Congenital Hypothyroidism
Congenital Hypothyroidism
Dr.Maria Rosa Finozzi*, Nadia Arguiñarena1, Beatriz Mendoza2
1. Nadia Arguiñarena - Resident 2 year, Clinic of Endocrinology and Metabolism UdelaR.
2.Beatriz Mendoza -- Professor at the UdelaR Endocrinology and Metabolism Clinic. Director of the Service of Endocrinology Pediatric UdelaR, CHPR. Medical Endocrinologist holder of CRENADECER.
*Correspondence to: Adj. Prof. Dr. Maria Rosa Finozzi, Specialist in Endocrinology and Metabolism, President of the Uruguayan Society of Endocrinology and Metabolism of Uruguay (SUEM), HPR Pediatric Endocrinology Reference, Head of Endocrinology, Diabetes and Metabolism Service, CASMU IAMC.
Copyright
© 2024 Dr.Maria Rosa Finozzi. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 17 Aug 2024
Published: 09 Sep 2024
Congenital Hypothyroidism
Aim
Know the clinical manifestations, diagnostic aspects, treatment and repercussions on untreated patients, with special focus on neonatal screening.
Introduction and Epidemiology
He hypothyroidism congenital (HC) is a endocrinopathy, being the major cause of preventable cognitive disability in newborns (NB). For this reason, and because owns a course asymptomatic in the R.N., HE they have implemented different techniques of screening, since early detection and treatment have a significant effect on the forecast short and long term of the patient.
In Uruguay, he screening of hypothyroidism congenital is mandatory, by he decree 183/994 on September 21, 1994. The incidence of the disease in our country is 1:1998.
It is performed by measuring TSH in cord blood at the time of birth. varying the cut-off points used in different areas of the country. The cutting point can vary according to blood is taken from the heel or cord. To the north of the Río Negro the samples were obtained from cord blood that is left to dry on special filter paper, its point of origin being cut 15 Ul/ml. In the south, serum is obtained by centrifuging cord blood, which is consider a TSH value of 25 - 30 mIU/L (1). A result of the investigation above These cut-off values require a second serum sample (1).
The current screening strategy implemented in Uruguay, that is, the measurement of TSH of screening, No detect central hypothyroidism, thyroxine binding protein deficiency (TBG), hypothyroxinemia or hypothyroidism of the pre-term newborn (PTNB) (1,5).
Historically, the first screening strategy used in the world was in Canada, in the year 1973, he which employed the measurement of T4 in newly born (1). TO leave of that initiative. Other strategies have been implemented, based on the increase in knowledge about pathology, costs and benefits.
Etiology and pathophysiology
Hypothyroidism is caused by a deficiency of the thyroid gland, it may be given by the gland's own deficiency or by a deficiency of the stimulating hormone thyroid gland (TSH), or less frequently by resistance to the action of TSH in the fabrics Diana. When he disorder HE diagnostic then of the birth HE consider congenital hypothyroidism (CH), which can be permanent or transient as well as central, primary or peripheral.
Primary HC corresponds to 95% of the total, the main cause is dysgenesis thyroid by 87%, which in turn is subdivided into ectopia (45%), agenesis (38%) and hypoplasia (3%). The remaining 13% is due to dyshormonogenesis, which can be associated with goiter (1).
Central HC may be due to an isolated TSH deficiency or a combined hormone deficiency. pituitary. He H.C. peripheral, infrequent, HE produces by a flaw in he transport, metabolism or action of thyroid hormones.
The thyroid gland begins to form approximately 24 days after fertilization, by influence of the ways of signaling of the FGF, to leave of a midline endodermal thickening on the floor of the primitive pharynx. Form a small evagination that corresponds to the primordium of the thyroid, a solid mass of cells endodermal.
Embryology:
To the principle, he thyroid primordium is hollow, but in a short time it becomes a solid cell mass, which is divided into the right and left lobes, connected to each other by he isthmus of the gland thyroid, which is located in front of the second and third ring developing tracheal (2).
The gland in general assumes its definitive shape and its final location in the neck towards the seventh week. In week 11, colloid material begins to appear inside the the follicles; Later it is possible to demonstrate the concentration of iodine and the synthesis of thyroid hormones(2).
During week 20, concentrations of fetal thyrostimulating hormones and thyroxine begin to increase, and towards week 35 they reach values corresponding to that of a adult.
Physiology:
The function of the gland is trigger the amount of hormone thyroid necessary for respond to the demand of peripheral tissues. For this it is necessary to capture iodide (carried to cape by he cotransporter thyroid sodium-iodine), his transfer to the colloid and its oxidation by thyroperoxidase (TPO).
Thyroglobulin, a precursor protein synthesized in the thyroid, is iodinated into residues specific tyrosine, forming monoiodotyrosine (MIT) and diiodotyrosine (DIT). The T.P.O. also catalyzes the coupling of two DIT molecules, or of one DIT and another MIT, which leads to the formation of T4 and triiodothyronine (T3), respectively, which are stored within the colloid forming part of the thyroglobulin molecule.
He hormone synthesis and release process by the thyroid, is stimulated by the TSH secreted by the thyrotropic cells of the pituitary gland. Thyroid cells express TSHR, a transmembrane receptor associated with G protein, which when it binds with TSH generates activation of intracellular pathways (through PLC and intracellular Ca) that stimulate the various TSH synthesis and secretion processes.
Various thyroid hormone transporters have been discovered in different tissues, which They serve to achieve the entry of hormones into the cells of these tissues.
Within hormonal metabolism, the main thing is the deiodination of T4 to form T3. The hormones thyroid they exercise his action by union to a receiver nuclear specific. The T3 HE binds to this receptor with an affinity 15 times higher than T4, which is why it is consider active thyroid hormone.
Pathophysiology:
Dysgenesis is the most common etiology; within it, ectopia (? of cases) occurs when "he tissue ectopic thyroid is located above the definitive normal location of the thyroid gland and is the result of a brake or abnormality in the caudal migration of the thyroid bud during embryonic development”(10). Thyroid remains are generally unique but in 5-10% it can be dual, sublingual and mid-cervical or multiple.
As result of this pathology HE gets a minor mass of cells follicular functioning, because of this, TSH-mediated compensatory growth is limited.
In shape less frequent, forming part of the dysgenesis HE finds the hypoplasia thyroid (<5% of cases) which is characterized by the presence of the gland in size diminished in correct location and variable function.
The dyshormonogenesis, causing defects in the biosynthesis of thyroid hormones, from of alterations in any of the steps of their preparation, is responsible for 15% total HC cases.
Regarding the central HC “the central structural or functional alterations, at any level of the axis hypothalamus-pituitary-thyroid, determine the qualitative or quantitative loss of stimulus trophic of the TSH about the gland thyroid and, in consequence, produce the Decreased synthesis and secretion of thyroid hormones.
Clinical manifestations. Diagnostic approach:
The symptomatology clinic is subtle and nonspecific in the first days of life mainly due to the transplacental supply of maternal thyroid hormones.
Among the first symptoms and signs that may appear infrequently when birth are found, inadequate suction, prolonged jaundice, hypothermia, edema, large fontanelle, hoarse crying, constipation, hypotonia, dry and rough skin, myxedema and failure of growth, HC is generally a silent disease, which is why it must be performed a biochemical test to detect it. Diagnosis in late stages can leave consequences severe and irreversible neurological disorders, especially mental retardation.
Due to what has been mentioned about the scarce specific symptoms and severity of this pathology, the which is reversible with treatment appropriate to time, HE they have formulated strategies of screening to achieve correct detection, with the aim of improving the quality of life of the patients.
He aim initial of the screening is the detection of all the shapes of hypothyroidism congenital primary: mild, moderate and serious, and the proof further sensitive for it is the measurement of the TSH. With bliss measurement No HE detect shapes secondary of the disease.
This type of screening has flaws, showing false negatives and false positives; according to Yunis, Ka et. to the. in the article “False-negative primary neonatal thyroid screening: the need for clinical surveillance and secondary screening” (2003) estimates between 5-10% false negative, these errors HE they can duty to the etiology of the pathology, either to situations biological conditions given by the increase in TSH after birth, etc. As well as errors in the collection of the sample (6).
Detection can be performed with 2 types of samples: cord blood serum and blood drops. cord blood on filter paper, both with different cut-off points as mentioned previously. TO leave of the extension of the investigation in he 2007, a sample obtained to the 40 hs of life in all the children through drops of blood of the bead, avoid cite needlessly for the repetition in serum, to those neonates whose values HE found between 25-50 Ul/ml for cord blood serum and between 15-25 Ul/ml for cord blood on filter paper (1).
An abnormal result in any of them must be followed by confirmation in serum by determining TSH and FT4. Figure 1 shows the algorithm taking into account count the different samples.
In premature children, it is necessary to evaluate thyroid function later, given that Pituitary immaturity does not allow an adequate TSH value, so HC can pass unnoticed. The guideline is to repeat it at 20 days of age (1). The situations specials in the that HE recommends measurement of TSH to the 2 and 4 weeks of life are the following: NB < 30 weeks GA, birth weight < 1500 g, use of antiseptics iodinated during childbirth or in the newborn, performing radiological techniques with iodinated contrast, neonates with syndrome of Down, insertion of catheters of silastic, births multiple particularly twins of the same sex, neonates admitted to intensive care (4).
Is important consider that neonatal screening is not a laboratory procedure only, but it is a multidisciplinary activity whose coordination with the system health care is essential to ensure its effectiveness and efficiency.
Figure 1. Algorithm taking into account the different samples
Extracted from Queiruga G, Lemes A, Ferolla C, Machado M, Queijo C, Garlo P, Parallada G. Neonatal screening: what a drop of blood can prevent. Angew Chemie Int Ed 6(11), 951–952. 1967
Studies complementary. Treatment:
Once HC is confirmed, no etiological study changes the therapeutic conduct, so it is not It is essential to do them at birth. If available, a scintigram can be performed thyroid in the first week after starting treatment with levothyroxine, before suppression of TSH. If this is not possible, treatment should be started urgently and carry out a reevaluation at 3 years of age. The etiological study should never delay the start of treatment (3).
This reevaluation is carried out to determine if it is a permanent primary HC or transient and the cause of it. Suspension of treatment for 4 weeks is necessary with the later measurement of TSH and T4L. Yeah HE confirm H.C. permanent (TSH by on of the range normal with T4L normal either low) they must be realized studies of image for determine its etiology (3).
The scintigraphy thyroid is he study of image with further specificity to define the location and size of thyroid tissue. Thyroid ultrasound, although it allows evaluating the size, location and characteristics of the thyroid gland, has technical limitations in newborns and a lower sensitivity for the detection of ectopias (3).
In case of H.C. central, HE has to carry out a hormonal evaluation of the rest of the axes pituitary glands and magnetic resonance imaging (MRI) with sellar approach for the detection of anomalies structural. Further of 80 % presents deficiency of others hormones, the further Frequently associated are growth hormone (GH) and hormone deficiency. adrenocorticotropic hormone (ACTH) (3).
The goal of treatment is to ensure adequate neurological and somatic development.
It should be started as soon as possible in the event of a positive result in the neonatal screening, after blood extraction for diagnostic confirmation, without waiting for its result.
It is performed with levothyroxine, in neonates with primary CH the dose is 10-15 µg/kg/day via oral, once a day and 30 minutes before breastfeeding, taking into account severity and etiology (3). It is necessary to quickly restore FT4 and TSH values to their normal range. He The first objective is the normalization of FT4 and then TSH.
HE they use dose further high for the agenesis (15 µg/kg/day), intermediate for the ectopias (12 µg/kg/day) and lower for dyshormonogenesis or other causes (10 µg/kg/day). In term neonates the dose is usually 37.5-50 µg/day (3). Subsequently the dose varies by function of growth and the age.
In the central HC the required dose is somewhat lower than those used in the primary HC. In shapes serious HE they use doses of up to 10 µg/kg/day and in mild forms 5-10 µg/kg/day (2). Treatment monitoring is carried out by determining FT4. Prior to At the beginning of treatment, adrenal insufficiency must be ruled out, and if present, treated, to avoid triggering an adrenal crisis.
Have in account that the absorption can be modified Yeah he child ingest iron, calcium, aluminum hydroxide, omeprazole, sucralfate, resins, fiber or soy (4).
Follow-up:
Regular monitoring of TSH and FT4 values is necessary to ensure that the dose of levothyroxine is adequate and the adherence to the treatment is good. Is It is also important to perform a complete physical examination, assess growth and development. psychomotor.
Blood collection is recommended before or at least 4 hours after administration of levothyroxine.
The first clinical and biochemical evaluation is carried out between the first or second week post initiation of treatment, and subsequently every 2 weeks until normalization of the TSH. Thereafter the frequency of checks may be reduced depending on the child's age.
After of a change of dose either of formulation of levothyroxine, a evaluation at 4-6 weeks.
The goal is to maintain TSH in the normal range and FT4 in the upper half of the normal range. normality in the primary HC, and in the central HC maintain FT4 in the upper half of the normal range (1).
Ideas to remember:
Early diagnosis and treatment is important to allow neurological development, adequate psychomotor and intellectual. The etiological search does not change the therapeutic conduct so it can be done later in the follow-up.
References
1. Queiruga G, Lemes A, Ferolla C, Machado M, Queijo C, Garlo P, Parallada G. Pesquisa neonatal: what a drop of blood can prevent. Angew Chemie Int Ed 6(11), 951–952. 1967
2. Van Trotsenburg P, Stoupa A, Léger J, Rohrer T, Peters C, Fugazzola L, et al. Congenital Hypothyroidism: A 2020-2021 Consensus Guidelines Update - An ENDO-European Reference Network Initiative Endorsed by the European Society for Pediatric Endocrinology and the European Society for Endocrinology. Thyroid. 2021;31(3):387–419.
3. Huidobro B, Rodriguez TO, Rodriguez M.D. Manual of diagnosis and therapy in Pediatric Endocrinology. Neonatal hypothyroidism. 2018;1–16.
4. Rodríguez Sánchez A, Chueca Guindulain MJ, Alija Merillas M, Ares Segura S, Moreno Navarrese J.C., Rodriguez Arnao M.D. Diagnosis and follow-up of patients with congenital hypothyroidism detected by neonatal screening. An Pediatrician 2019;90(4):250.e1-250.e8.
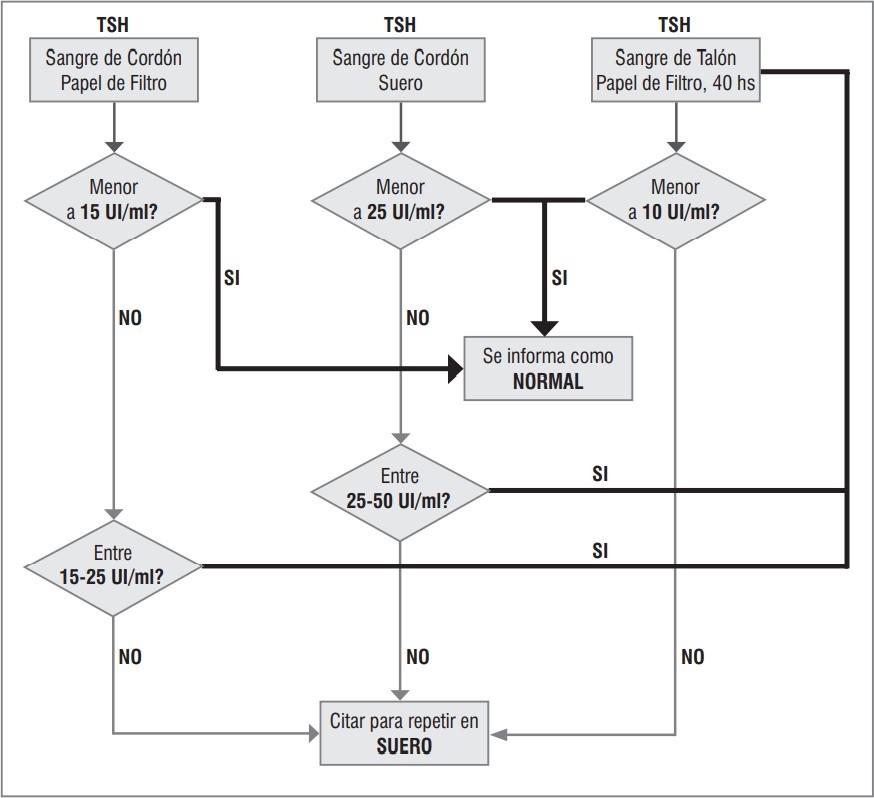
Figure 1
