score. Inj. Diclofenac Sodium 75 mg i.v. was given as rescue analgesia. Rescue analgesia is defined as interval from time of intrathecal injection to the time of 1st analgesic demand post operatively or when VAS score >5 since it depicts moderate pain. After completion of surgery, patients were transferred to the postoperative room and observed hemodynamic parameters and any side effects or complications in the postoperative period for 24 hrs.
Data entry was done in Microsoft Office Excel 2016, and analysis was done using the software package Epi Info (version 7.2.2.6) from CDC, Atlanta, U.S.A. Appropriate statistical tests such as unpaired t test was used. The study was approved by the institutional ethics committee.
Results
Perioperative mean blood pressure was recorded at different time intervals in both the groups. The difference of blood pressure between two groups were not found to be statistically significant (P>0.05) [Figure 1].
Fifty pregnant mothers who underwent cesarean delivery under spinal anesthesia during the study period was included. Of these patients, 25 patients were given bupivacaine with fentanyl and 25 patients were given bupivacaine alone. Mean age of both thaving a mean age of 26 years in both groups. Average height of all the patients were around 152 cm and weight was 68 kg with a standard deviation of 5 cm and 6 kg respectively. There was no statistically significant difference among the groups with socio-demographic data [Table 1].
Time to onset of sensory block was statistically not significant in both groups (P >0.05). Duration of regression of sensory block to S2 dermatome was higher in group BF (patients receiving bupivacaine with fentanyl) patients as compared to group B (patients receiving bupivacaine) and it was found to be statistically significant (P<0.0001). There was no significant difference in time of onset and time from grade 3 to grade 0 motor block between the two groups by bromage scale (P>0.05) [Table 2].
Heart rate was recorded pre-operatively in both the groups and then at different time intervals and this was decreased in both groups as compared to baseline value. The difference in decreasing heart rate between two groups were not found to be statistically significant (P>0.05) [Table 3].
In group B, maximum and minimum time for first rescue analgesia was 190 minutes and 166 minutes respectively. Maximum time was 228 minutes and minimum time was 200 minutes required for first rescue analgesia in group BF. Mean time with standard deviation was more among patients received BF as compared to patients received B; Mean ± SD among group BF was 213.36 ± 19.1 and among group B was 178.56 ± 6.58. This difference in time for first rescue analgesia between two groups was found to be statistically significant (P<0.001).
After giving bupivacaine, 4 patients had hypotension, 4 had nausea and vomiting, 3 had shivering and 1 had bradycardia intraoperatively. Those patients who received bupivacaine with fentanyl, 1 had hypotension and 1 had pruritus intraoperatively. Intraoperative complications are more in group B than group BF.
Figure 1: Perioperative mean blood pressure (mmHg) at different time intervals of patients underwent elective caesarean section under spinal anesthesia
Figure 2: Perioperative mean heart rate (per min) at different time intervals of patients underwent elective caesarean section under spinal anesthesia
*Group B - Patients receiving bupivacaine, Group BF – Patients receiving bupivacaine with fentanyl
|
Variables |
Group- B |
Group-BF |
P value |
|
No. of patient |
25 |
25 |
|
|
Age (years) (Mean ± SD) |
26.28 ± 4.36 |
26.76 ± 2.99 |
> 0.05 |
|
Height(cm) (Mean ± SD) |
152.52 ± 4.84 |
153.4 ± 6.4 |
> 0.05 |
|
Weight(kg) (Mean ± SD) |
68.88 ± 6.20 |
67 ± 6.60 |
> 0.05 |
|
Duration of surgery (min) |
59.76 ± 5.768 |
62.72 ± 5.601 |
> 0.05 |
|
ASA grade I |
17 (68%) |
|
|
|
ASA grade II |
8 (32%) |
|
|
Table 1: Demographic characteristics of patients undergoing elective caesarean section with spinal anesthesia (n=50)
|
Characteristics |
Group B (Mean ± SD) |
Group BF (Mean ± SD) |
P value |
|
Time of onset of sensory block (min) |
4.12 ± 0.881 |
4.4 ± 0.645 |
> 0.05 |
|
Time for sensory regression to S2 level (min) |
158 .96 ± 4.16 |
178.48 ± 3.17 |
<0.001 |
|
Onset of grade 3 motor block (min) |
6 ± 0.957 |
6.32 ± 0.748 |
> 0.05 |
|
Time from grade 3 to grade 0 motor block (min) |
163.36 ± 6.76 |
164.88 ± 2.86 |
> 0.05 |
Discussion
Regional anaesthesia is more popular over GA in obstetric patients due to less complications and mortality. There is always a chance of higher levels of block or toxicity of Local anaesthesia, the risk being higher in pregnant patients than non-pregnant patients. Recent trends in obstetric anaesthesia has shown an increased usage of intrathecal opioids as an adjuvant with local anaesthetic drugs in regional anaesthetics because it improves the quality of intra operative analgesia and also provides postoperative pain relief for longer duration. This study was a comparison of subarachnoid block with Bupivacaine and Bupivacaine with Fentanyl for caesarean section.
Group B: intrathecal hyperbaric Bupivacaine hydrochloride 0.5% 9mg (1.8ml) + 0.4 ml of NS
Group BF: intrathecal hyperbaric Bupivacaine hydrochloride 0.5% 9mg (1.8ml) + 20mcg of Fentanyl citrate (0.4ml)
In present study, demographic data (age, height, weight, ASA grade and duration of surgery) of both the groups were compared and there was no significant difference in both groups (P>0.05).
There was no statistically significant difference in both groups regarding the onset of sensory blockage in this study as it was 4.12± 0.881 min in group B and 4.4+ 0.645 min in group BF (P>0.05). Biswas BN, Rudra A et al in 2002 studied 12.5 mcg Fentanyl with 10 mg Bupivacaine intrathecally and found no statistical significance in sensory onset in both groups.[8] Thapa SG et al in 2014 studied the effect of intrathecal Fentanyl 20 mcg as an adjuvant to Bupivacaine in elective caesarean section and concluded there was no statistical significance in sensory onset in both groups.[6] Yesuf KA et al in 2017 studied the analgesic effect of intrathecal Fentanyl as an adjuvant with Bupivacaine to spinal anaesthesia in comparison with Bupivacaine alone for emergency caesarean section and found no statistical significance in onset of sensory block.[1]
In present study there was a statistically highly significant difference that was present regarding duration of regression of sensory blockade to S2 dermatome and it was 158.96±4.16 min in Group B and 178.48± 3.177 min in Group BF. Gupta R et al in 2011 studied intrathecal Fentanyl 25 mcg with Bupivacaine and found that the time of regression of sensory block to S1 was 187±12.3 min.[9] Biswas BN, Rudra A et al observed in their study that time for sensory regression to L1 from highest sensory level (min) was 116±14.39 min in control group and 151±7.33 min in Fentanyl group.[8] Sheikh F, Ahmed M, Ommid M et al also found significant difference in time taken for sensory regression to T12 (162.6± 10.5 min in control group compared to 209.9 ±11.6 min in study group) in their study of 12.5mcg with 10mg of Bupivacaine.[10]
In present study, the onset time of motor block was 6 ± 0.957 min in group B and 6.32± 0.748 min in group BF. So there was no statistical significance in both groups (P>0.05). Yesuf KA et al studied Fentanyl as an adjuvant with Bupivacaine in spinal anaesthesia in emergency caesarean section and found no statistical significance in both groups.[1] Gopichand K, Suresh T et al (2016) found no significant difference in onset of motor block in both groups.[5] Sheikh F, Ahmed M et al (2013) studied 12.5 mcg Fentanyl with 10 mg Bupivacaine in caesarean section of patients having PIH and concluded onset of motor block were comparable and non-significant in both groups.[10]
In this study, time to grade 0 from grade 3 was not statistically significant as it was 163.36 ±6.76 min in group B and 164.88±2.86 min in group BF (P>0.05). Choi DH, Ahn HJ et al studied 10 mcg Fentanyl adjuvant to 3 different doses of Bupivacaine intrathecally in caesarean section and found motor recovery time did not change with additional Fentanyl.[11] Biswas BN, Rudra A et al studied 12.5mcg of Fentanyl with 10 mg of hyperbaric Bupivacaine and observed that duration of motor block was comparable in both groups. There was no statistically significance among them.[8] Sheikh F, Ahmed M et al in 2013 studied 12.5 mcg Fentanyl with 10mg Bupivacaine in caesarean section of patients having PIH and observed that time to grade 0 from grade 3 motor block was not significant in Fentanyl group (170±13.9min) as compared to Bupivacaine alone group (170± 19.7min).[10]
In present study, intraoperative and postoperative pulse rate and blood pressure were recorded in both groups and association of this parameters were not statistically significant (P>0.05). David B et al, 1997 demonstrated better haemodynamic condition with low dose Bupivacaine with Fentanyl in spinal anaesthesia for caesarean section.[7] Sheikh F, Ahmed M et al in 2013 studied 12.5 mcg Fentanyl with 10mg Bupivacaine in caesarean section of patients having PIH and observed that there were no significant changes in hemodynamic parameter in both groups. In group B and group BF fall in BP were less than 20% from baseline value.[10]
In our study, hypotension was seen in 4(16%) patients in group B and 1 (4%) patients in group BF and bradycardia was seen in 1(4%) patients in group B and 0 (0%) patients in group BF.
Effective analgesia is defined as time from subarachnoid injection to 1st dose of postoperative analgesic.[6] In present study, duration of effective analgesia was prolonged significantly in group BF (213.36 ± 19.1min) as compared to group B (178.56 ± 6.58min) (P<0.001). So effective analgesia time in group BF was highly significant as compared to group B. Sheikh F, Ahmed M[10] et al in 2013 studied 12.5 mcg Fentanyl with 10mg Bupivacaine in caesarean section of patients having PIH and observed that time from injection to first rescue analgesic was significantly prolonged in Fentanyl group (326.1+50 min) as compared to Bupivacaine alone group (234.7+32.9 min). Dr. B. N. Biswas[8] et al studied 12.5 mcg Fentanyl as an adjuvant to 10mg Bupivacaine in spinal anesthesia in caesarean section and found complete analgesia lasted longer in group B (Fentanyl group) for 183 ± 9 min as compared to group A (control group) 129 ± 9.5 min.
In this study, incidence of nausea and vomiting was 16% (4 patients) in group B and it was 0% (0 patients) in group BF. Dr B N Biswas, Dr A Rudra[8] et al reported the incidence of nausea and vomiting in 8 patients(40%) in Bupivacaine group as compared to 1 patient(5%) in Fentanyl group. In this study, incidence of shivering was 12% (3 patients) in group B compared to 0% (0 patient) in group BF. Dr B N Biswas, Dr A Rudra[8] et al found the incidence of shivering in 4 patients(20%) in Bupivacaine group as compared to 1 patient(5%) in Fentanyl group. Incidence of pruritus was 4% (1 patients) in group BF (but did not require any treatment) while none of the patients from group B developed pruritus. Dr B N Biswas[8] et al found no pruritus in any group with Fentanyl intrathecally in 40 pregnant patients undergoing caesarean section.
Conclusion
The addition of 20mcg Fentanyl as adjuvant to 1.8ml Bupivacaine intrathecally provides good hemodynamic stability, better surgical analgesia, prolongs the duration of analgesia post operatively, reduce severity of pain as well as total analgesia consumption without an effect on the mother and fetus.
References
1. Yesuf KA, Gebremedhin EG and Melkie TB ., Analgesic effect of intrathecal Fentanyl as an Adjuvant to Spinal Anaesthesia in comparison with Spinal Anaesthesia with Bupivacaine Only for mothers delivered by emergency caesarean section. Journal of anaesthesia & Critical care, Volume 7 Issue 5- 2017.
2. Morgan and Mikhail’s, 5th edition, section IV: regional and pain management,chapter 45:spinal, epidural and caudal blocks.
3. Morgan and Mikhil’s clinical anaesthesiology, 5th edition, chapter 41, obstetric anaesthesia,page no. 843.
4. T K Agasti, Textbook of Anaesthesia for postgraduate 1st edition:2011, chapter 24- spinal, epidural and caudal anaesthesia or central neuraxial block. Page no.702 to 740.
5. Gopichand K, Suresh T., Effects Fentanyl on hyperbaric Bupivacaine in spinal anaesthesia for Caesarean section, JMSCR Volume 04, Issue 08, Page 11714- 11719 August 2016.
6. S.Gauchan, C. Thapa et al: Effects of intrathecal Fentanyl as an adjuvant to hyperbaric Bupivacaine in spinal anaesthesia for elective caesarean section. Nepal Med Coll J 2013; 15(3) :156-159.
7. B Ben David, E Solomon, H Levin, H Admoni, intrathecal Fentanyl with small dose dilute Bupivacaine; better anesthesia without prolonging recovery., anesth analg, 1997 sep;85(3): 560-5.
8. B.N.Biswas et al: Intrathecal Fentanyl with hyperbaric Bupivacaine improves analgesia during caesarean delivery : Indian journal of Anaesthesia 2002 ; 46(6) 469- 472
9. Rajni Gupta, Reetu Verma,Monica Kohli, A Comparative study of intrathecal dexmedetomidine and Fentanyl as adjuvants to Bupivacaine., Journal of Anaesthesia Clinical Pharmacology, 2011,volume 27,issue 3, 339-343.
10. F Sheikh, M Ahmed, M Ommid, S Gurcoo, N Shakoor., Comparative evaluation of low dose hyperbaric Bupivacaine with or without Fentanyl in spinal anaesthesia for caesarean section in patients with pregnancy induced hypertension., The internet journal of anaesthesiology . 2013 Volume 31 number 1.
11. Choi DH, Ahn HJ, Kim MH. Bupivacaine-sparing effect of Fentanyl in spinal anesthesia for caesarean delivery.reg Anesth Pain Med.2000 May- jun;25(3):240-5.
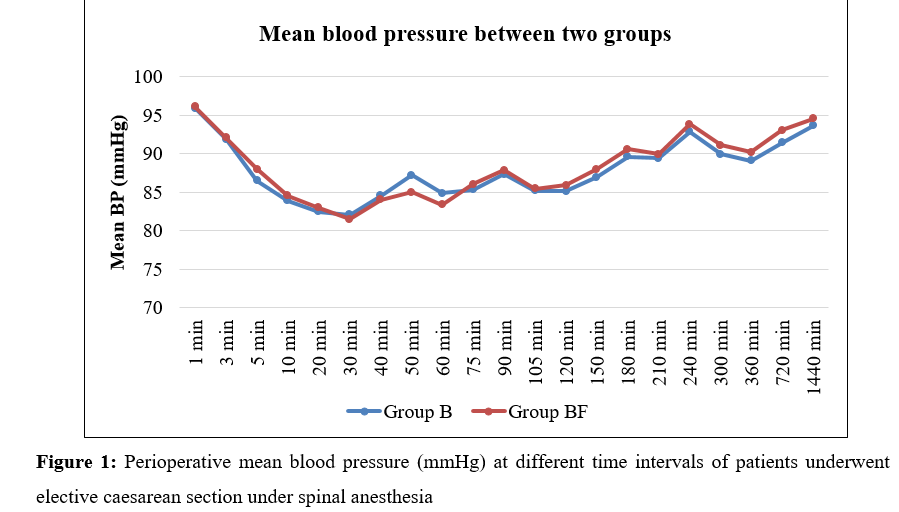
Figure 1
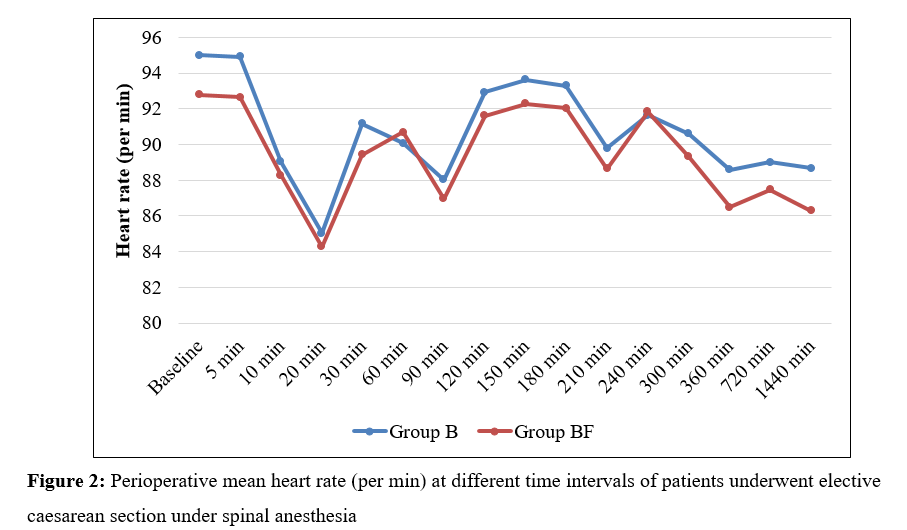
Figure 2
