Comparision of Intraperitoneal Instillation of Bupivacaine, Ropivacaine and Saline for Postoperative Pain Relief after Laparoscopic Intraabdominal Surgeries
Comparision of Intraperitoneal Instillation of Bupivacaine, Ropivacaine and Saline for Postoperative Pain Relief after Laparoscopic Intraabdominal Surgeries
Dr. Vandanaba L. Rathod 1*, Dr. Jagruti R. Satasia2
1.R3, Department of Anaesthesia, SCL General Hospital and Smt. NHL Medical College, Ahmedabad, Gujarat.
2.Associate Professor, Department of Anaesthesia, SCL General Hospital and Smt. NHL Medical College, Ahmedabad, Gujarat.
*Correspondence to: Dr. Vandanaba L. Rathod, R3, Department of Anaesthesia, SCL General Hospital and Smt. NHL Medical College, Ahmedabad, Gujarat.
Copyright
© 2024: Dr. Vandanaba L. Rathod. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 07 August 2024
Published: 24 August 2024
Abstract
Introduction: Laparoscopic surgeries involve insufflation of gas usually carbon dioxide into peritoneal cavity producing a pneumoperitoneum. Although minimal invasive surgery is characterized by reduced pain but it is not painless. Patients undergoing laparoscopic surgery suffer considerable pain on the day of surgery frequently requiring narcotic analgesia. Intraperitoneal instillation of local anaesthetic in combination with General Anaesthesia for postoperative analagesia is a part of multimodal approach for pain control.
Aim & Objectives: To evaluate the efficacy of two different local anaesthetic Bupivacaine vs Ropivacaine in terms of
1. Duration of postoperative pain relief.
2. Need of rescue Analgesia in postoperative period.
3. Any side effects or complications.
Methodology: A Prospective, randomised, comparative case control study conducted on 60 Patients undergoing laparoscopic abdominal surgeries.
INCLUSION CRITERIA:
1. Adult patient of either sex
2. Age between 18 to 60 years
3. ASA grade I/ II
4. Patient posted for elective laparoscopic surgeries
5. Patient who had given informed written consent
EXCLUSION CRITERIA:
1. Patient not satisfying above inclusion criteria
2. ASA physical status III, IV AND V
3. Local anaesthetic allergy
4. Patients who refused
5. Pregnancy
6. Any laparoscopic surgery converted to open surgery
After explaining and taking informed written consent, pre-operative preparation were done, all drugs and instruments kept ready for cardio -pulmonary resuscitation. IV line secured. Non-invasive monitors and Etco2 monitor was applied. Before induction pre-operative vitals noted. General Anesthesia given.
The patients were devided into three comparative study groups
GROUP B: Bupivacaine group
GROUP R: Ropivacaine Group
GROUP C: Control Group
Results:
Ropivacaine provided adequate Analgesia of 11.5 hours compared to Bupivacaine which provided for 8 hours and control group which provided Analgesia for 5.5 hours. Ropivacaine provide Analgesia for longer duration as compared to other two groups.
Conclusion:
Ropivacaine provide most profound and prolonged analgesia as compared to Bupivacaine.
This technique of providing postoperative analagesia is simple, safe, effective and improves postoperative recovery profile of the patient.
Comparision of Intraperitoneal Instillation of Bupivacaine, Ropivacaine and Saline for Postoperative Pain Relief after Laparoscopic Intraabdominal Surgeries
Introduction
Laparoscopic surgeries involve insufflation of gas usually carbon dioxide into peritoneal cavity producing a pneumoperitoneum. Although Minimal Invasive Surgery is characterized by reduced pain but it is not painless. Patients undergoing laparoscopic surgery suffer considerable pain on the day of surgery frequently requiring analgesia1,2
Uncontrolled postoperative pain has an adverse sequel of delayed resumption of normal pulmonary function, restriction of mobility (thus contributing to thromboembolic complications), nausea and vomiting, increase in the systemic vascular resistance, cardiac work, and myocardial oxygen consumption through an increase in the catecholamine release induced by the stress response.3
Adequacy of postoperative pain control is one of the most important factors in determining when a patient can be safely discharged from surgical facility and has a major influence on the patient’s ability to resume their normal activities of daily living.4
Although traditionally the mainstay of postoperative analgesia is opioid based, increasingly more evidence exists to support a multimodal approach with the intent to reduce opioid side effects (such as nausea and paralytic ileus) and improve pain scores.5 Intraperitoneal instillation of local anaesthetic in combination with General Anesthesia for postoperative Analgesia is a part of multimodal approach for pain control.
Aim and Objectives
Aim of the study is to evaluate the efficacy of intraperitoneal instillation of local anesthetics for post operative pain relief after laparoscopic abdominal surgeries and compare the efficacy of two different local anesthetics Bupivacaine vs Ropivacaine in terms of –
1. Duration of postoperative pain relief.
2. Need of rescue Analgesia in postoperative period.
3. Any side effects or complications
Materials and Methods
A prospective, randomized clinical study was conducted on 60 subjects undergoing laparoscopic abdominal surgery. Patients were divided into three comparative study groups – Group B (Bupivacaine), Group R (Ropivacaine) and Group C (control).
INCLUSION CRITERIA:
1. Adult patient of either sex
2. Age between 18 to 60 years
3. ASA grade I/ II
4. Patient posted for elective laparoscopic surgeries
5. Patient who had given informed written consent
EXCLUSION CRITERIA:
1. Patient not satisfying above inclusion criteria
2. ASA physical status III, IV AND V
3. Local anaesthetic allergy
4. Patients who refused
5. Pregnancy
6. Any laparoscopic surgery converted to open surgery
Detailed history and preoperative assessment was carried out before operation. A detailed general as well as systemic examination was done to rule out any major systemic illness. An informed consent was obtained from all the patients. Enrolled patients were explained about the use of visual analogue scale employed in this study.
All patients received Tab.alprazolam 0.5 mg orally and Tab.ranitidine 150 mg orally night before surgery. Preoperatively patients were inquired about the NBM status. In pre-operative room pulse rate, blood pressure, respiratory rate and oxygen saturation were noted. Thereafter patients were shifted into the theatre. Monitors were attached (ECG, NIBP, PR, ETCO2 and SPO2). Basal parameters were noted. Local anaesthetic test dose was given to confirm the absence of allergic reactions.
Patients were premedicated with inj. Glycopyrrolate 0.2 mg IV and inj. Fentanyl 2 μg/kg IV, pre oxygenated with 100% O2 for 3min with bag and mask. Induction was carried out with inj. Propofol 2 mg/kg IV and intubated with an appropriate size endotracheal tube after inj. succinylcholine 2 mg/kg IV was effective. Nasogastric tube was introduced and the patient was placed in a head up position in order to provide optimum conditions for laparoscopic surgery. General anaesthesia was maintained by controlled mechanical ventilation with a sevoflurane and oxygen. Muscle relaxation was achieved with atracurium 0.5mg/kg IV initially and repeated every 20 minutes thereafter (0.1mg/kg IV). No extra dose of analgesia was given intra operatively. After skin incision 11mm trocar introduced via umbilical port, abdomen inflated with CO2 1 lit/min with IAP pressure kept around 12-14mmHg in all patients.
After the procedure gets over, abdomen was thoroughly washed to remove the blood clots and debris. Inj. Bupivacaine (preservative free) 0.5% 20 ml, Inj. Ropivacaine (preservative free) 0.5% 20 ml ,0.9% normal saline 20ml is instilled intra peritoneally under vision. After the removal of trocar, CO2 gas was completely evacuated from the abdomen. Patients were kept in trendelenburg position for 10 minutes. If abdominal drain was present it was clamped. 4ml of 2% Lignocaine was infiltrated into the skin. During the surgery ETCO2 value was maintained between 25 to 35 mm hg. At the end of surgery, skin closure was done. And only after adequate spontaneous ventilation and neuromuscular recovery achieved, patients were reversed with inj. Glycopyrrolate 0.4 mg IV and inj. Neostigmine 0.05 mg/kg IV and extubated.
Post operatively the patients were assessed for pain utilizing VAS. The time of arrival in the postoperative ward was defined as zero hour postoperatively. Pain intensity was measured at fixed time interval postoperatively at 0, 2, 4, 6, 8, 12 and 24 hours. The patients were also enquired about nausea, vomiting and shoulder tip pain.
VAS - visual analogue scale consists of a 10 cm scale representing varying intensity of pain from 0 (no pain) to 10 (worst pain).
Inj. tramadol 50 mg i.v given as the rescue analgesia whenever the VAS score were more than 4. Total dose of tramadol required was noted. Time of the first rescue analgesic requirement was noted. The occurrence of nausea and/or vomiting was assessed.
Statistical analysis was done with statistical package for social sciences (SPSS for windows, version 15)
- ANOVA test used for statistical analysis.
- Results expressed as mean and standard deviation.
- A ‘p’ value of less than 0.05 was considered significant.
Observation and Results:
This prospective study was carried out in 60 ASA I and II patients posted for laparoscopic intra abdominal surgeries under general anaesthesia. The study population was randomly allocated into three groups, 20 patients in each group.
Group B – Bupivacaine group - patients received 20 ml 0.5% Bupivacaine intraperitoneally.
Group R – Ropivacaine group - patients received 20 ml 0.5% Ropivacaine intraperitoneally.
Group C – control group - patients received 20 ml of 0.9% saline intraperitoneally.
Table 1 - Demographic profile: Age, sex, weight and height distribution of patients
|
|
Group B |
Group R |
Group C |
P value |
|||
|
|
Mean |
SD |
Mean |
SD |
Mean |
SD |
|
|
Age (years) |
37.05 |
13.70 |
33.25 |
9.83 |
41.55 |
9.47 |
0.071 |
|
Height(cm) |
158.15 |
5.508 |
158.65 |
5.091 |
156 |
5.099 |
0.244 |
|
Weight (kg) |
59.70 |
5.068 |
59.95 |
5.633 |
58.45 |
4.999 |
0.627 |
Table 2 – Mean Visual Analogue Scale (VAS) score after intraperitoneal instillation
|
|
Group B |
Group R |
Group C |
P value |
|||
|
|
Mean |
SD |
Mean |
SD |
Mean |
SD |
|
|
0 hour |
1.25 |
0.850 |
0.45 |
0.686 |
1.65 |
0.745 |
0.000 |
|
2 hour |
2.05 |
1.050 |
1.55 |
0.887 |
3.3 |
1.174 |
0.000 |
|
4 hour |
2.8 |
0.695 |
2.2 |
1.196 |
4.15 |
0.988 |
0.000 |
|
6 hour |
3.95 |
1.394 |
2.8 |
1.321 |
4.45 |
1.356 |
0.001 |
|
8 hour |
4.55 |
0.998 |
3.9 |
1.119 |
4.45 |
0.944 |
0.105 |
|
12 hour |
3.85 |
1.225 |
3.8 |
1.239 |
4.55 |
1.276 |
0.113 |
|
24 hour |
3.5 |
1.277 |
3.8 |
1.239 |
4.25 |
1.409 |
0.199 |
Table 3 –Rescue analgesic timing (hour)
|
Group |
No. of patients |
Mean |
SD |
P value |
|
Group B |
20 |
8 |
2.190 |
0.000 |
|
Group R |
20 |
11.5 |
5.391 |
|
|
Group C |
20 |
5.5 |
2.417 |
Table 4 – Post operative analgesic consumption in 24 hours
|
Group |
No. of patients |
Mean |
SD |
P value |
|
Group B |
20 |
102.94 |
48.317 |
0.0002 |
|
Group R |
20 |
84.375 |
43.660 |
|
|
Group C |
20 |
147.5 |
41.278 |
|
Group |
Nausea and vomiting |
P value |
|||
|
YES |
NO |
||||
|
Total |
% |
Total |
% |
||
|
Group B |
1 |
5 |
19 |
95 |
0.001 |
|
Group R |
1 |
5 |
19 |
95 |
|
|
Group C |
5 |
25 |
15 |
75 |
|
Discussion
Pain after laparoscopic surgery is multifactorial and comprises of several components. The parietal pain is due to placement of trocars through the abdominal wall. The visceral pain is because of intraperitoneal dissection and insufflation of CO2 resulting in distension of abdominal wall and prolonged elevation of diaphragm leading to shoulder tip pain.1,6,7
Postoperative pain is the main factor delaying discharge of patients undergoing day-care procedures and hence adding to hospital stay. The techniques that can be used for providing pain relief in laparoscopic surgeries include surgery under subarachnoid block, parental opioids and NSAIDs, Instillation of local anaesthetics etc.
Our study was done to compare the analgesic efficacy of Bupivacaine and Ropivacaine, which were instilled intraperitoneally during laparoscopic intra abdominal surgery, with a control group.
Donatsky AM et al.9 conducted a systematic review to study the role of intraperitoneal saline in prevention of postoperative pain in laparoscopic cholecystectomy. Their findings also support the analgesic action of normal saline in the form of intraperitoneal instillation. Thus, we compared the effect of intraperitoneal local anaesthetic drugs with normal saline.
In our study we compared the mean VAS score at different time intervals after intraperitoneal instillation among the three groups. There was no statistically significant difference in the mean VAS score of bupivacaine and ropivacaine group during first 4 hours but at sixth hour there was statistically significant difference in the VAS score between bupivacaine (mean VAS – 3.95) and ropivacaine group (mean VAS – 2.8) with p=0.01. Bupivacaine group had higher VAS score and pain was perceived earlier in bupivacaine group requiring additional analgesia.
Rakesh Babu et al10 compared low dose ropivacaine 0.20% with bupivacaine 0.25% intraperitoneally. The difference in the VAS scores of bupivacaine and ropivacaine group at the four time points (0, 4, 8 and 12 hour) across 12 hour time period was not significant p= 0.702. There was significant reduction in VAS scores over the 12 hour period in both groups.In our study it was found that the total dose of opioid required in the post operative period was significantly less in both Bupivacaine and Ropivacaine group, when compared to the control group. Out of these two groups, Ropivacaine group needed less Tramadol 84.37 ± 43.66mg, when compared with Bupivacaine group which needed 102.94 ± 48.31 mg, though the difference was found to be statistically insignificant(p>0.05). But the saline group needed 147.5±41.27 mg Tramadol, which was statistically significant (p<0.05). This difference in the rescue analgesic requirement closely correlates with the study done by Tae Han kim et al 11 where the total dose of Fentanyl consumed in Ropivacaine group was 367 ± 85.88 μg over 48 hour via PCA when compared to535 ± 100.29 μg in control group. This was statistically significant with a p value of<0.001.
Bhardwaj et al 12 conducted study in patients undergoing laparoscopic cholecystectomy. He instilled 20 ml 0.5% bupivacaine only at the end of surgery in the Trendelenburg position. Post operatively they assessed for vital signs (heart rate, blood pressure and respiratory rate), pain scores (VAS, VRS and shoulder pain) and analgesic consumption. They found that it reduced post operative cholecystectomy pain and analgesic consumption.
In our study intraperitoneal instillation of Bupivacaine or Ropivacaine at the end of the surgery provided analgesia for 8 ± 2.19 hours and 11.5± 5.39 hours respectively when compared with saline group which was about 5.5± 2.41 hours, which was found to be statistically significant.
Radhe Sharan et al13 in their study on comparison of intraperitoneal ropivacaine and bupivacaine for postoperative analgesia had similar results showing that the duration of analgesia with ropivacaine group was 162.22±124.16 mins which was greater than bupivacaine group 150.00± 86.40 mins. Though the duration of analgesia provided by both the groups were comparable.
In our study there was no significant hemodynamic changes noted. PR, BP,RR were maintained within 20% of the normal limit through out the study. Canankucuk14 and coworkers showed there was no significant change in the hemodynamics during the study which was similar to our study.
One of the common cause of PONV is the use of opioids for postoperative pain relief.
In our study the incidence of nausea and vomiting was 5% among ropivacaine and bupivacaine group when compared with control group 25% which was clinically significant with p=0.001.
Andrei et al15 in their study compared the post operative vomiting in the patients who received Bupivacaine, Ropivacaine intraperitoneally. They used 4 point scale for evaluation. Compared with control group (1.11), bupivacaine (0.41) and Ropivacaine (0.48) group experienced less vomiting. Antiemetic treatment was needed only 10% Bupivacaine group and 15% in Ropivacaine group compared with saline group which was about 43%.
Local anaesthetics are associated with toxicity which is dose related. Intraperitoneal instillation of 100mg of bupivacaine did not result in toxic plasma concentration30, as also 300mg31The maximal tolerated dose before manifestation of central nervous system toxicity is 12% to 25%32,33. Based on these studies we conducted our study with 0.5% bupivacaine and 0.5% ropivacaine. In our study no significant complications were noted like seizure and allergic reaction among the three groups. Sunil Chiruvella et al16 also had similar results where they found no significant incidence of complications while using intraperitoneal local anaesthetics.
Conclusion
This study concludes that intraperitoneal instillation of local anaesthetic solution in laparoscopic abdominal surgeries provides effective postoperative analgesia. Ropivacaine provides a more profound and prolonged analgesia as compared to bupivacaine.
This technique of providing postoperative analgesia is simple, safe, effective and improves the postoperative recovery profile of the patient.
References
1. Pain in Laparoscopy. Review article by J.I.Alexander , British Journal of Anaesthesia. 1997 ; 79 ; 369 -378
2. Laparoscopic abdominal surgery by Mandy Perrin FRCA, Anthony Fletcher FRCA, , British Journal ofAnaesthesia 2004.
3. Rawal N, Allvin R, Amilon A. Postoperative analgesia at home after ambulatory hand surgery: a controlled comparison of tramadol, metamizol and paracetamol. AnesthAnalg 2001;92: 347–51,.
4. Kehlet H, Dahl JB. Anesthesia, surgery and challenges in postoperative recovery. Lancet 2003;362: 1921–8.
5. Christina Cellini, MD, Division ofColorectal Surgery, Department of Surgery, University of RochesterMedical Center, 601 Elmwood Ave, Box SURG, Rochester, NY 14642
6. ANJ journal of surgery.The Royal Australian college of surgeon.Arman kahoker, Taricsammour,Mattiassoop,Volume 81,Issue 4
7. Korell M, Schmaus F. Pain intensity following laparoscopy. SurgLaparEndos.1996;6: 375-379.
8. Sharp JR, Pierson WP. Comparison of CO2 and N2O induced discomfort during peritoneoscopy under local anaesthesia. Gastroenterology.1982; 82: 453-456.
9. Donatsky AM, Bjerrum F, Gögenur I. Intraperitoneal instillation of saline and local anaesthesia for prevention of shoulder pain after laparoscopic cholecystectomy: a systematic review. SurgEndosc. 2013;27(7):2283–92.
10. Rakesh Babu, Prithi Jain, Lulu Sherif, intraperitoneal instillation of ropivacaine Vs bupivacaine for postoperative pain relief in laparoscopic cholecystectomy; International journal of health sciences and research Vol.3, issue: 12; December 2013
11. Tae Han kim, Hyun Kang. Intraperitoneal Ropivacaine Instillation for Postoperative Pain Relief after Laparoscopic Cholecystectomy, Department of Anaesthesiology and painMedicine, College of Medicine, Chung-Ang University, 224-1, Departments of Surgery and Anaesthesiology and Pain Medicine, College of Medicine,Chung-Ang University, Seoul, Department of Surgery, Kyungpook National University Hospital, School of Medicine, Kyungpook National University, Daegu.
12. Bharadwaj N, SharmaV, Chari P. Intraperitoneal bupivacaine instillation for postoperative pain relief after laparoscopic cholecystectomy. Indian J.Anaesth.2002;46(1):49-52.
13. Sharan R, Singh M, Kataria AP, Jyoti K, Jarewal V,Kadian R. Intraperitoneal instillation of bupivacaine and ropivacaine forpostoperative analgesia in laparoscopiccholecystectomy. Anesth EssaysRes 2018;12:377-80.
14. N. Malhotra, K.K. Roy, C. Chanana, S. Kumar: Post-Operative Pain Relief After Operative Gynecological Laparoscopic Procedures With Intraperitoneal Bupivacaine. The Internet Journal of Gynecology and Obstetrics.2006 Volume 5 Number 2. DOI: 10.5580/208c
15. Goldstein A, Grimault P, Henique A, Keller M, Fortin A, DaraiE. Preventing postoperative pain by local anesthetic instillation after laparoscopic gynecologic surgery: a placebo-controlled comparison of bupivacaine and ropivacaine. Departments of Anesthesiology and Gynecology, Hotel-Dieu Hospital Paris, PMID:10910857.
16. Sunil Chiruvella, Srinivasa Rao Nallam. Intraperitoneal instillation of ropivacaine plus dexmedetomidine for pain relief after laparoscopic hysterectomy; Journal of Dr. NTR University of Health Sciences, Vol. 5, No. 2, April 2016, pp. 93-97.
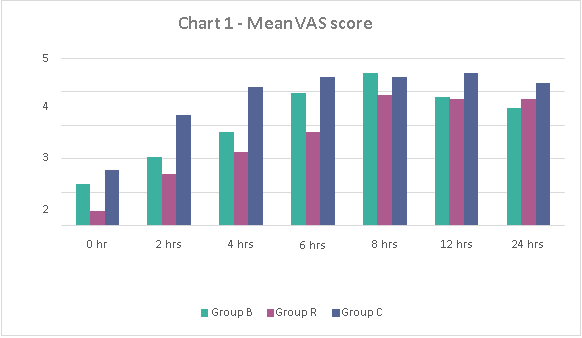
Figure 1
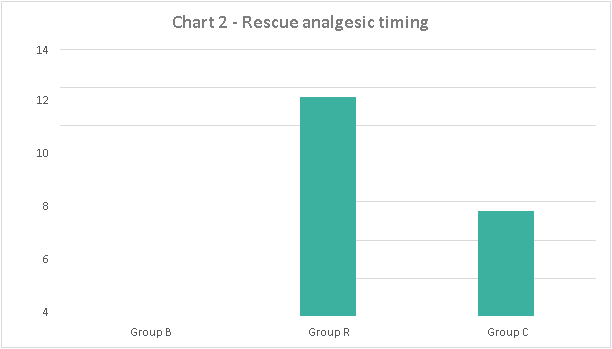
Figure 2
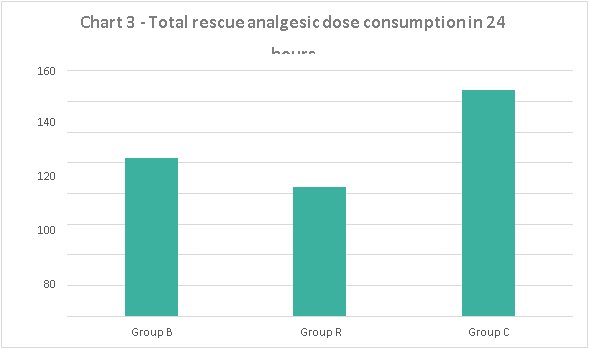
Figure 3
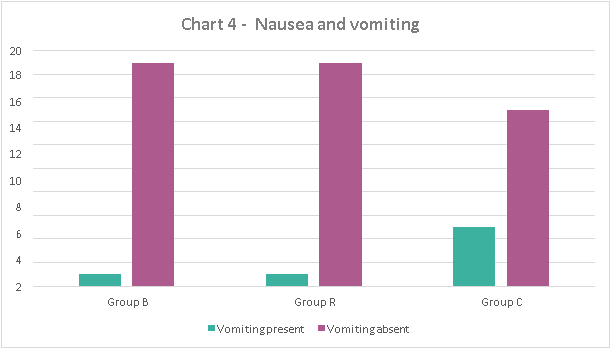
Figure 4
