Analyzing the Structural, Flowmetric, and Functional Effects of using a 532-nm Argon Laser for Panretinal Photocoagulation in Diabetic Retinopathy as Opposed to a 577-nm Pattern Scanning Laser
Analyzing the Structural, Flowmetric, and Functional Effects of using a 532-nm Argon Laser for Panretinal Photocoagulation in Diabetic Retinopathy as Opposed to a 577-nm Pattern Scanning Laser
Ahmed Shabana*
*Correspondence to: Ahmed Shabana, Ophthalmology Specialist, Al Zahra Hospital, Dubai.
Copyright
© 2024 Ahmed Shabana. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 24 August 2024
Published: 01 September 2024
Abstract
Purpose: To compare the effect of 532-nm argon laser and 577-nm pattern scanning laser in the anatomy, vasculature and retinal function in patients with diabetic retinopathy
Methods: This was a single-center, interventional, single-blind case series study. Twelve patientes without macular edema and with clinical criteria for treatment according to ETDRS study underwent panretinal photocoagulation with 532-nm or 577-nm laser by a single retina specialist. Changes in retinal morphology and function were assessed before photocoagulation as well as the 1st week, 4th weeks, 8th weeks and 12th weeks after treatment.
Results: Twelve patients were enrolled in 532-nm laser treatment (50%) or 577-nm laser treatment (50%) homogeneously. No significant difference was seen in visual acuity (p = 0.39), contrast sensitivity (p = 0.76) and color vision (p = 0.21) 3 months after PRP. Additionally, the papillary vascular density was not different at the end of the follow up in both groups (p > 0.05) The average central retinal thickness (CRT) at the 8th week was higher in the argon group (287μm  59μm vs. 268μm 24μm; p < 0.05). Furthermore, the initial size as well as the scar expansion was larger in the argon group in all visits (p < 0.001).
59μm vs. 268μm 24μm; p < 0.05). Furthermore, the initial size as well as the scar expansion was larger in the argon group in all visits (p < 0.001).
Conclusions: There were no significant changes in retinal function at 12th weeks after PRP. The papillary vascular density was restored at the end of the follow up. Patients who underwent argon laser therapy had a significant increase in CRT with larger scar expansion compared to pattern scanning laser group.
Keywords: Diabetic Retinopathy; Argon laser; Pattern scanning laser; Panretinal photocoagulation; Central retinal thickness; papillary vascular density
Analyzing the Structural, Flowmetric, and Functional Effects of using a 532-nm Argon Laser for Panretinal Photocoagulation in Diabetic Retinopathy as Opposed to a 577-nm Pattern Scanning Laser
Introduction
Diabetic retinopathy is the number one cause of visual impairment in working-age adults around the world. This disease is characterized by poor capillary perfusion and retinal ischemia, which leads to macular edema and neovascularization, and can severely alter the visual function of these patients.
Likewise, although panretinal photocoagulation (PRP) has provided an effective treatment to reduce the risk of severe visual loss in patients with diabetic retinopathy, it is not absent of complications that can result in central function loss due to macular edema, peripheral constriction of the visual field with poor adaptation to darkness and accommodation (1).
For that reason, different types of lasers have been created with modifications of international protocols to try to minimize these effects as much as possible and the PASCAL® laser has been postulated as a proposal to this objective, controlling energy delivery in short pulse duration (2).
The laser energy is transformed into heat when absorbed by the melanin of the retinal pigmented epithelium and the hemoglobin contained within the vessels, so with less pulse duration, less energy extends in all directions changing in a more innocuous way the retinal tissue, with less lateral thermal diffusion and damage to the RPE and less alteration of the internal retina, with a better patient tolerance and less collateral damage compared to the conventional laser treatment.(2)
Objectives
General objective
To compare the effect of 532-nm argon laser and 577-nm pattern scanning laser in the anatomy, vasculature and retinal function in patients with diabetic retinopathy.
Specifics objectives
To determine changes in visual acuity, chromatic vision and contrast sensitivity in both groups
Measure changes in central retinal thickness (CRT) and retinal scar expansion over time using spectral domain optical coherence tomography (OCT)
Quantify the variation of papillary retinal circulation by optical coherence tomography guided angiography (OCT-A)
Compare the patients perceived pain and time of each laser session in both laser groups
Methods
The current study was a single-center, interventional, single-blind case series study of patients of 18 year of age or older with severe, very severe or proliferative diabetic retinopathy based on the clinical criteria of the ETDRS.
Subjects were enrolled with informed consent between August 2019 and March 2020. Eyes with the following conditions were excluded: Severe cataract (Stated as NO3NC3C3SCP3 or worse following LOCS III classification), any grade of vitreous hemorrhage, CRT more than 300μm, history of PRP, any retinochoroid pathology other than diabetic retinopathy, history of intravitreal injection within the past 3 months and any optic neuropathy. Demographic data, ophthalmic examination findings and other relevant clinical data was extracted from patient personal record file.
All patients underwent a clinical examination that included baseline best corrected visual acuity (BCVA) with Snellen ETDRS letters, contrast sensitivity with Pelli-Robson chart (From 0 to 100%) and chromatic vision with standard ishihara test (14 color plates). Furthermore, a slit-lamp and dilated fundus examination was performed by a single ophthalmologist altogether with a baseline OCT (Optovue®) to quantify CRT and an OCT-A to measure the papillary vascular density using the platform angiovue (Optovue®).
After informed consent approval, enrolled patients underwent PRP using 532-nm single spot argon laser (OcuLight®,IRIDEX, Mountain View, CA) or 577-nm pattern scanning laser (PASCAL Synthesis® Topcon Canada Inc.) by another single retina specialist. Pupillary dilation was obtained with combined phenylephrine and tropicamide drop (T-P, 50mg/8mg/ml, Sophia®). Topical anesthesia with one drop of proparacaine (Anestears, Lansier®) was administered before laser treatment.
Every patient underwent two separate sessions spared with two weeks between them, using the following parameters: (1) Stardard 200μm spot size using a single lens (Volk® transequator), (2) power and duration were subject to variation until a gray light lesion was attained, thus documenting the average power used in both groups at the end of each laser session. (3) The spots were placed 1 spot away in the argon group and a 3x3 grid with 1.25μm spacing in the pattern scanning laser group. In the subjects, an inferotemporal area below the vascular arcade was selected to measure the scar expansion in no more than 3 scars.
Immediately after the treatment, total session time was recorded and patient perceived pain was assessed with a standardized subjective pain scale from 0 to 10, where 0 indicated that the subject experienced no pain and 10 indicated that the procedure was extremely painful. In that way, another single ophthalmologist performed the measurements of the other variables in the 1st week, 4th weeks, 8th weeks and 12th weeks after treatment.
All the data was analized on SPSS version 23. Significance level considered as p<0.05.
Results
Twelve eyes with severe, very severe or proliferative diabetic retinopathy based on the clinical criteria of the ETDRS were enrolled. The BCVA (logMAR) was 0.25 ± 0.10 before treatment, 0.28 ± 0.11 at the 4th week, 0.3 ± 0.11 at 8th weeks and 0.26 ± 0.11 at the 12th weeks in both de PASCAL and argon group. There was no significant difference between the groups at any time point. (p = 0.39) (Figure 1.)
Figure 1. Mean BCVA
|
|
Before PRP* |
4 weeks after PRP* |
8 weeks after PRP* |
12 weeks after PRP* |
||||
|
BCVA (mean ± SD) |
0.25 ±0.10 |
0.28 ±0.11 |
0.3 ±0.11 |
0.26 ±0.11 |
||||
|
SD = standard deviation; PRP= panretinal photocoagulation |
|
|
|
|||||
In terms of chromatic vision at 12th weeks in the argon group, 1 patient failed in one of the plates of the ishihara test, and another patient presented 2 failures or more. All the remaining patients asserted the 100% of the plates in all the visits. However, this data did not obtain statistical significance after performing a Kruskall-Wallis test for independent variables. (p = 0.21)
The subjective pain was measured from 0 to 10 immediately after panretinal photocoagulation treatment (Figure 2). The mean pain scale grade was 8.5 ± 1.5 in the argon group and 6 ± 1.4 in the PASCAL group. These changes were statistically significant using a t-student test (p < 0.05).
Mean panretinal photocoagulation session time was 7.69 ± 5.30 minutes and 4.63 ± 2.63 minutes in the argon and PASCAL group respectively (p <0.05). The mean number of PRP burn was 657 ± 377 in the argon group and 887 ± 434 in the PASCAL group (p <0.05) (Figure 2).
Figure 2. Mean PRP session time, PRP burn and subjective perceived pain
|
|
Argon single spot laser group |
Short pulse pattern scan laser group |
P value |
|
PRP session time* (mean ± SD) |
7.69 |
4.63 |
p < 0.05 |
|
Number of burns (mean ± SD) |
657 ±377 |
887 ±434 |
p < 0.05 |
|
Patient perceived pain (mean ± SD) |
8.5 ± |
6±1.4 |
p < 0.05 |
|
SD = standard deviation; PRP= panretinal photocoagulation; *Measured in minutes |
|||
Figure 3. Mean CRT, peripapillary ONH vascular density and horizontal scar diameter (PASCAL group)
|
|
Before PRP* |
1 week after PRP* |
4 weeks after PRP* |
8 weeks after PRP* |
12 weeks after PRP* |
|
CRT (μm) |
256μm |
261μm |
262μm |
268μm |
265μm± |
|
ONH vascular density (%) |
56% |
54.56% |
55.1%±3.51% |
53.18% |
54.9% |
|
Horizontal scar diameter (μm) |
- |
162μm± |
171μm ± |
198μm± |
214μm±31μm |
|
CRT = central retinal thickness; ONH = optic nerve head; PRP= panretinal photocoagulation *Values are expressed as the mean ± standard deviation. |
|||||
Figure 4. Mean CRT, peripapillary ONH vascular density and horizontal scar diameter (argon group)
|
|
Before PRP* |
1 week after PRP* |
4 weeks after PRP* |
8 weeks after PRP* |
12 weeks after PRP* |
|
CRT (μm) |
259μm |
253μm± |
268μmμm |
287μmμm |
274μmμm |
|
ONH vascular density (%) |
56% |
55.24%± |
55.46%± |
56.28% |
56.92%±08% |
|
Horizontal scar diameter (μm) |
- |
304μm |
288μm± |
329μm± 51μm |
354μm±46μm |
|
CRT = central retinal thickness; ONH = optic nerve head; PRP= panretinal photocoagulation *Values are expressed as the mean ± standard deviation. |
|||||
The mean peripapilar vascular density was 56%± 1.27% before laser treatment, 55.24%± 3.82% at the 1st week, 55.46%± 3.48% at the 4th week, 56.28%± 1.27% at the 8th week and 56.92%± 2.08% in the 12th week in the argon group. (Figure 4) The PASCAL group presented 56%± 1.45% before laser treatment, 54.56%± 3.14% at the 1st week, 55.1%± 3.51% at the 4th week, 53.18%± 3.82% at the 8th week and 54.9% ± 4.11%.(Figure 3) There was not a statistical difference between baseline and the last follow up using a friedman test (p <0.05)
Regarding scar expansion, the mean scar horizontal diameter was 304μm ± 103μm in the 1st week after laser treatment, 288μm ± 54.6μm at the 4th week, 329μm ± 51μm at the 8th week and 354μm ± 46μm in the argon group. The PASCAL group presented a mean scar horizontal diameter of 162μm ± 46μm at the 1st week after treatment, 171μm ± 27μm at the 4th week, 198μm ± 32μm at the 8th weeks and 214μm ± 31μm at 12th weeks. There was an important statistical difference between the scar diameter in every visit between de argon and PASCAL laser treatment groups using a kruskall-Wallis test (p < 0.001) (Figure 6)
Figure 6. Mean horizontal scar expansion
Discussion
The main objective of this study was to evaluate the changes in the anatomy, vasculature, and retinal function in patients with diabetic retinopathy with good visual acuity and no macular edema that were treated with PRP either with conventional argon laser or PASCAL laser. In our study, non statistically significant changes were noted in BCVA, chromatic vision or contrast sensitivity at the end of the follow up between both laser treatment group.
The subjective patient perceived pain was higher in the conventional argon laser group (8.5 ± 1.5 vs. 6 ± 1.4). Mirashi et al. compared pain scores in patients with severe NPDR or PDR, in which one eye of each patient was randomized to undergo conventional laser and the other one to short pulse laser. In their study, subjects had an average pain score of 7.5 ± 1.14 and 1.75 ± 0.87 in the conventional and in the short duration laser group respectively. (3) Reduced pulse duration may be correlated with less pain due to decreased thermal diffusion into the choroid, which is rich in sensory nerves, resulting in minor collateral damage. This fact associated with shorter laser sessions makes short pulse laser therapy more tolerable by patients as demonstrated in this study. (3-5)
In our data, patients in the conventional argon group presented an increase in CRT at the 8th week that had statistically significance. Many studies had evaluated this effect in CRT (3, 6-8) Mirashi et al. study demostrated an increase in mean central macular thickness as early as the 1st week (37.9 μm vs. 8.7μm) that remained 4 months later (50.8μm vs. 9.1μm) (p<0.05) (3) Takamura et al. showed that more patients in the conventional laser group had more than a 20% increase in CRT from baseline in comparison to the PASCAL group at 18th weeks (23.8% vs. 9.5%) (p<0.05) (7) Similar results were presented by Mahgoub et al. with a slight increase from baseline (33.68μm vs. 26.06μm) (8) This stated difference is probably associated with the fact that with a longer duration, there is a greater tissular disruption with subsequent release of IL-6, ICAM-1 and MCP-1 that upregulates VEGF and causes an increase in vascular permeability(1,7)
Other methods described previously have been used to quantify the variation in the optic nerve head flow after PRP, like speckle flowgraphy, and there is limited literature with the use of OCT angiography in this specific field. As far as the authors are aware, there’s no comparative data of the variation in the optic nerve head flow using this method between conventional argon laser and PASCAL laser photocoagulation. In our study, there was a slight diminish in the optic nerve head flow in the 4th week and the 8th week in both groups respectively (Figure 7). At the end of the follow up, the ONH flow was not different from the baseline measure, suggesting recovery as showed by Iwase et al. (9) The possible explanation is that PRP improves oxygenation of the ischemic inner retinal layers by destroying metabolically highly active photoreceptor cells resulting in higher retinal oxygen tension which leads to retinal arteries constriction by autoregulation and in reduction in blood flow(9) Studies suggests that gradual recovery is linked with the restoration of the outer retinal layer after photocoagulation (10-13)
Figure 7. Qualitative OCT-A image of a patient that received argon laser PRP
Limited prospective literature exists about scar expansion rate.(14-16) Higaki et al. compared this subject between conventional laser and short pulse pattern scan laser using fundus autofluorescence and a digital image analysis software, finding greater expansion rate in the conventional laser at 12 months of follow up (1.39 ± 0.11 vs. 1.13 ± 0.05, p <0.01). As far we know, there is no comparative data of the scar expansion rate using OCT between both laser groups. Our data shows not only greater initial scar size but greater mean horizontal expansion at 12th week in the subjects who received single spot argon laser PRP (72.12μm ± 61.31μm vs. 43.83μm ± 31.60μm, p<0.001) (Figure 7). Collateral damage to photoreceptors and subsequent apoptosis of surrounding horizontal and amacrine cells occurs after conventional laser although the main target is the RPE. As a consequence, the scar expands, not so when short-pulse laser is performed, in which the retinal damage is limited. (14) Interestingly, we report an initial scar contraction in the conventional laser group. Studies in rabbits demonstrate that in intense and moderate lesions, gliotic scar filling stabilizes after one month, and the wound contracts to approximately 40% of the original lesion diameter with a decrease in early retinal edema(17)There were several limitations that need to be acknowledged in the current study. First, we had strict inclusion and exclusion criteria, so caution is advised to extrapolate this data to the general population. Second, we had a small sample size. To evaluate the exact changes in CRT, ONH flow and scar expansion rate comparing conventional single spot argon laser with short pulse pattern scan laser, a larger sample size would be warranted, although this demonstrated data may be the beginning of future research.
Figure 8. OCT images in which scar expansion is showed in both laser groups
Conclusion
Non statistically significant changes were noted in BCVA, chromatic vision or contrast sensitivity at the end of the follow up. Short pulse pattern scan laser is more tolerable to patients. There was a significant augmentation of CRT in the single spot argon laser group. The ONH vascular density was restored at 12th week after PRP. There was a greater initial size and horizontal scar expansion in the subjects that received conventional argon laser.
References
1) Alasil, T., Waheed, N. Pan retinal photocoagulation for proliferative diabetic retinopathy: pattern scan laser versus argon laser. Curr Opin Ophthalmol 2014, 25:164–170
2)Topcon-medical.es (2020) PASCAL Synthesis 532. Available at: [Accessed 08 March 2020].
3) Mirashi, A., Lashay, A., Roozbahani, M. Pain score of patients undergoing single spot, short pulse laser versus conventional laser for diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol (2013) 251:1103–1107
4) Al-Hussainy S., Dodson P., Gibson J., Pain response and follow-up of patients undergoing panretinal laser photocoagulation with reduced exposure times. Eye (Lond) 2008; 22:96–99.
5) Inan, S., Polat, O., Yigit, S., PASCAL laser platform produces less pain responses compared to conventional laser system during the panretinal photocoagulation: a randomized clinical trial. . Afri Health Sci. 2018;18(4): 1010-1017
6) Muqit M., Marcellino G., Henson D., et al. Single-session vs. multiple- session pattern scanning laser panretinal photocoagulation in proliferative diabetic retinopathy: The Manchester Pascal Study. Arch Ophthalmol 2010; 128:525 – 533.
7) Takamura, Y., Arimura, S., Miyake, S. Panretinal Photocoagulation Using Short-Pulse Laser Induces Less Inflammation and Macular Thickening in Patients with Diabetic Retinopathy. Hindawi Journal of Ophthalmology Volume 2017, Article ID 8530261
8) Mahgoub M., Macky T., (2017) El efecto de la panfotocoagulación con láser en edema macular diabético con el fotocoagulador Pascal ® versus el láser de argón convencional. ophthalmologica 2017;238(suppl 1):16–20
9) Iwase, T., Mikoshiba, Y., Evaluation of blood flow on optic nerve head after pattern scan and conventional laser panretinal photocoagulation. Medicine (2019) 98:24(e16062)
10) Yamada, Y., Suzuma, K., Onizuka, N. Evaluation of retinal blood flow before and after panretinal photocoagulation using pattern scan laser for diabetic retinopathy. Current eye research 2019. ISSN:0271-3683
11) Diddie KR, Ernest JT. The effect of photocoagulation on the choroidal vasculature and retinal oxygen tension. Am J Ophthalmol 1977;84:626.
12) Roider J., Michaud N., Flotte T., et al. Response of the retinal pigment epithelium to selective photocoagulation. Arch Ophthalmol 1992;110: 1786–92.
13) Iwase T., Ueno Y., Ra E., et al. Changes in choriocapillaris and retinal morphology after laser photocoagulation by OCT angiography: a case report. Medicine (Baltimore) 2018;97:e13278.
14) Higaki M., Nozalo M., Yoshida M. Less Expansion of Short-Pulse Laser Scars in Panretinal Photocoagulation for Diabetic Retinopathy. Hindawi Journal of Ophthalmology Volume 2018, Article ID 9371895
15) Maeshima K., Utsugi-Sutoh N., Otani T., et al. Progressive enlargement of scattered photocoagulation scars in diabetic retinopathy. Retina (2004)
16) Muqit M. et al., “Fundus autofluorescence and Fourier-domain optical coherence tomography imaging of 10 and 20 millisecond Pascal retinal photocoagulation treatment,” British Journal of Ophthalmol- ogy, vol. 93, no. 4, pp. 518–525,
17) Paulus Y., Jain A., Gariano R., et al. Healing of retinal photocoagulation lesions. Invest Ophthalmol Vis Sci. 2008;49(12):5540–5545.
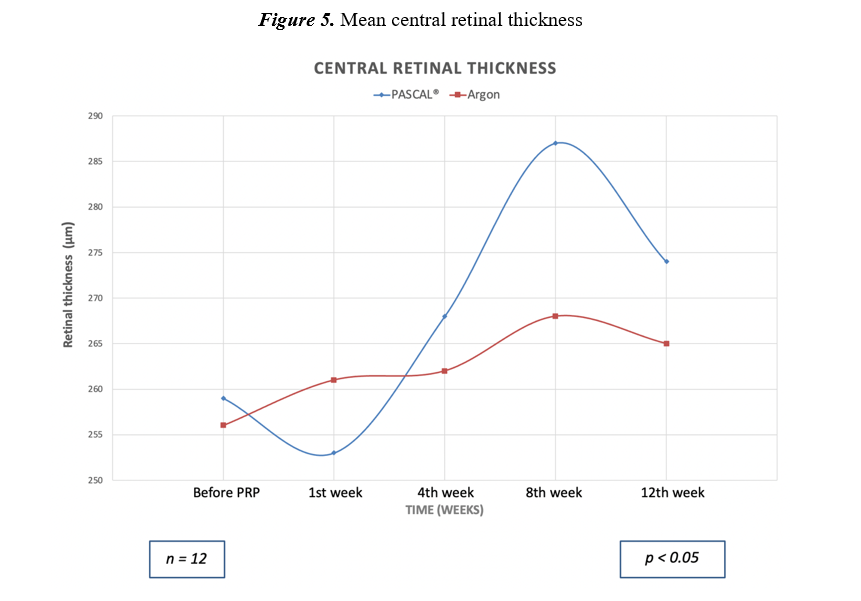
Figure 1
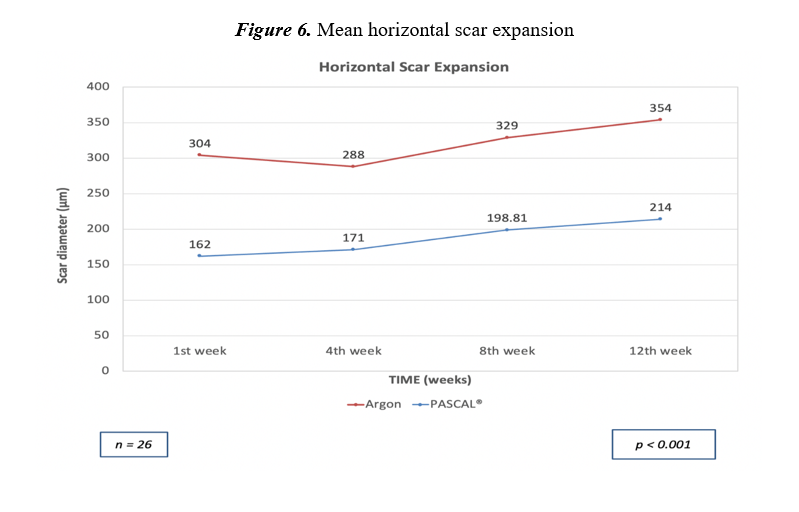
Figure 2
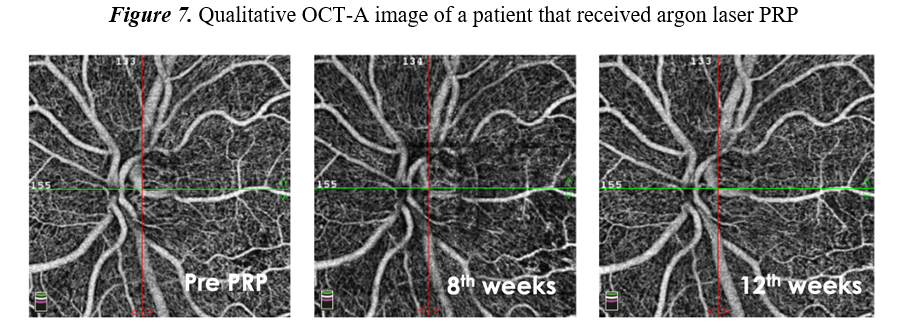
Figure 3
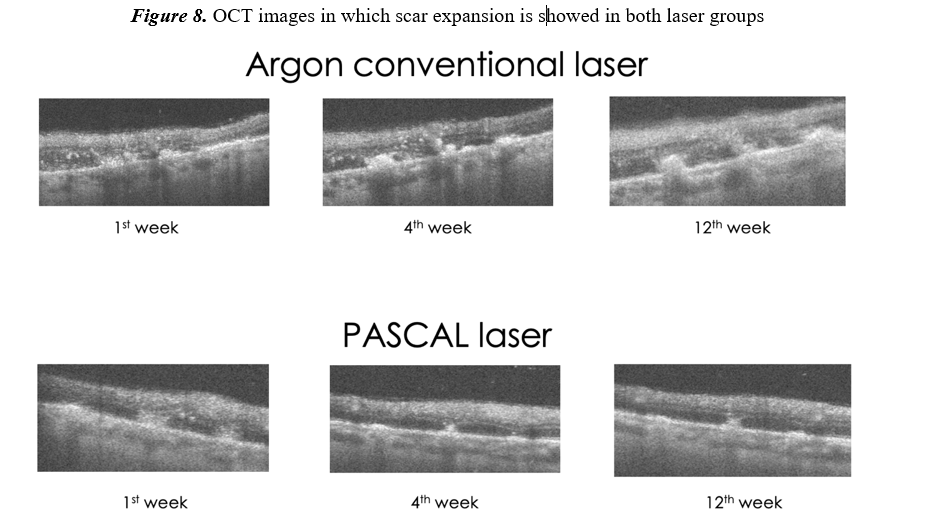
Figure 4

 ±5.30
±5.30