An Analysis of Slipped Capital Femoral Epiphyses in the General Population
An Analysis of Slipped Capital Femoral Epiphyses in the General Population
Kassem El Houcheimi *
*Correspondence to: Kassem El Houcheimi, FACS, MBA, Orthopedic surgeon, Clemenceau Medical Center Dubai.
Copyright
© 2024: Kassem El Houcheimi. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 28 August 2024
Published: 05 Sept 2024
Abstract
Objective: Slipped epiphysis femoral (SCFE) is the most common abdominal pain in children aged 9–15 years. In the Sex Survey, we analyzed pre- and postoperative photographs, medical records, demographic data, falls, and procedures for every child with SCFE in Sweden from 2007 to 2013. Surgery. 162 girls, mean age 11.7 (7.2–15.4) years, 217 boys, mean age 13 (3.8–17.7) years. The mean annual incidence was 4.4/10,000 in girls and 5.7/10,000 in boys aged 9–15 years. 56% of girls and 76% of boys were overweight or obese. Abdominal/groin pain and knee pain were presenting as the first symptom in 66% of children. At first presentation, 7% of children had bilateral SCFE. The remaining 21% of children subsequently developed contralateral spondylolisthesis.
Femoral neck osteotomies were performed in 11 hips. The male-to-female ratio is lower than previous regional figures for Sweden. Being overweight or obese is a significant factor in boys with SCFE, but less so in girls. The initial symptom, knee pain, may lead to a delay in diagnosis. Most hospitals in Dubai treat <2 children per year.
Keywords: Epidemiology, Slipped capital femoral epiphysis, Incidence, Hip, Slipped upper femoral epiphysis
An Analysis of Slipped Capital Femoral Epiphyses in the General Population
Introduction
Slipped capital femoral epiphysis (SCFE) is the most common hip injury in children aged 9–15 years (1,2). Identified biomechanical factors include obesity, increased femoral retroversion, and increased epiphyseal plate inclination, all of which increase femoral epiphyseal plate shear forces . Diseases associated with endocrine disorders such as hypothyroidism, hypogonadism, and hypopituitarism. Children with osteodystrophy secondary to renal failure or those receiving pelvic radiation therapy are also thought to be at increased risk of developing SCFE. Separation of the epiphysis and metaphysis of the proximal femur. The femur usually rotates and extends laterally, while the epiphysis remains in the acetabulum. The duration of symptoms has been associated with increasing and decreasing weight [3,4].
More severe forms are associated with increased pain and increased mobility. Total population of the country . Report events related to race and sex. Seasonal variations have also been described, but their role in the etiology of SCFE is unclear. The male/female ratio has been reported to range from 1.1:1 to 4.1:1. Previous national population reports have relied on data from national registries.
The aim of this study was to describe the epidemiology of SCFE and to determine the characteristics of children, the type and extent of SCFE and the surgical procedures performed. (2) Knee pain as a symptom makes a difference when compared to abdominal/groin pain
There is a difference in the incidence of low back pain when compared to the first and the first contact with health services (5) the age of diagnosis has not changed compared to previous regional epidemiological data is being overweight or obese is assumed to be the most important SCFE Childhood Tics.
Methods
This is a prospective study covering the entire population of children treated for SCFE at the hip index in Sweden between 2007 and 2013. All children were reported regularly to the National Quality Registry by one of the authors (BH). The person's personal identification number was recorded on the lumbar part of the index finger while the SCFE was being studied. Exclusion criteria were: SCFE due to exertional or septic hip arthritis. To maintain the integrity of the study, we re-annotated the personal data of the Swedish National Board of Health and Welfare and compared our data with patients registered with the Swedish National Board of Health and Welfare. All hospitals recorded all admissions using diagnosis codes (WHO classification ICD-10) and medical codes according to the Statutory Surgery Committee, NCSP guidelines NOMESCO - NCSP surgical procedure classification (NOMESCO - Nordic Surgical Classification).
The number of children aged 9–15 who had a Swedish personal number at the start of the study was slightly higher for girls and boys, see Table 1. To calculate the mean annual incidence of SCFE, the mean number of children aged 9–15 during the study period was used as the mean risk population. In calculating the annual average, we excluded five girls under 9 years of age, boys under 3.8 years of age and four boys under 16 years of age. br> Radiographs were taken from all patients and continued to be examined. Missing information was added by contacting the hospital or family members.
A follow-up was performed 24 months later by a contact person at each hospital to determine whether additional surgery had been performed on the contralateral hip of the SCFE.
About: Gender, place of residence, type of initial symptom, first physician, duration of symptoms, age at diagnosis, presence or absence of SCFE pain, type of surgical treatment, reduction maneuvers [6] , implants used, and whether prophylactic surgery had been performed on the contralateral hip. For osteotomies, we recorded whether femoral head realignment surgery had been performed with or without hip surgery [7]. Other specific treatments recorded were open reduction and internal repair according to Parsch and whether there was a joint causing unstable SCFE. This was not always measured and therefore not reported to us. We then asked families to sign additional consent forms so that we could obtain the school nurse's progress. We accept age-adjusted BMI values from the 12 months before or after the initial hip replacement surgery according to Karlberg 2001. As healthcare providers, we use the medical history information provided at the initial SCFE admission. Total duration of symptoms, measured in months, is the time from symptom onset to start of surgery. Surgery performed on the first day of symptoms equals 0 months; 1 day but ≤1 week equals 0.25 months; > 1 week but ≤2 weeks equals 0.50 months; >2 weeks but ≤3 weeks equals 0.75 months, etc.
Among children with bilateral SCFE at presentation, the hip index was the hip with the longest symptom duration. When symptoms were equal in both hips, we selected the hip with the largest hip angle with initial SCFE. For bilateral data, information from the index hip was used only, except for the comparison of first and second slipped capital femoral epiphyses. The measurement of the angle is calculated using the femoral calcar method of the Lauenstein view (Fig. 1). If obtaining a billing-side view, use the Billing method [8] (Fig. 2)). If the lateral view cannot be obtained due to instability of the SCFE, the Southwick's head axis angle HSA is used in the anteroposterior (AP) view. Cut-off values for the SCFE are not described in the literature for the use of the HSA in AP monitoring. Therefore, we use the following criteria: HSA of the AP view "110°" and a broken Klein line [9,10] and Clinical appearance/symptoms of hip disease such as chest claudication or Gin/symptoms of abdominal pain. An HSA of "110°" on the AP view is classified as severe. , the protrusion of the lateral femoral epiphysis is increased relative to the lateral femoral neck (Klein line). In unilateral valgus SCFE, an increase in HSA compared to the contralateral hip has also been noted .Used in cases of stable or unstable SCFE (inability to walk with two crutches). Data from medical admission records or descriptions of surgical procedures were used to classify clinical sites.). Continuous data are reported as mean with minimum and maximum values. Discrepancy data are reported as frequency and/or percentage. For non-significant evaluation of two independent groups, Mann-Whitney U test was used. To compare the ratio of two independent groups, we used cross-tabulations and chi-square test. When Mann-Whitney U test and Chi-square test were compared with Fisher test, the same results were obtained.
Table 1 Number of girls and boys, 9–15 years old During 2007–2013
|
Year |
2007 |
2008 |
2009 |
2010 |
2011 |
2012 |
2013 |
2007-2013 AVG |
|
Girls |
386372 |
371151 |
357163 |
346664 |
337959 |
336135 |
339852 |
353614 |
|
Boys |
406293 |
390426 |
375523 |
365425 |
357094 |
354890 |
359177 |
372690 |
|
Total |
792665 |
761577 |
732686 |
712089 |
695053 |
691025 |
699029 |
726304 |
Fig. 1 The slip angle measured according to the calcar femorale method (Hansson et al.)1
1 Permission has been obtained to use the figure from Hansson et al. 1988research. It is a kind of multisystem autoimmune ailment involving almost every system in the body. Although immunosuppressive agents have been utilized but very challenging at the same time.Many options of treatments still have intermittent disease flares and remissions (1,2,3).
Fig. 2 The slip angle measured according to the Billing method
Results
Mean annual incidence
A total of 379 children suffered from a first SCFE between 2007 and 2013. Thirty-five of these cases were identified retrospectively from the Swedish National Patient Register. The mean number of children aged 9 to 15 years in Sweden from 2007 to 2013 was 726,304 (353,614 girls and 372,690 boys). In calculating the mean annual incidence in children aged 9 to 15 years, we excluded five girls and one boy under 9 years of age and four boys under 16 years of age.
The annual incidence of SCFE is 4.4 per 10,000 girls and 5.7 per 10,000 boys
Primary SCFE was seen in 162 girls aged 9-15 years, with a mean age at diagnosis of 11.7 years (7.2â ) <15.4), a mean age of 11.6 217 boys aged 13.0 (3.8-17.7), a mean age of 12.9 The youngest son (3.8 years old) has microcephaly and cerebral palsy. 81% of the population.
74 of 131 girls (56%) and 133 of 176 boys (76%) are overweight or obese. Most children with abdominal/groin pain are the first symptoms, but mixed symptoms and knee pain may also occur. 0 to 48 months; missing data, n = 5). In 44 children (15 girls and 29 boys) with knee pain as the main symptom, the mean duration was 4 months (0.5 to 18 months), while in 250 children with hip pain, mild abdominal/groin pain was the main symptom. 2-month interval (0.25 to 48 months). Knee and hip/groin pain Mean duration of symptoms as the first symptom was significant for the entire population (p = 0.004), but when the same analysis was done separately for boys and girls the difference was statistically significant only for boys (p = 0.004). Conduct surveys of medical professionals. Initially, 85 children went to the hospital's emergency room.
The rest of the children are seen on an outpatient basis, usually by a pediatrician, a doctor from the school health department, or a physiotherapist or doctor/physician.), when he first consulted a doctor, a stomach infection was suspected and he was referred for a stomach examination. Of the 44 children (27%) whose main symptom was knee pain, 12 (27%) were referred for a hip radiograph at the first visit. Of 250 children with abdominal or groin pain as the primary symptom, 180 (72%) were referred for pelvic radiography at the first visit. There was a significant difference in the number of children with knee pain referred for radiographic hip examination compared to children with abdominal/groin pain as the first symptom (p = 0.033). was associated with an increase in mean time (Figure 3).
Among the 89 major errors; 36 were girls aged 12 (9-15) on average and 53 were girls aged 13 (10-16) on average. Of these, 66 were girls aged 12 (8-14) on average and 59 were boys aged 13 (9-16). Both cases of spondylolisthesis were classified as valgus SCFE. In boys aged 12 (4-17). Both spondylolisthesis were valgus SCFE. Four children were excluded due to symptoms lasting longer than 24 months. No records were found to identify their original address.
According to statistics, 64% of the children live in cities and 35% in the regions. 26% of the children (0-19 years) live in rural areas. Data on age-adjusted body mass index were available for the groups.
76% of boys and 56% of girls are overweight or obese. Intermediate glides are fixed by screw or pin fastening. Immobilization with an implant allows further development of the femoral neck; Hansen clasps (Figure 4) or screws with ultra-short thread lengths are used in more than 90% of patients for index hip surgery with prophylactic pinning. Due to the difficulty of finding the correct access, 12 of the index hip percutaneous surgeries had to be expanded to more invasive surgical methods.
Fig. 3 Severity of the slip in relation to duration of symptoms (missing data, n = 5)1 . 1 Outliers with duration of symptoms >24 months:. Mild (n = 1). Moderate (n = 1). Severe (n = 2)
Fig. 4 Seasonal variation for the study period 2007–2013 (missing data, n = 5)
Unstable SCFE Sixty hips were unstable at surgery: 40 were severe and 20 had mild or moderate symptoms (one had valgus SCFE). Of the 60 patients with unstable SCFE, 2 underwent open reduction and internal repair and 3 underwent surgical resection with commercial reconstruction, all of whom had severe SCFE. continue working. Of these, 9 patients had mild or slight displacement and 22 patients had severe displacement. Contralateral hip
Sexual fixation (43%). We found a mean interval of 10.8 months between index surgery and contralateral hip surgery for the 43 children with subsequent contralateral hip displacement. The second largest interval, excluding the 59.8-month outlier period, was 24 months. The child, who was only 0.5 months apart, had no symptoms but had an external X-ray examination at the initial presentation. The child was referred to hospital only two weeks later and now had symptoms in the contralateral hip and was diagnosed with contralateral SCFE. Twelve of the 43 contralateral spondylolisthesis were diagnosed more than a year after the index spondylolisthesis. br>> 30.6 months, mean 26.9 months (range 6.5-93 months).
Secondary joint replacements of 46 children were followed between 12 and 24 months. Fifteen children, all with radiographic evidence of epiphyseal closure, underwent second hip replacement in less than 12 months. br>Index Hip Surgery. Another son died during hip surgery at 22 months. 17.7) years. For 201 children not treated with prophylactic surgery, the mean age at diagnosis of SCFE at hip measurement was 12.1 (8.4–14.7) years for girls 13.4 (3) years for boys. .8-16.7). . >The hospital changed the treatment and sent the child with SCFE to surgery. Between 2007 and 2013, 20 hospitals treated an average of more than 1 child with SCFE per year, 4 treated an average of more than 2 children per year, and 3 treated an average of more than 3 children per year.
|
Disorder Number |
|
Neurocognitive disorder (ADD, ADHD, Autism) 15 Thyroid insufficiency 2 Down’s syndrome 2 Other chromosome abnormalities 3 Hypopituitarism 1 Early onset of puberty 1 Late onset of puberty 1 Adrenoleukodystrophy 1 Short stature (treated with growth hormone) 1 Vitamin D deficiency 1 Diabetes mellitus 1 Osteopetrosis 1 Marfan’s syndrome 1 Cerebral palsy (with concomitant microcephaly) 1 Embryonal rhabdomyosarcoma (irradiation to pelvic area) 1 Fibrous dysplasia of proximal femur 1 |
Table 2 Co-morbidity
Table 3 Method of treatment related to severity of SCFE
Fig. 5 Implant for fixation that will allow for further growth of the femoral neck (Hansson pin)
Discussion
This study is the first prospective cohort study to describe the epidemiology of scoliosis and fracture (SCFE) based on a total national population. The study reached 100% completeness using the definition of the proportion of all children treated for SCFE that were registered in the population covered by the Swedish National Patient Register (NPR). The median age at diagnosis was similar to previous studies, with a gradual decrease in age at onset of SCFE observed during the twentieth century [11,12].
The male-to-female ratio was 1.3:1, with 76% of boys having overweight or being obese, while 56% had this for girls. The average annual incidence calculated in this study was for children aged 9-15 years old in Sweden during the period 2007–2013. There seems to be an increase in incidence for girls, but not for boys. The severity of the slip was correlated with the duration of symptoms[13].
The most common diagnosis in this study was neuropsychiatric disorders (15 of 379), which might have a different risk behavior in recreational activities that could contribute to this situation[14,15]. All children below 2 years in Sweden are routinely offered supplemental Vitamin D and parents are encouraged to allow their children to be exposed to the sun, which might explain the very low number of co-existing Vitamin D deficiency in this cohort.
In the present study, 43% of the contralateral hips had a prophylactic fixation performed, with the rationale for a programme where prophylactic fixation is always performed being controversial. Most hospitals in Sweden where prophylactic fixation is not routinely performed have a follow-up program with repeat radiographic examinations of both hips until physeal closure of the proximal femur has occurred[16,17,18].
The number of hospitals in Sweden treating SCFE has decreased from 39 to 34 since January 2007, with only three hospitals treating on average >3 children per year for SCFE in the index hip. Continuous education will be of utmost importance for surgeons in hospitals that annually receive a low volume of children with SCFE [19,20].
Conclusion
The annual incidence of proximal femoral edema (SCFE) is 4.4 per 10,000 girls and 5.7 per 10,000 boys aged 9-15. Most children are treated with percutaneous pin or screw fixation, with prophylactic fixation of the contralateral hip performed in 43% of cases. Boys with SCFE are more likely to be overweight, while girls are less affected. Knee pain can delay diagnosis. Hospitals should implement a program with regular radiographic follow-up until the closure of the proximal femoral physis is verified. Despite reduced surgery, most hospitals in Sweden treat less than two children per year.’
References
1. Loder RT. The demographics of slipped capital femoral epiphysis. An international multicenter study. Clin Orthop Relat Res. 1996;322:8–27.
2. Lehmann CL, Arons RR, Loder RT, Vitale MG. The epidemiology of slipped capital femoral epiphysis: an update. J Pediatr Orthop. 2006;26(3):286–90.
3. Galbraith RT, Gelberman RH, Hajek PC, Baker LA, Sartoris DJ, Rab GT, Cohen MS, Griffin PP. Obesity and decreased femoral anteversion in adolescence. J Orthop Res. 1987;5(4):523–8.
4. Gelberman RH, Cohen MS, Shaw BA, Kasser JR, Griffin PP, Wilkinson RH. The association of femoral retroversion with slipped capital femoral epiphysis. J Bone Joint Surg Am. 1986;68(7):1000–7.
5. Pritchett JW, Perdue KD. Mechanical factors in slipped capital femoral epiphysis. J Pediatr Orthop. 1988;8(4):385–8.
6. Loder RT, Wittenberg B, DeSilva G. Slipped capital femoral epiphysis associated with endocrine disorders. J Pediatr Orthop. 1995;15(3):349–56.
7. Wells D, King JD, Roe TF, Kaufman FR. Review of slipped capital femoral epiphysis associated with endocrine disease. J Pediatr Orthop. 1993;13(5):610–4.
8. Wilcox PG, Weiner DS, Leighley B. Maturation factors in slipped capital femoral epiphysis. J Pediatr Orthop. 1988;8(2):196–200.
9. Loder RT, Hensinger RN. Slipped capital femoral epiphysis associated with renal failure osteodystrophy. J Pediatr Orthop. 1997;17(2):205–11.
10. Loder RT, Hensinger RN, Alburger PD, Aronsson DD, Beaty JH, Roy DR, Stanton RP, Turker R. Slipped capital femoral epiphysis associated with radiation therapy. J Pediatr Orthop. 1998;18(5):630–6.
11. Libshitz HI, Edeiken BS. Radiotherapy changes of the pediatric hip. AJR Am J Roentgenol. 1981;137(3):585–8.
12. Jerre R: Physiolysis of the hip : epidemiology, diagnosis and long-term follow-up. Göteborg; 1995.
13. Loder RT. Unstable slipped capital femoral epiphysis. J Pediatr Orthop. 2001;21(5):694–9.
14. Carney BT, Weinstein SL, Noble J. Long-term follow-up of slipped capital femoral epiphysis. J Bone Joint Surg Am. 1991;73(5):667–74.
15. Carney BT, Weinstein SL. Natural history of untreated chronic slipped capital femoral epiphysis. Clin Orthop Relat Res. 1996;322:43–7.
16. Jerre R, Karlsson J, Romanus B, Wallin J. Does a single device prevent further slipping of the epiphysis in children with slipped capital femoral epiphysis? Arch Orthop Trauma Surg. 1997;116(6–7):348–51.
17. Loder RT, Starnes T, Dikos G, Aronsson DD. Demographic predictors of severity of stable slipped capital femoral epiphyses. J Bone Joint Surg Am. 2006;88(1):97–105.
18. Kocher MS, Bishop JA, Weed B, Hresko MT, Millis MB, Kim YJ, Kasser JR. Delay in diagnosis of slipped capital femoral epiphysis. Pediatrics. 2004; 113(4):e322–5.
19. Schur MD, Andras LM, Broom AM, Barrett KK, Bowman CA, Luther H, Goldstein RY, Fletcher ND, Millis MB, Runner R, et al. Continuing Delay in the Diagnosis of Slipped Capital Femoral Epiphysis. J Pediatr. 2016;
20. Ordeberg G, Hansson LI, Sandstrom S. Slipped capital femoral epiphysis in southern Sweden. Long-term result with closed reduction and hip plaster spica. Clin Orthop Relat Res. 1987;220:148–54.
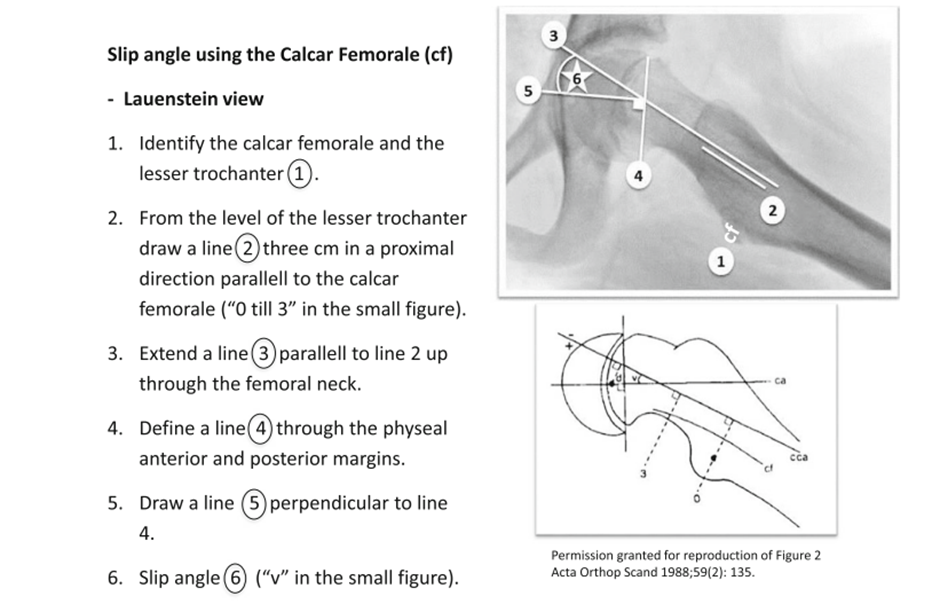
Figure 1
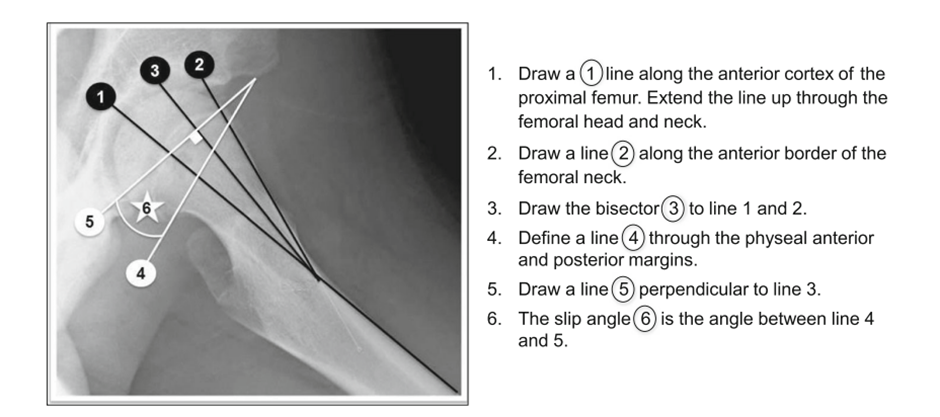
Figure 2
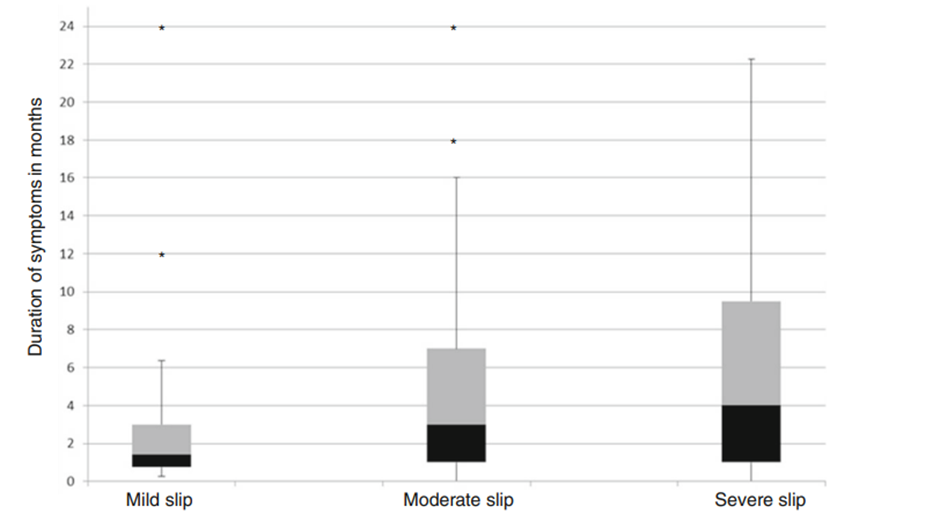
Figure 3
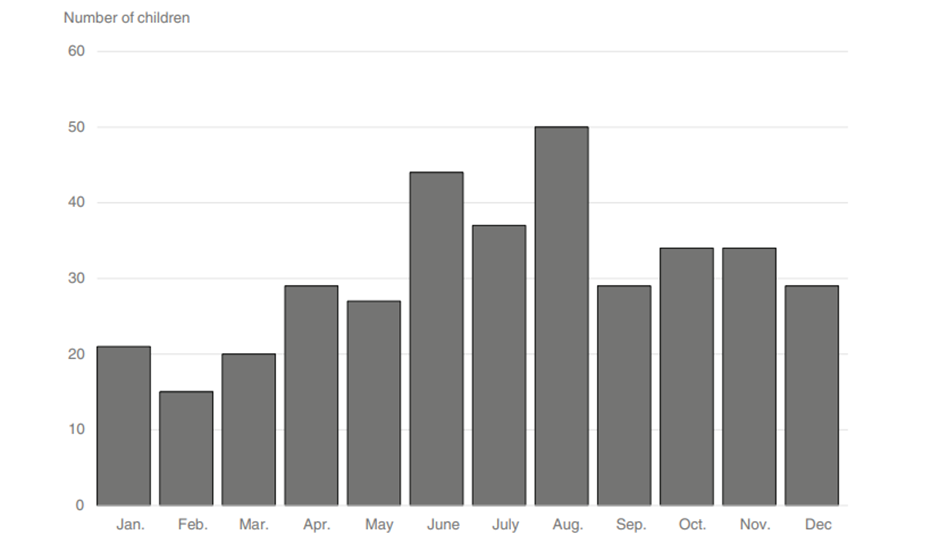
Figure 4
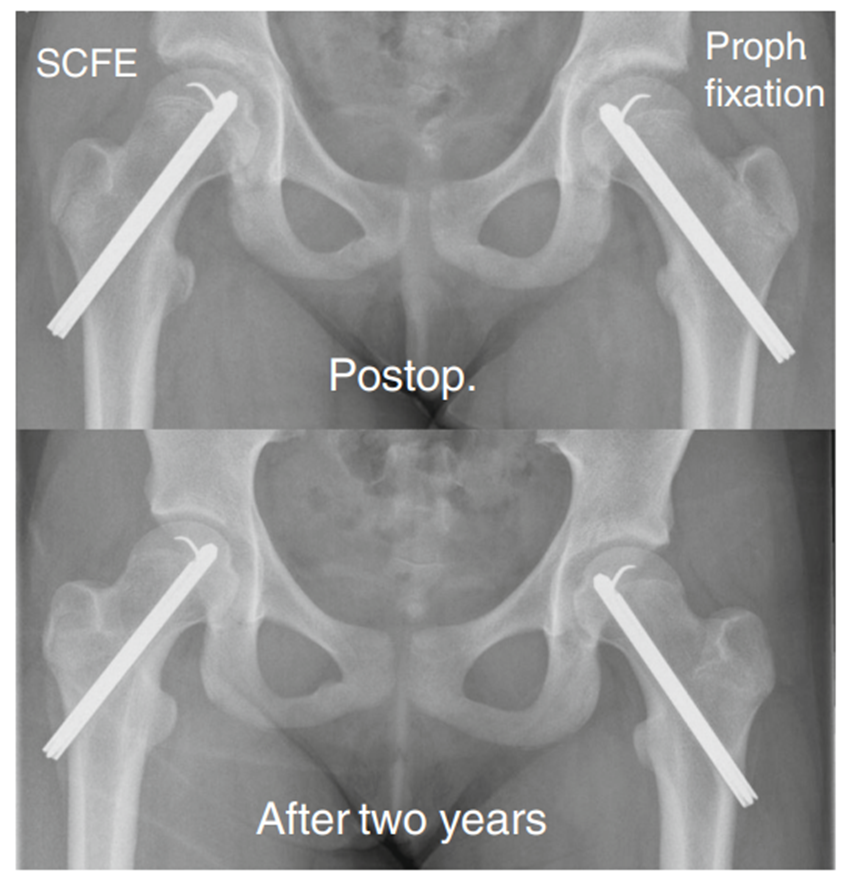
Figure 5
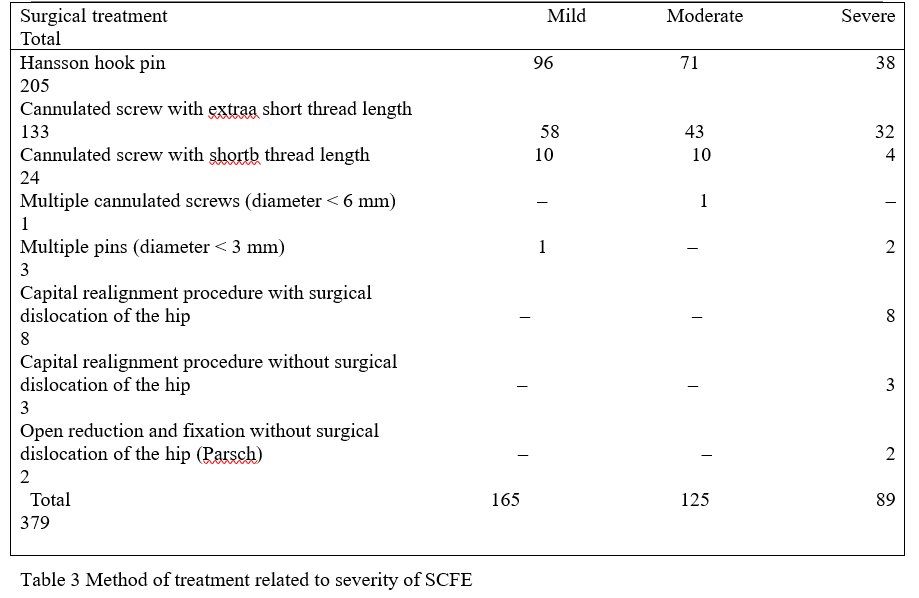
Figure 6
