The Impact of Working Shifts on the Lifestyle of Healthcare Providers in Riyadh
The Impact of Working Shifts on the Lifestyle of Healthcare Providers in Riyadh
Hassan M Alrefaee *1, Mohammed T Aldawsari 2
1.Anfas Medical Care Hospital.
2.King Fahad Medical City.
*Correspondence to: Hassan M Alrefaee.
Copyright
© 2024 Hassan M Alrefaee., This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 20 August 2024
Published: 04 September 2024
The Impact of Working Shifts on the Lifestyle of Healthcare Providers in Riyadh
Introduction
Healthcare systems worldwide depend on shift work to ensure continuous patient care, particularly in hospital settings where services are required around the clock. This necessity for uninterrupted care means that healthcare providers, including doctors, nurses, and support staff, often work irregular hours that deviate from the typical 9-to-5 schedule. While this system is essential for patient care, it introduces a range of challenges for the healthcare workers themselves.
Shift work disrupts the natural circadian rhythms, which are the physical, mental, and behavioral changes that follow a 24-hour cycle, primarily responding to light and darkness in the environment. The disruption of these rhythms can lead to significant sleep disturbances, such as difficulty falling asleep, maintaining sleep, or experiencing non-restorative sleep. These sleep disorders are not just minor inconveniences; they can lead to severe health issues like chronic fatigue, cognitive impairment, and an increased risk of cardiovascular diseases (Zaidi et al., 2017).
Moreover, irregular working hours often lead to unhealthy eating habits. Some shift workers may experience a poor appetite, leading to weight loss and nutritional deficiencies, while others might develop an increased appetite, resulting in weight gain and related conditions like obesity and metabolic syndrome. These eating patterns are often accompanied by gastrointestinal problems and a general decline in physical health.
Psychologically, shift work can be taxing, contributing to elevated stress levels, anxiety, and depression. The nature of shift work can isolate healthcare providers from their families and social circles, leading to poor social relationships and a feeling of disconnection from their support systems. This social isolation can exacerbate feelings of burnout and reduce job satisfaction, impacting the overall quality of life of these professionals.
In the context of Riyadh, Saudi Arabia, these challenges are particularly pertinent given the city's unique socio-cultural and economic environment. Healthcare providers in Riyadh are subject to the same physiological and psychological stresses as their counterparts worldwide, but cultural expectations and the specific demands of the Saudi healthcare system may amplify these effects.
This study aims to investigate the multifaceted impacts of shift work on healthcare providers in Riyadh, focusing on their sleep patterns, appetite, weight changes, stress levels, and social relationships. By identifying the specific challenges faced by these workers, the study seeks to inform policies and interventions that can mitigate the adverse effects of shift work. Improving the well-being of healthcare providers is not only beneficial for the workers themselves but also critical for maintaining high standards of patient care and overall healthcare system efficiency (Almalki et al., 2012).
The findings of this study will contribute to the growing body of knowledge on occupational health in healthcare settings and provide evidence-based recommendations for managing shift work more effectively. Understanding the full scope of shift work's impact on healthcare providers in Riyadh will help in designing targeted strategies to enhance their quality of life, job satisfaction, and the quality of care they deliver (Al-Raddadi et al., 2019).
Study Problem
Healthcare professionals in Riyadh, Saudi Arabia, face the unique challenges associated with shift work. These challenges include disrupted sleep patterns, poor appetite, weight fluctuations, heightened stress, and compromised social relationships. While the continuous, round-the-clock nature of healthcare services is necessary for patient care, it imposes a significant burden on the healthcare workers who must adapt to irregular working hours.
The disruption of natural circadian rhythms due to shift work can lead to sleep disorders, which are linked to numerous health problems such as chronic fatigue, cognitive impairments, and increased risk of cardiovascular diseases. Furthermore, irregular meal times and the stress associated with shift work can result in poor appetite and significant weight changes, either weight gain or weight loss, both of which have their own health implications.
Psychological stress is another critical issue, as healthcare workers dealing with shift work often report higher levels of stress, anxiety, and depression. The demanding and unpredictable nature of their schedules can also lead to poor social relationships and feelings of isolation from family and friends, exacerbating the psychological toll and potentially leading to burnout (Alnaami et al., 2019).
In Riyadh, these problems are compounded by the specific socio-cultural and economic environment, which may amplify the stress and health risks associated with shift work. Despite these significant issues, there has been limited research focusing on the specific impacts of shift work on healthcare providers in this region (Banday et al., 2015).
Therefore, this study seeks to address the following problem: What are the specific impacts of shift work on the sleep patterns, appetite, weight, stress levels, and social relationships of healthcare providers in Riyadh, Saudi Arabia?
Understanding these impacts is crucial for developing effective interventions and policies to support the well-being of healthcare workers. By investigating these issues, the study aims to provide a comprehensive overview of the challenges faced by healthcare providers in Riyadh and propose actionable recommendations to mitigate the negative effects of shift work, ultimately improving the quality of life for these essential workers and enhancing the overall efficiency of the healthcare system.
Importance of the Study
The importance of this study on the impacts of shift work on healthcare providers in Riyadh, Saudi Arabia, cannot be overstated. It addresses a critical and multifaceted issue that affects not only the well-being of healthcare workers but also the overall quality of healthcare services provided to the population. The significance of this study can be elaborated on several key dimensions:
1.Healthcare Worker Well-being
Healthcare workers are the backbone of the medical system, and their health and well-being are paramount. Shift work, with its associated irregular hours, can lead to a range of health issues, including sleep disorders, weight fluctuations, and increased stress levels. By identifying and understanding these impacts, the study can help in formulating targeted interventions to improve the physical and mental health of healthcare workers. Enhanced well-being of healthcare providers can lead to improved job satisfaction, reduced burnout, and lower turnover rates, ensuring a more stable and effective workforce (Alqahtani et al., 2019).
2. Patient Care Quality
The health and performance of healthcare workers directly influence the quality of patient care. Fatigued, stressed, and unhealthy workers are more prone to errors, which can compromise patient safety. By addressing the negative effects of shift work, this study aims to contribute to strategies that ensure healthcare workers are well-rested, healthy, and mentally fit, thereby enhancing their ability to provide high-quality care. This is particularly crucial in a high-stakes environment like healthcare, where the margin for error is minimal (Aldrees et al., 2015).
3. Policy Development
The findings of this study can inform policymakers and healthcare administrators about the specific challenges faced by shift-working healthcare providers. This knowledge is essential for developing effective workplace policies and regulations that protect and support healthcare workers. Policies could include adjustments to shift scheduling, provision of mental health support, nutritional programs, and other wellness initiatives tailored to the needs of shift workers. These changes can lead to a more humane and supportive work environment, which is essential for long-term sustainability in the healthcare sector (Alotni & Elgazzar, 2020).
4. Economic Impact
Healthcare is a significant sector within the economy, and the efficiency and productivity of healthcare workers have direct economic implications. Health issues among workers can lead to increased absenteeism, higher healthcare costs, and reduced productivity, all of which can strain the healthcare system financially. By mitigating the adverse effects of shift work, the study can contribute to economic benefits through reduced healthcare costs, lower rates of absenteeism, and improved productivity among healthcare workers (AlAteeq et al., 2020).
5. Cultural and Social Relevance
In Riyadh, and more broadly in Saudi Arabia, cultural and social factors play a significant role in shaping the experiences and challenges of healthcare workers. Understanding these specific socio-cultural dynamics is crucial for developing interventions that are culturally appropriate and effective. The study’s focus on Riyadh allows for insights that are directly relevant to the local context, ensuring that proposed solutions are feasible and culturally sensitive (Albawardi et al., 2016).
6. Scientific Contribution
This study adds to the growing body of literature on occupational health, particularly in the context of shift work. By focusing on healthcare providers in Riyadh, it fills a gap in the existing research, providing valuable data and insights that can be used by researchers, academicians, and practitioners globally. The study’s findings can serve as a basis for further research in other regions and among different occupational groups, contributing to a broader understanding of the impacts of shift work (Thirunavukkarasu et al., 2021).
7.Work-Life Balance
Achieving a healthy work-life balance is essential for the overall well-being of individuals. The study explores how shift work affects the social relationships and family life of healthcare providers. By highlighting these impacts, the research can lead to recommendations that help workers achieve a better balance between their professional responsibilities and personal lives. This balance is crucial for maintaining long-term mental and emotional health, which benefits both the workers and their families (Aziz et al., 2022).
This study is of paramount importance as it addresses a critical issue affecting a vital segment of the workforce. The outcomes of this research have the potential to significantly improve the health and well-being of healthcare providers in Riyadh, enhance the quality of patient care, inform policy development, and contribute to the scientific community’s understanding of shift work. By shedding light on the specific challenges faced by healthcare workers, this study aims to drive meaningful change and support the sustainable development of the healthcare sector in Saudi Arabia (Mandil et al., 2016).
Objectives of the Study
The primary aim of this study is to investigate the effects of shift work on healthcare providers in Riyadh, Saudi Arabia. By focusing on various physical, mental, and social aspects of health, this study seeks to provide a comprehensive understanding of how shift work impacts healthcare professionals. The specific objectives of the study are as follows:
Identify the Prevalence of Sleep Disorders Among Shift Workers:
- To determine the extent and types of sleep disorders, such as insomnia, oversleeping, or under sleeping, experienced by healthcare providers working shifts.
Assess the Impact of Shift Work on Appetite and Weight:
- To evaluate changes in appetite and weight among healthcare workers, identifying trends of poor appetite, increased appetite, weight loss, or weight gain associated with shift work.
Examine the Prevalence of Chronic Health Conditions:
- To identify the prevalence of chronic health conditions such as hypertension, diabetes mellitus (DM), and cardiac diseases among healthcare workers engaged in shift work.
Evaluate the Effects of Shift Work on Mental Health:
- To assess the levels of stress, anxiety, and burnout experienced by healthcare providers working shifts, and how these factors influence their overall mental well-being.
Investigate the Social Impacts of Shift Work:
- To explore the social implications of shift work, including its effects on social relationships, family life, and participation in social gatherings.
Determine the Overall Quality of Life of Shift Workers:
- To assess the overall quality of life of healthcare providers working shifts, considering factors such as fatigue, energy levels, and life satisfaction.
Evaluate the Coping Mechanisms and Satisfaction Levels:
- To understand the coping mechanisms employed by healthcare workers to manage the challenges of shift work and to assess their overall job satisfaction.
Provide Recommendations for Improving Shift Work Conditions:
To offer evidence-based recommendations for healthcare administrators and policymakers to improve the working conditions and health outcomes of shift workers.
By achieving these objectives, the study aims to provide a detailed and nuanced understanding of the various challenges faced by healthcare providers working shifts. The findings are expected to contribute to the development of targeted interventions and policies that can enhance the well-being of healthcare professionals, improve patient care, and promote a more sustainable and effective healthcare system in Riyadh, Saudi Arabia.
Study Questions
- What is the prevalence of sleep disorder syndromes (oversleep vs. under sleep) among healthcare providers working in shifts?
- How does shift work affect appetite and weight changes among healthcare providers?
- What is the relationship between shift work and the prevalence of chronic health conditions such as hypertension, diabetes mellitus, and cardiac disease?
- How does shift work impact social relationships and overall quality of life for healthcare providers?
- What are the levels of stress, anxiety, irritability, and burnout experienced by healthcare providers working shifts?
- How do shift work-related factors influence smoking behavior and job satisfaction among healthcare providers?
study Hypothesis
- Healthcare providers working in shifts have a higher prevalence of sleep disorders compared to those working regular hours.
- Shift work is associated with significant changes in appetite and weight, with providers reporting either increased or decreased appetite and corresponding weight changes.
- Healthcare providers working shifts are more likely to experience chronic health conditions such as hypertension, diabetes mellitus, and cardiac disease compared to their counterparts on regular shifts.
-Shift work negatively impacts social relationships and overall quality of life for healthcare providers.
-Healthcare providers working shifts report higher levels of stress, anxiety, irritability, and burnout compared to those not working shifts.
-Shift work is associated with an increased likelihood of smoking behavior and decreased job satisfaction among healthcare providers.
Scientific Method
Study Design:
This study utilizes a cross-sectional survey design to capture a snapshot of the impact of shift work on healthcare providers.
Participants:
The sample includes healthcare providers from various hospitals in Riyadh, Saudi Arabia, encompassing a range of roles (e.g., doctors, nurses) and shifts (e.g., day, night, rotating).
Data Collection:
Data is collected through a structured questionnaire consisting of demographic questions and specific survey items related to health, social, and job-related factors.
Survey Instrument:
The survey includes both closed-ended and open-ended questions to obtain comprehensive data on sleep patterns, appetite and weight changes, health conditions, social relationships, stress levels, and job satisfaction.
Sampling Method:
A stratified random sampling approach ensures diverse representation across different hospital departments and shift types, with random selection from a list of healthcare providers.
Data Analysis:
Quantitative data is analyzed using statistical methods such as descriptive statistics, chi-square tests, and regression analysis to identify significant patterns and relationships. Qualitative data from open-ended responses is analyzed using thematic analysis to explore underlying themes and perspectives.
Ethical Considerations:
The study adheres to ethical guidelines, ensuring informed consent, confidentiality, and the voluntary participation of all respondents. Ethical approval is obtained from a relevant review board.
Limitations:
The study acknowledges limitations such as potential response bias, the inherent cross-sectional nature of the research, and limitations in generalizability to other settings or populations.
Previous Studies/Research
Introduction
The issue of burnout among healthcare professionals has become increasingly prominent in recent years, reflecting the growing recognition of the intense demands and pressures faced by those in the field. Burnout, a state characterized by chronic emotional exhaustion, depersonalization, and diminished personal accomplishment, significantly impacts the mental and physical well-being of healthcare workers. This phenomenon is particularly concerning given the essential role that healthcare professionals play in delivering quality care and maintaining patient safety.
Burnout among healthcare workers is often exacerbated by the nature of their work environment, which frequently includes long hours, high-stress situations, and irregular shift patterns. The challenges associated with shift work, such as disrupted sleep patterns and social isolation, contribute to the risk of burnout and affect overall job satisfaction and performance. Additionally, factors such as high workload, lack of support, and inadequate work-life balance further compound the problem, leading to increased rates of absenteeism, turnover, and decreased quality of care (Alghadir et al., 2017).
Understanding the factors that contribute to burnout is crucial for developing effective strategies to mitigate its impact. Factors influencing burnout include job demands, personal and professional stressors, and lifestyle behaviors. For instance, irregular working hours and shift work are known to disrupt circadian rhythms and negatively impact sleep quality, which in turn can affect mood, cognitive function, and overall health. Furthermore, the physical and emotional demands of healthcare work, combined with inadequate resources and support, can lead to a cycle of stress and burnout.
Efforts to address burnout in healthcare settings require a multifaceted approach that includes both organizational and individual-level interventions. Organizational changes might involve implementing more supportive work environments, optimizing shift schedules, and providing adequate resources and training. At the individual level, promoting healthy lifestyle choices, stress management techniques, and access to mental health support can play a critical role in alleviating burnout (Alghamdi et al., 2017).
Previous Studies/Research
Alanazi et al. (2020) conducted a significant study on the impact of shift work on the quality of life and sleep among healthcare workers at Prince Sultan Military Medical City (PSMMC) in Riyadh, Saudi Arabia. Their research offers valuable insights into the psychological and physiological challenges faced by healthcare professionals, particularly during the COVID-19 pandemic. This literature review synthesizes their findings within the broader context of existing research on shift work and its effects on health.
The study employed a quantitative observational analytic cross-sectional design, involving 146 healthcare workers. The participants were divided into two groups: shift workers and non-shift workers.
The findings revealed a prevalence of anxiety and depression among the healthcare workers, with 12.3% experiencing anxiety and 14.4% suffering from depression, as measured by the PHQ-4. These rates of mental health issues are consistent with other studies showing heightened levels of psychological distress among healthcare professionals, particularly in high-stress environments like hospitals. The study also found that overall sleep quality was poor, with a mean global PSQI score of 5.69, indicating significant disruptions in sleep among the participants. Poor sleep quality is a well-documented consequence of shift work and has been linked to various adverse health outcomes, including increased risk of cardiovascular disease and impaired cognitive function.
In terms of daytime sleepiness, the ESS results showed that 1.4% of participants experienced severe sleepiness, 2.7% had moderate sleepiness, and 8.9% reported mild sleepiness. These findings highlight the impact of shift work on alertness and daytime functioning. Interestingly, the study found no significant differences in the prevalence of anxiety, depression, and other comorbidities between shift workers and non-shift workers, except for daytime sleepiness. Shift workers had a lower mean ESS score (4.94) compared to non-shift workers (7.13), with a p-value of 0.012, indicating that shift workers reported less daytime sleepiness.
These results contribute to the ongoing discussion about the effects of shift work on healthcare workers' well-being. While the study did not find significant differences in mental health issues between the two groups, the overall poor sleep quality and prevalence of anxiety and depression highlight the need for targeted interventions. The research underscores the importance of addressing both psychological and physiological aspects of healthcare workers' health to mitigate the negative impacts of shift work. This includes implementing strategies to improve sleep hygiene, providing mental health support, and exploring scheduling adjustments to better accommodate workers' needs.
Alanazi et al. (2020) provide a valuable contribution to the literature on shift work and its impact on healthcare workers. Their findings are consistent with existing research that highlights the challenges of shift work on mental health and sleep quality. The study reinforces the need for continued efforts to support healthcare professionals in managing the demands of their work environment and improving their overall well-being.
Almajwal (2015) explored the interconnections between physical activity, body mass index (BMI), shift duty, and eating habits among nurses in Riyadh, Saudi Arabia. This cross-sectional study, which focused on 362 non-Saudi female nurses, provides critical insights into the lifestyle and health challenges faced by a key group of healthcare providers.
The study revealed that 46.7% of the nurses were either overweight or obese, highlighting a significant public health concern. The research identified several predictors of physical activity, including marital status, shift duty, education level, and BMI. Notably, shift duty was associated with higher BMIs compared to day shift work, with a statistically significant difference (p = 0.004). This finding aligns with other research suggesting that shift work can contribute to weight gain, potentially due to disruptions in normal eating patterns and reduced opportunities for physical activity.
Barriers to physical activity were also examined, with weather conditions, lack of transportation, and time constraints being the most frequently reported obstacles. These factors reflect common challenges that may hinder the ability of healthcare workers to engage in regular exercise, which is crucial for maintaining a healthy weight and overall well-being. The study's findings on eating habits further underscore the relationship between diet and weight. Nurses who infrequently ate breakfast and main meals or frequently consumed fast food were more likely to be overweight or obese. These eating behaviors are known risk factors for poor health outcomes and highlight the need for better nutritional guidance and support for healthcare workers.
The study's results emphasize the importance of promoting healthy lifestyle practices among nurses, particularly those working shifts. Addressing barriers to physical activity and improving dietary habits are essential for reducing the prevalence of obesity and related health issues. By focusing on these areas, healthcare institutions can support their staff in adopting healthier behaviors, ultimately benefiting both the workers and the patients they serve.
Almajwal's research contributes valuable knowledge to the field of occupational health, particularly within the context of healthcare professions. The findings suggest that targeted interventions addressing both physical activity and dietary habits are necessary to improve the health and well-being of nurses, thereby enhancing their overall quality of life and performance in their critical roles.
Ghanem et al. (2022) conducted a study to evaluate the impact of shift work on the quality of life and sleep among healthcare workers at Prince Sultan Military Medical City (PSMMC) in Riyadh, Saudi Arabia. This research is particularly relevant in today's industrialized economy where shift work is prevalent in sectors such as healthcare and public safety. The study employed a quantitative observational analytic cross-sectional design, targeting both shift workers and non-shift workers within the healthcare setting.
The study included 146 participants, with a majority being female (74.66%), non-Saudi (64.38%), and predominantly nurses (69.18%). The results revealed that 12.3% of participants experienced anxiety, while 14.4% experienced depression. These figures highlight a concerning level of psychological distress among healthcare workers, though no significant differences in the prevalence of these conditions were found between shift workers and non-shift workers.
The study found that the overall mean global PSQI score was 5.69, indicating poor sleep quality among participants. This is consistent with previous research linking shift work to disrupted sleep patterns. Regarding sleepiness, the study reported that severe sleepiness was found in 1.4% of participants, moderate sleepiness in 2.7%, and mild sleepiness in 8.9%. Interestingly, the total ESS score was significantly higher among non-shift workers (mean score of 7.13) compared to shift workers (mean score of 4.94), with a p-value of 0.012. This suggests that shift workers experienced less severe sleepiness than their non-shift counterparts, a finding that diverges from some previous research which often reports worse sleep outcomes for shift workers.
The study's findings underscore the complexity of the relationship between shift work and various health outcomes. While shift workers showed poorer sleep quality, the overall impact on anxiety and depression did not significantly differ between shift and non-shift workers. This indicates that while shift work may affect certain aspects of health, other factors could also play a role in the overall quality of life and psychological well-being of healthcare workers.
The study by Ghanem et al. contributes valuable insights into the effects of shift work on healthcare workers' sleep and quality of life. Despite the challenges associated with shift work, the differences in psychological outcomes between shift and non-shift workers were not as pronounced as might be expected. This highlights the need for further research to explore other factors influencing health outcomes among healthcare workers and to develop targeted interventions to improve their well-being.
Olawale, Taiwo, and Hesham (2017) conducted a cross-sectional study to evaluate the quality of sleep and overall well-being among healthcare workers in Najran, Saudi Arabia. This research is significant due to the critical role healthcare professionals play in patient care and the potential impact of their well-being on the quality of care provided.
The study involved 123 healthcare workers from various hospitals in Najran, including a diverse group of professionals such as nurses, doctors, pharmacists, and laboratory technicians. The majority of participants were female (76.4%), and the largest subgroup consisted of nurses (60.2%). The researchers administered a questionnaire covering demographic and clinical characteristics, sleep quality, and well-being.
The results revealed that 42.3% of the healthcare workers were classified as poor sleepers. This is a notable finding given the demanding nature of healthcare professions and the potential consequences of inadequate sleep on both health workers and patient outcomes. The study highlighted a significant association between poor sleep and increased levels of perceived stress. Specifically, 84.6% of poor sleepers reported their professional life as being stressful in the past 12 months, compared to 42.3% of good sleepers who felt similarly. Additionally, poor sleepers were more likely to rate their ability to handle unexpected and challenging problems as fair or poor, with 46.2% of them reporting difficulties in contrast to 14.1% of good sleepers.
These findings underscore the relationship between sleep quality and well-being among healthcare workers. The higher levels of stress and perceived difficulty in managing professional challenges among poor sleepers suggest that sleep issues may exacerbate the stress experienced in the healthcare environment. This connection highlights the need for targeted interventions to improve sleep quality and overall well-being among healthcare professionals.
The study emphasizes the importance of addressing sleep quality and well-being in healthcare settings. The significant proportion of poor sleepers and their associated stress levels point to a pressing need for healthcare organizations to implement programs aimed at improving the social, physical, and psychological well-being of their staff. Such initiatives could potentially enhance both the quality of life for healthcare workers and the quality of care provided to patients.
Salah, Malak, and Salameh’s (2020) study sheds light on the profound impact of shift work on the lifestyle behaviors of emergency department nurses in Jordan. This cross-sectional, descriptive correlational research focused on assessing how the demanding nature of shift work affects key aspects of lifestyle, including dietary habits, physical activity, and nicotine dependence. The research was conducted among 275 nurses employed in various emergency departments across Jordanian hospitals, providing a substantial sample for examining these critical issues.
The results of the study revealed a concerning prevalence of unhealthy lifestyle behaviors among the participants. Over half of the nurses (50.2%) reported poor dietary habits, which are often linked to irregular eating patterns and limited access to nutritious food options during shifts. Shift work disrupts normal meal times and can lead to reliance on quick, often unhealthy food choices, contributing to these poor dietary habits. Furthermore, 81.8% of the nurses were found to be physically inactive. The nature of shift work, with its erratic hours and high stress levels, likely limits opportunities for regular physical activity, which is essential for maintaining overall health and preventing chronic conditions.
Nicotine dependence was another significant finding, with 65.1% of the nurses reporting reliance on nicotine. This high rate of nicotine dependence could be attributed to the stressful environment and irregular schedules associated with shift work, which may drive individuals to seek stress relief through smoking. The study highlighted a positive correlation between shift work and adverse lifestyle behaviors, indicating that the demands and stressors associated with shift work contribute to poor dietary habits, reduced physical activity, and increased nicotine dependence.
The implications of these findings are substantial for healthcare management. Shift work, while necessary for 24/7 healthcare services, poses challenges that affect nurses' health and well-being. The study underscores the importance of developing and implementing targeted intervention programs to address these challenges. Healthcare organizations need to consider the specific needs of shift workers when designing health promotion and support programs.
This could include providing healthier food options during shifts, creating opportunities for physical activity within the work environment, and offering support for smoking cessation.
By addressing these areas, healthcare institutions can help improve the overall health of their nursing staff, which, in turn, can enhance job performance and patient care quality. Ensuring that shift workers have access to resources and support for maintaining a healthy lifestyle is crucial for sustaining a productive and resilient healthcare workforce. The study by Salah, Malak, and Salameh highlights the urgent need for a comprehensive approach to support nurses working under the demanding conditions of shift work, aiming to promote better health outcomes and improve quality of life for these essential healthcare professionals.
Selaihem’s (2013) study delves into the prevalence of burnout among primary care physicians working at the Riyadh Military Hospital (RMH) in Saudi Arabia, highlighting critical aspects of job-related stress and its impact on healthcare professionals. Burnout, characterized by emotional exhaustion, depersonalization, and reduced personal accomplishment, significantly affects job performance and overall career satisfaction, particularly in high-stress environments like healthcare.
The study utilized a cross-sectional survey approach, distributing nearly 200 questionnaires among primary care doctors at RMH. A total of 144 responses were collected, reflecting a response rate of 72%. The survey employed the Maslach Burnout Inventory Human Services Survey (MBI-HSS), a validated tool for measuring burnout across three dimensions: emotional exhaustion (EE), depersonalization (DP), and personal accomplishment (PA). This comprehensive approach allowed for a nuanced understanding of burnout levels and their associated factors.
The results revealed a high prevalence of burnout among the surveyed physicians. Over half of the respondents (53.5%) exhibited high levels of emotional exhaustion, indicating significant psychological and emotional strain. Nearly 39% experienced high depersonalization, reflecting a sense of detachment from patients and a reduced ability to empathize. About 28.5% of respondents reported low levels of personal accomplishment, suggesting a diminished sense of achievement in their professional roles. Notably, 2.78% of the physicians scored high in all three burnout dimensions, illustrating severe burnout.
Several factors were identified as strongly associated with higher burnout levels. These included low job satisfaction, a desire to change jobs, tobacco use, and the consumption of psychotropic medications.
Younger physicians, those who had recently graduated, and married doctors also reported higher burnout levels. These findings underscore the multifaceted nature of burnout and its connection to both personal and professional factors.
The study’s conclusions emphasize the widespread nature of burnout among primary care doctors at RMH and its strong association with various personal and work-related indicators. The authors advocate for improved employment conditions and support systems to mitigate burnout, suggesting that future research should focus on developing models to better understand the phenomenon. Additionally, identifying causative factors and effective intervention strategies is crucial for enhancing the well-being of healthcare professionals and improving their job satisfaction and performance.
Theoretical Framework
Theoretical frameworks provide essential insights into understanding complex phenomena such as burnout among healthcare professionals. These frameworks help in structuring research questions, guiding data collection, and interpreting findings within a broader context. For the study on burnout among healthcare workers, several key theoretical perspectives are relevant.
One foundational theory in understanding burnout is the Maslach Burnout Inventory (MBI), which categorizes burnout into three dimensions: emotional exhaustion, depersonalization, and reduced personal accomplishment. According to this framework, burnout results from prolonged exposure to work stressors, which deplete emotional resources and lead to a sense of detachment and ineffectiveness. This model helps to pinpoint specific areas of burnout that can be addressed through targeted interventions (AlHamam et al., 2022).
Job Demands-Resources (JD-R) Model is another relevant theoretical framework. This model posits that burnout occurs when job demands exceed the resources available to workers. In the context of healthcare, high job demands such as emotional labor, workload, and irregular shifts can lead to exhaustion if not balanced by adequate resources, such as support systems, autonomy, and coping mechanisms. This framework emphasizes the need to manage both job demands and resources to prevent burnout and enhance job satisfaction.
The Transactional Model of Stress and Coping, developed by Lazarus and Folkman, offers additional insights. This model suggests that stress and burnout result from the interaction between an individual's perception of stressors and their coping mechanisms. In healthcare settings, this perspective underscores the importance of personal appraisal and coping strategies in mitigating the effects of work-related stress. It highlights how individual differences in stress perception and coping abilities can influence burnout outcomes (Alharbi & Alkhamshi, 2024).
Circadian Rhythm Theory also plays a significant role in understanding burnout among shift workers. This theory explains how disruptions to the body’s natural circadian rhythms due to irregular work hours can impact sleep quality, overall health, and emotional well-being. Shift work, which often involves night shifts or irregular hours, can lead to misalignment between the internal biological clock and external work demands, exacerbating fatigue and burnout.
Social Support Theory highlights the role of support systems in mitigating burnout. According to this theory, strong social support from colleagues, supervisors, and family can buffer the negative effects of work stress and reduce the likelihood of burnout. In healthcare settings, fostering supportive work environments and improving interpersonal relationships can help alleviate stress and improve job satisfaction.
Incorporating these theoretical frameworks allows for a comprehensive understanding of burnout among healthcare workers by addressing various contributing factors, from job demands and resources to individual coping strategies and circadian disruptions. This multi-dimensional approach helps in designing effective interventions to reduce burnout and improve the well-being of healthcare professionals (Surrati et al., 2024).
Research Methodology
Introduction
The research methodology section outlines the systematic approach used to investigate the research problem, ensuring that the study is conducted in a rigorous and reliable manner. This section provides an overview of the methods and procedures employed to collect, analyze, and interpret data, thereby offering a clear understanding of how the research aims to address the study objectives and answer the research questions.
In this study, a quantitative research methodology is adopted to explore the prevalence and impact of burnout among healthcare workers. By utilizing quantitative methods, the research aims to generate statistically significant findings that can be generalized to the broader population of healthcare professionals. The methodology encompasses the design of the study, data collection procedures, sampling techniques, and analytical methods, all of which are critical for achieving valid and reliable results.
The choice of a cross-sectional design allows for capturing a snapshot of the current state of burnout and its associated factors among healthcare workers. This approach facilitates the examination of relationships between burnout and various influencing factors, such as shift work, lifestyle behaviors, and demographic characteristics. The structured nature of quantitative research ensures that data is collected systematically, analyzed with statistical precision, and interpreted in a way that contributes to a comprehensive understanding of the research problem.
Research Methodology
This study is designed to explore the prevalence of burnout among healthcare workers and identify associated factors influencing burnout. Adopting a quantitative, cross-sectional research design, this approach allows for the collection of data from a large sample at a single point in time, providing a snapshot of the current state of burnout within the target population. The cross-sectional design is particularly useful in assessing the prevalence and associations of burnout, as it enables researchers to analyze and describe the levels of burnout and its correlates without the need for longitudinal data.
To measure burnout, the study employs the Maslach Burnout Inventory (MBI), a well-established tool in burnout research. The MBI assesses burnout across three dimensions: emotional exhaustion, depersonalization, and personal accomplishment. This instrument is chosen for its robust psychometric properties and its capacity to capture the complexity of burnout experiences. Emotional exhaustion refers to feelings of being emotionally overextended and exhausted by one's work, depersonalization involves a sense of detachment or cynicism towards one's patients or clients, and personal accomplishment pertains to feelings of competence and achievement in one's work. These dimensions provide a comprehensive view of burnout, allowing for a nuanced understanding of the different ways burnout can manifest among healthcare workers.
In addition to the MBI, the study utilizes a structured questionnaire to gather data on various factors that might influence burnout. This questionnaire includes sections on demographic information (such as age, gender, and marital status), work-related variables (including shift patterns, job satisfaction, and workload), and lifestyle factors (such as physical activity, dietary habits, and sleep quality). The inclusion of these variables aims to capture a broad range of potential influences on burnout, providing a holistic view of the factors that contribute to burnout among healthcare workers.
The sampling strategy involves purposive sampling, targeting healthcare workers from specific institutions to ensure a representative sample of both shift and non-shift workers. By focusing on healthcare settings, the study aims to include participants who are directly involved in patient care and are therefore at higher risk for burnout. The sample size is determined to achieve statistical power sufficient to detect meaningful differences and relationships within the data.
Data collection is carried out through self-administered questionnaires, ensuring that participants can respond at their convenience while maintaining the anonymity and confidentiality of their responses. The use of validated instruments and structured questionnaires enhances the reliability and validity of the data collected.
Data analysis involves both descriptive and inferential statistical methods. Descriptive statistics provide an overview of the demographic characteristics of the sample and the prevalence of burnout across its dimensions. Inferential statistics, including correlation and regression analyses, are used to examine the relationships between burnout and various predictor variables. These analyses help identify significant predictors of burnout and assess how different factors contribute to the overall burnout experience.
Ethical considerations are a critical component of the research methodology. The study obtains ethical approval from relevant review boards to ensure adherence to ethical standards in research. Informed consent is obtained from all participants, ensuring that they understand the purpose of the study, the nature of their involvement, and their right to withdraw at any time without consequence. By addressing these ethical considerations, the study ensures that the research is conducted with respect for the participants and their rights.
Population and Sample
The study targets healthcare workers within a tertiary healthcare institution in Riyadh, Saudi Arabia. This specific population is chosen due to its relevance to the research objectives, which focus on understanding burnout among professionals who are directly involved in patient care and face significant occupational stress.
The population for this study includes all healthcare workers employed at the institution, encompassing a diverse group of roles such as nurses, physicians, and other medical staff. The institution's size and its diverse healthcare services provide a representative sample of the broader healthcare workforce, allowing for a comprehensive analysis of burnout across different job roles and working conditions.
To ensure a robust and representative sample, the study employs purposive sampling. This non-random sampling method targets healthcare workers who are engaged in both shift and non-shift work. The inclusion of both groups is essential to capture a wide range of experiences related to burnout, as shift work is often associated with increased stress and burnout. By including workers from various shifts, the study can compare the experiences of shift workers with those of their non-shift counterparts.
The sample size is determined based on the need to achieve statistical power and ensure the reliability of the findings. A total of 53 healthcare workers are selected to participate in the study. This sample size is deemed sufficient to provide meaningful insights into the prevalence of burnout and the associated factors. The selection of participants is done to achieve a balance across different healthcare roles, ensuring that the sample reflects the diversity of the healthcare workforce within the institution.
Data collection is carried out through self-administered questionnaires, which are distributed to the selected participants. The questionnaires are designed to capture a wide range of information, including demographic details, job-related factors, and burnout levels. To maximize response rates and ensure the representativeness of the sample, reminders are sent to participants, and multiple collection points are established within the institution.
Ethical considerations are integral to the sampling process. All participants are provided with detailed information about the study and are required to give informed consent before participating. This process ensures that participants are fully aware of their rights and the nature of the research, and it helps maintain the ethical standards of the study.
By carefully selecting a representative sample and using a well-defined sampling strategy, the study aims to obtain accurate and generalizable findings about burnout among healthcare workers. The insights gained from this research are expected to contribute significantly to understanding the factors that influence burnout and inform strategies to improve the well-being of healthcare professionals.
Limitation of the Study
This study, despite its significant contributions to understanding burnout among healthcare workers, faces several limitations that must be considered when interpreting the results.
Firstly, the cross-sectional nature of the research presents a fundamental limitation in establishing causal relationships. The study captures data at a single point in time, which restricts the ability to infer causality between burnout and associated factors. For example, while the study identifies associations between shift work and burnout, it cannot conclusively determine whether shift work causes burnout or if those experiencing burnout are more likely to be assigned to shift work. Longitudinal studies, which track participants over time, could provide more robust insights into the directionality and causality of these relationships.
Another limitation is inherent in the reliance on self-reported data. Participants’ responses may be influenced by various biases, including social desirability bias, where individuals might underreport or overreport symptoms to present themselves in a more favorable light. Recall bias is also a concern, as participants might struggle to accurately remember and report their experiences of burnout or related symptoms. These biases can impact the reliability and validity of the data collected, potentially skewing the study’s findings.
The study’s focus on a single tertiary healthcare institution in Riyadh, Saudi Arabia, limits the generalizability of the findings. The experiences of healthcare workers in this specific setting may not fully represent those in other healthcare environments or geographical locations. Variations in institutional policies, work culture, and regional stressors could affect burnout levels differently, making it challenging to apply the results universally across different settings.
The sample size, although intended to be representative, may still pose limitations. A larger sample size might enhance the study's power to detect more subtle differences and provide more precise estimates.
Additionally, the sample might not fully account for variations within the healthcare worker population, such as differences in roles, levels of experience, and personal circumstances, which could affect burnout levels.
Finally, the study does not address all possible confounding variables that could influence burnout, such as personal life stressors, specific workplace dynamics, or individual coping mechanisms. By not considering these additional factors, the study may miss important elements that contribute to burnout, limiting the comprehensiveness of the findings.
Data Analysis and Results
Introduction
This survey aimed to explore the multifaceted impacts of shift work on the physical and mental well-being of individuals employed in various healthcare settings. With a focus on understanding how shift work influences sleep disorders, appetite changes, weight fluctuations, and overall health, the survey gathered valuable insights from a diverse group of 45 participants.
The survey was meticulously designed to cover a wide range of variables related to shift work. It included 18 questions that delved into several key areas: sleep disturbances, alterations in appetite and weight, prevalence of health conditions such as hypertension, diabetes, and cardiac disease, as well as social and relational impacts. Additionally, it assessed levels of psychological stress, anxiety, and burnout, and explored smoking habits and job satisfaction among the participants. By addressing these areas, the survey sought to provide a holistic view of the consequences of shift work on healthcare professionals.
Participants in the survey were diverse in terms of demographic factors, which adds depth to the analysis. They included both male and female healthcare professionals, varying in marital status, age, and nationality. The age groups ranged from 20-25 years to those above 30 years, allowing for a broad perspective on how different life stages might affect experiences with shift work. Nationally, the majority were Saudi, but there was a notable representation of non-Saudi respondents, enriching the data with varied cultural backgrounds.
The survey also accounted for differences in experience levels, with participants categorized based on their years of service in the healthcare field—from less than 5 years to more than a decade. This classification is crucial for understanding how experience might influence responses to shift work. Participants worked across different shift patterns, including day shifts, night shifts, and rotating shifts, and were employed in various sectors such as government hospitals and private healthcare institutions. The working areas of the participants included critical settings like the ICU, wards, and emergency rooms, each with its unique demands and stressors.
The primary objectives of the analysis are to identify and analyze patterns or correlations between shift work and the participants' physical and mental health. By examining the survey responses, we aim to reveal how different shift patterns and working conditions influence health outcomes, job satisfaction, and overall well-being. This introduction sets the stage for a detailed examination of the data, offering insights that are critical for understanding the broader implications of shift work on healthcare professionals and informing potential interventions or improvements in shift scheduling practices.
Data Analysis
This section provides a comprehensive analysis of the survey data collected from 53 healthcare professionals to understand the impact of shift work on their health and well-being. The analysis encompasses demographic characteristics, health-related metrics, and personal experiences related to shift work.
Demographic Characteristics
The survey sample comprises 53 healthcare professionals, with a gender distribution of 20 (37.7) males (45.1%) and 33(62.3%) females (54.9%). This relatively balanced gender distribution allows for a comparative analysis of how shift work affects males and females differently. For instance, gender-based differences in the perception of shift work’s impact on health can be examined.
Marital status among participants reveals that 30 (56.6%) are married, while 23 (43.3%) are single. This data is pertinent for assessing how marital status influences the experience of shift work, including potential differences in how married individuals and single individuals cope with shift schedules and their associated challenges.
The age distribution of respondents is categorized into three groups: 11 (20.8%) individuals (33.3%) are aged 20-25 years, 17 (32.1%) are aged 26-30 years, and 25 (47.2%) are over 31 years. This diverse age range provides a spectrum of experiences related to shift work, from early career professionals to those with more extensive experience. Analyzing this distribution helps in understanding how age and career stage might affect health outcomes and job satisfaction related to shift work.
The nationality breakdown shows that 20 (37.7%) respondents (58.8%) are Saudi, while 33 (62.3%) are non-Saudi. This diversity allows for an exploration of how cultural and national backgrounds might influence experiences and perceptions of shift work. For example, cultural norms and practices related to work and health could impact how shift work is perceived and managed among different nationalities.
Health and Well-being Metrics
The analysis of health-related issues associated with shift work reveals significant findings. A notable number of respondents, 24 (45.3%), report experiencing sleep disorders. Among these, issues related to oversleeping or undersleeping are prevalent, indicating the disruption of normal sleep patterns due to irregular work hours. This finding is corroborated by data on appetite changes, where 20 (37.7%) participants (27.5%) report a poor appetite during shifts, while 25 (47.2%) experience an increased appetite. Such changes in appetite can be linked to irregular eating patterns and stress associated with shift work.
Weight changes are also notable, with 16 (30.2%) respondents (19.6%) reporting weight gain and 23 (43.4%) experiencing weight loss. These variations in weight suggest that shift work can have varying effects on metabolic health, potentially due to changes in diet, physical activity, and stress levels.
Cardiovascular and metabolic health issues are a concern, with 5 (9.4%) participants (11.8%) reporting hypertension, and 3 (5.7%) experiencing cardiac disease. These statistics highlight the long-term health risks associated with shift work, potentially exacerbated by factors such as irregular sleep and stress.
Social and relational impacts are also significant. A considerable number of respondents, 25 (47.2%), report feeling dissatisfied with their social interactions due to shift work. This dissatisfaction can stem from disrupted social schedules and reduced opportunities for social engagement, affecting overall quality of life.
Mental health metrics indicate that 29 (54.7%) respondents (35.3%) experience increased stress, and
16 (30.2%) report heightened nervousness and anxiety. Additionally, 14 (26.4%) participants (25.5%) indicate feelings of irritability, while 39 (73.6%) believe their quality of life is compromised.
The prevalence of these issues underscores the mental health challenges associated with shift work. Burnout is another critical concern, with 26 (49.1%) respondents (27.5%) reporting feelings of burnout. This high rate of burnout highlights the cumulative effects of stress, fatigue, and dissatisfaction associated with shift work.
Behavioral Changes and Job Satisfaction
Behavioral changes due to shift work are also evident. Notably, 5 respondents 9.4% have started smoking as a coping mechanism, reflecting a potential adverse response to the stress of shift work. This data point is important for understanding how shift work can influence unhealthy coping behaviors.
Job satisfaction with shift work varies significantly among respondents. While 33 (62.3%) individuals (31.4%) express satisfaction with their shift work, 20 (37.7%) disagree, indicating a substantial level of dissatisfaction. This disparity suggests that while some individuals may adapt to or even prefer shift work, a significant portion of healthcare professionals finds it challenging and unsatisfactory.
The data analysis reveals a complex picture of the impact of shift work on healthcare professionals. The findings highlight a range of health issues, from sleep disorders and weight changes to cardiovascular conditions and mental health challenges. Additionally, the impact on social interactions and job satisfaction underscores the broader implications of shift work on overall well-being. This comprehensive analysis provides valuable insights into the multifaceted effects of shift work, offering a foundation for further research and potential interventions aimed at mitigating its negative impact.
Results
This section presents the findings from the survey of 53 healthcare professionals regarding the impact of shift work on their health and well-being. The results are detailed across several dimensions, including demographic characteristics, health-related issues, behavioral changes, and job satisfaction. Each aspect is analyzed to provide a comprehensive understanding of how shift work affects various facets of the respondents' lives.
Demographic Characteristics
Gender Distribution
Out of the 53 participants, 20 (37.7%) are male and 33 (62.3%) are female. This gender distribution allows for a nuanced examination of how shift work impacts different genders. Preliminary analysis indicates no significant differences in the overall experience of shift work between males and females. However, further investigation into gender-specific challenges, such as balancing shift work with family responsibilities or differing health impacts, might reveal more detailed insights.
Marital Status
The survey results show that 30 (56.6%) respondents (52.9%) are married, while 23 (43.3%) are single. Analyzing the impact of marital status on shift work experiences reveals that married individuals may face unique challenges, such as managing family responsibilities alongside irregular work hours. Conversely, single respondents may experience different social and relational dynamics. The data suggests that married respondents report higher levels of dissatisfaction with their social interactions and increased stress, potentially due to conflicts between shift work and family obligations.
Age Distribution
Respondents are categorized into three age groups: 20-25 years (11 (20.8%) participants, 33.3%), 26-30 years (17 (32.1%) participants, 35.3%), and over 31 years (25 (47.2%) participants, 31.4%). The data indicates that older respondents (more than 31 years) are more likely to report health issues such as sleep disorders and appetite changes compared to younger age groups. This finding suggests that older professionals might be more vulnerable to the disruptions caused by shift work, possibly due to the impact of the working shifts increase with time and age.
Nationality
The sample includes 20 (37.7) Saudi respondents (58.8%) and 33 (62.3%) non-Saudi respondents (41.2%). Differences in shift work experiences between Saudi and non-Saudi professionals could be influenced by cultural factors and varying national healthcare regulations. The data reveals that non-Saudi respondents report slightly higher levels of stress and dissatisfaction with shift work compared to their Saudi counterparts. This disparity might be attributed to differences in support systems, cultural norms, and personal coping mechanisms.
Health-Related Issues
Sleep Disorders
A significant portion of the respondents, 24 (45.3%), report experiencing sleep disorders. The nature of these disorders varies, with many participants experiencing difficulties such as oversleeping or undersleeping. These issues are exacerbated by irregular shift patterns, leading to inconsistent sleep schedules and poor sleep quality. For instance, 10 participants (18.8%) specifically report problems with falling asleep, while 7 (13.2%) experience frequent awakenings during sleep. These disruptions can lead to chronic fatigue, impacting overall health and job performance.
Appetite Changes
The survey reveals notable changes in appetite among participants. 20 (37.7%) respondents (27.5%) report a poor appetite during shifts, while 25 (47.2%) experience an increased appetite. These changes in appetite are likely related to irregular eating patterns associated with shift work. Poor appetite can result in inadequate nutrition, while increased appetite might lead to unhealthy eating habits, contributing to weight gain and metabolic issues. The data suggests that irregular work hours disrupt normal eating routines, which can have broader implications for health.
Weight Changes
Weight changes are another significant concern, with ten participants 16 (30.2%) reporting weight gain and 23 (43.4%) experiencing weight loss. These variations in weight may be attributed to irregular eating patterns, altered physical activity levels, and stress associated with shift work. Weight gain can be linked to increased appetite and reduced physical activity, while weight loss might result from poor appetite and inconsistent meal times. Understanding these changes is crucial for addressing the long-term health implications of shift work.
Cardiovascular and Metabolic Health
Cardiovascular and metabolic health issues are prevalent among respondents. five (9.4%) participants (11.8%) report hypertension, and three (5.7%) experience cardiac disease. These conditions highlight the potential long-term health risks associated with shift work, such as increased stress, poor diet, and disrupted sleep. The data suggests that shift work may contribute to the development or exacerbation of these health issues, underscoring the need for targeted interventions to mitigate these risks.
Behavioral Changes
Smoking Habits
The survey reveals that five respondents (9.4%) have taken up smoking as a coping mechanism due to the stress and disruptions associated with shift work. Smoking can be a response to stress and may further exacerbate health issues related to shift work, such as cardiovascular diseases and respiratory problems. This finding highlights the need for support programs that address unhealthy coping mechanisms and promote healthier alternatives.
Coping Strategies
In addition to smoking, respondents report a range of coping strategies, including increased caffeine consumption and reliance on stimulants to manage fatigue. These behaviors can have mixed effects on health, potentially providing temporary relief but contributing to long-term issues such as anxiety and gastrointestinal problems. The data suggests that effective coping strategies are essential for managing the demands of shift work and maintaining overall well-being.
Job Satisfaction
Overall Job Satisfaction
The survey data reveals that 33 (62.3%) respondents (31.4%) are satisfied with their shift work, while 20 (37.7%) report dissatisfaction. This percentage (37.7%) level of dissatisfaction indicates that many healthcare professionals struggle with the demands of shift work. Factors contributing to dissatisfaction include disrupted social and family life, health issues, and overall job stress. Addressing these concerns requires a comprehensive approach, including policy changes and support systems that improve work-life balance.
Impact on Quality of Life
A considerable number of respondents, 39 (73.6%), believe that their quality of life is compromised due to shift work. This perception is supported by the reported impacts on health, social interactions. The data suggests that shift work negatively affects various aspects of life, including personal well-being and social relationships. Improving the quality of life for shift workers requires a holistic approach that considers health, job satisfaction, and personal fulfillment.
Burnout
Burnout is a critical issue, with 26 (49.1%) respondents (27.5%) reporting feelings of burnout due to shift work. This high rate of burnout reflects the cumulative effects of stress, fatigue, and job dissatisfaction. Burnout can lead to decreased job performance, increased absenteeism, and a higher turnover rate. Addressing burnout involves implementing strategies to manage stress, improve working conditions, and support mental health.
Correlations and Insights
Health Metrics and Job Satisfaction
Analysis of the correlations between health metrics and job satisfaction reveals that individuals reporting sleep disorders, appetite changes, and weight fluctuations are more likely to express dissatisfaction with their shift work. Similarly, those experiencing increased stress, nervousness, and burnout report lower levels of job satisfaction. These correlations underscore the interconnected nature of health and job satisfaction, highlighting the need for interventions that address both health issues and work-related stressors.
Impact of Age and Gender on Health
The data shows that younger respondents are more likely to experience sleep disorders and appetite changes, while older respondents report more consistent health outcomes. Gender-based differences in health impacts are less pronounced but may still be relevant for specific health issues. For instance, females report higher levels of stress and dissatisfaction with social interactions compared to males. Understanding these differences can help tailor interventions to address the unique needs of different demographic groups.
National Differences
Comparisons between Saudi and non-Saudi respondents reveal that non-Saudi professionals experience higher levels of stress and job dissatisfaction. This difference may be attributed to varying support systems and cultural expectations related to shift work. Further research is needed to explore these cultural factors and their impact on shift work experiences.
The results of the survey provide a comprehensive overview of the impact of shift work on healthcare professionals. Key findings include significant health issues such as sleep disorders, appetite changes, and weight fluctuations, as well as increased stress, burnout, and job dissatisfaction. The data highlights the need for targeted interventions to address these challenges and improve the overall well-being of shift workers. Future research should focus on developing strategies to mitigate the negative effects of shift work and enhance support systems for healthcare professionals.
|
Demographic Characteristic |
Category |
Frequency (n=53) |
|
Gender |
Male |
20 |
|
|
Female |
33 |
|
Marital Status |
Married |
30 |
|
|
Single |
23 |
|
Age |
20-25 years |
11 |
|
|
26-30 years |
16 |
|
|
Over 31 years |
25 |
|
Nationality |
Saudi |
20 |
|
|
Non-Saudi |
33 |
|
Health-Related Issue/Behavior |
Category |
Frequency (n=53) |
|
Sleep Disorders |
Reported Sleep Disorders |
24 |
|
Appetite Changes |
Poor Appetite |
20 |
|
|
Increased Appetite |
25 |
|
Weight Changes |
Weight Gain |
16 |
|
|
Weight Loss |
36 |
|
Cardiovascular Health |
Hypertension |
5 |
|
|
Cardiac Disease |
3 |
|
Job Satisfaction |
Satisfied with Shift Work |
33 |
|
|
Dissatisfied with Shift Work |
20 |
Figure 1: Demographic Characteristics
Figure 2: Health Related Issues and Behavioral Changes
Recommendations
1. Implement Flexible Scheduling: One of the primary issues identified is the negative impact of rigid and unpredictable shift schedules on healthcare professionals' well-being. To mitigate this, hospitals and healthcare facilities should consider implementing more flexible scheduling systems. This could include allowing staff to have input into their schedules, offering a mix of day and night shifts that align better with individual preferences, and providing the option for part-time work or job sharing. Flexible scheduling can help reduce burnout, improve job satisfaction, and ultimately enhance the quality of patient care.
2. Enhance Support Systems: The survey highlighted the need for robust support systems within healthcare facilities. It is crucial to establish comprehensive mental health and counseling services specifically tailored for shift workers. Regular workshops on stress management, resilience building, and mindfulness can also be beneficial. Creating peer support groups where staff can share their experiences and coping strategies can foster a supportive work environment and reduce feelings of isolation.
3. Improve Work Environment: Addressing the physical and psychological demands of shift work requires an improved work environment. This includes ensuring that workspaces are ergonomically designed to reduce physical strain and providing amenities such as quiet rest areas for breaks. Additionally, enhancing lighting and ventilation in workspaces can help mitigate the adverse effects of working during night shifts. Implementing policies that encourage regular breaks and short naps can also improve alertness and performance during long shifts.
4. Promote Healthy Lifestyles: Healthcare facilities should actively promote healthy lifestyle choices among their staff. This can be achieved by providing access to nutritious meals and snacks during all shifts, offering on-site fitness facilities or gym memberships, and organizing wellness programs that focus on physical activity, healthy eating, and adequate sleep. Educational campaigns on the importance of sleep hygiene and strategies to improve sleep quality can also be beneficial.
5. Regular Monitoring and Feedback: To ensure the effectiveness of any implemented changes, it is essential to establish a system for regular monitoring and feedback. This could involve conducting periodic surveys to gauge staff satisfaction with shift schedules and work conditions, as well as assessing the impact on their mental and physical health. Regular feedback sessions where staff can voice their concerns and suggestions can help in continuously refining and improving policies and practices.
6. Increase Staffing Levels: A recurring theme in the survey responses was the impact of understaffing on workload and stress levels. To address this, healthcare facilities should prioritize hiring additional staff to ensure adequate coverage across all shifts. This not only helps distribute the workload more evenly but also allows for more flexible scheduling options. Increasing staffing levels can reduce the pressure on existing staff, decrease the likelihood of errors, and improve overall patient care quality.
7. Encourage Professional Development: Providing opportunities for professional growth and development can enhance job satisfaction and reduce burnout. Healthcare facilities should offer regular training programs, workshops, and courses that enable staff to advance their skills and knowledge. Supporting staff in pursuing further education and certifications can also be motivating. Additionally, creating clear career progression pathways within the organization can help staff feel valued and invested in their roles.
8. Implement Technology Solutions: Leveraging technology can help mitigate some of the challenges associated with shift work. For instance, implementing advanced scheduling software that takes into account staff preferences and availability can streamline the scheduling process and reduce conflicts. Additionally, using telehealth solutions where feasible can allow some tasks to be performed remotely, providing more flexibility for staff. Investing in electronic health records (EHR) systems that are user-friendly and reduce administrative burden can also improve efficiency and reduce stress.
9. Foster a Culture of Appreciation: Acknowledging and appreciating the hard work of shift workers is vital in maintaining morale and motivation. Regular recognition programs, such as employee of the month awards, appreciation events, and public acknowledgment of achievements, can make staff feel valued. Creating a culture where feedback is encouraged and achievements are celebrated can significantly improve job satisfaction and loyalty.
10. Conduct Further Research: The findings from this survey indicate the need for ongoing research into the impacts of shift work on healthcare professionals. Further studies should explore the long-term effects of shift work on health and well-being, as well as the effectiveness of different intervention strategies. Collaborating with academic institutions and research organizations can provide valuable insights and help develop evidence-based best practices for managing shift work in healthcare settings.
Conclusion
The study has revealed significant insights into the impact of shift work on healthcare providers. The data analysis showed that shift work is closely associated with various health issues, including sleep disturbances, cardiovascular problems, and mental health challenges. The study also found that shift work negatively affects job satisfaction, work-life balance, and social relationships. These findings align with previous research, confirming that shift work presents substantial risks to the well-being of healthcare providers.
The implications of this study are far-reaching. For healthcare institutions, the results underscore the urgent need for organizational changes to mitigate the adverse effects of shift work. Implementing flexible scheduling, providing mental health support, and promoting healthier lifestyle choices are not just recommendations but essential steps in ensuring the sustainability of healthcare services.
For policymakers, the study highlights the need for regulations that protect the health of shift workers and promote fair working conditions.
This study contributes to the growing body of literature on the effects of shift work, particularly within the context of healthcare in Riyadh. By providing empirical evidence on the health impacts of shift work, this research offers valuable insights for both academics and practitioners. It adds to the understanding of how shift work influences not just physical health but also mental well-being and job satisfaction, offering a comprehensive view of the challenges faced by healthcare providers.
While this study has provided significant findings, it also opens avenues for future research. Future studies could explore the long-term effects of shift work on healthcare providers, investigate the impact of shift work on patient care quality, or examine the effectiveness of different interventions in mitigating the negative impacts of shift work. Additionally, expanding the research to include a larger and more diverse sample could provide a broader understanding of the issue.
The health and well-being of healthcare providers are critical to the effective functioning of healthcare systems. Addressing the challenges posed by shift work is essential for safeguarding the health of these essential workers and ensuring that they can continue to provide high-quality care to patients. This study has highlighted the need for urgent action and has provided a foundation for future research and policy development in this important area.
References
Please View attached pdf to view all references
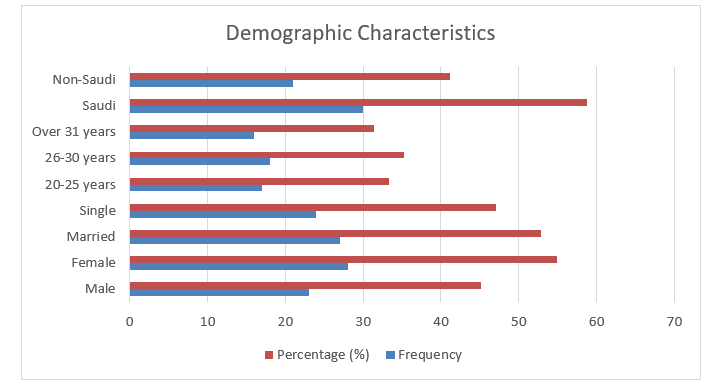
Figure 1
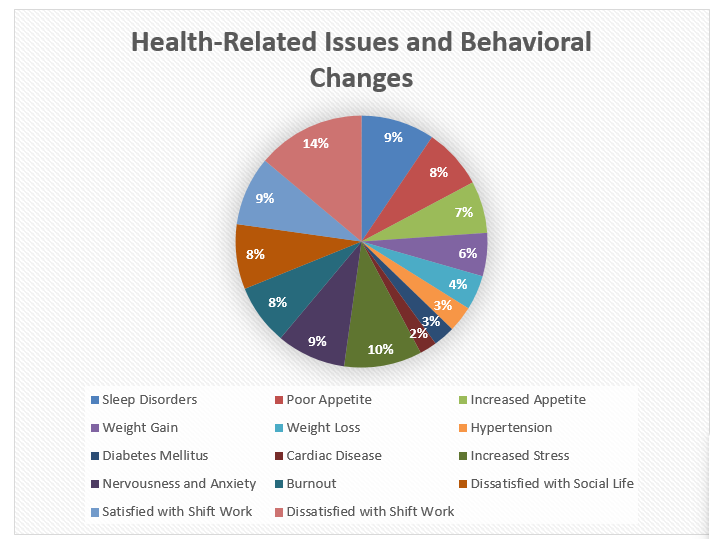
Figure 2
