Response to Steroids and Extended Surveillance in a Case with Cronkhite Canada Syndrome.
Response to Steroids and Extended Surveillance in a Case with Cronkhite Canada Syndrome.
Anil Grover *, Vinod Kumar Singhal 1, Faris Dawood Alaswad 2, Nufra Senopher 3, Adil Mohammed Suleman 4
1. Vinod Kumar Singhal, Consultant surgeon, Department of General Surgery, Prime hospital, Dubai, UAE.
2. Faris Dawood Alaswad, Consultant General Surgeon, Department of Surgery, Gladstone Hospital, Perth, Australia.
3. Nufra Senopher, Department of General Surgery, Prime Hospital, Dubai, UAE.
4. Adil Mohammed Suleman, Specialist General Surgeon, Department of General Surgery, Prime Hospital, Dubai, UAE.
*Correspondence to: Anil Grover, Specialist Internal Medicine, Prime Hospital, Dubai.
Copyright.
© 2024 Anil Grover. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 16 Sep 2024
Published: 17 Sep 2024
Abstract
We describe a 42-year-old woman who presented to us with diarrhea and edema last month. The features of protein deficient enteropathy (PLE), some ectodermal findings, and the presence of multiple gastroduodenal and ileocal polyps on endoscopy led us to investigate a rare gastrointestinal (GI) polyp syndrome called Clonket Canada syndrome (CCS). Histopathology of the gastrointestinal polyps further confirmed the diagnosis. She responded excellently to steroids and has been treated with azathioprine for the past 36 months without recurrence. To our knowledge, CCS is the only colonic polyposis that responds to steroids.
Response to Steroids and Extended Surveillance in a Case with Cronkhite Canada Syndrome.
Introduction
Clonket-Canada Syndrome (CCS) is a rare intestinal polyposis syndrome that can affect any part of the intestine except the esophagus. This site was first reported in 1955 by Leonard W. Cronkhite and Wilma J Canada in two female patients with colon disease, cutaneous hyperpigmentation, alopecia, and onychodystrophy [1]. Since then, numerous cases have been reported in the literature. The disease is highly prevalent and responds to steroids and immunosuppressants. We present a case of CCS that responded to steroids and azathioprine.
Case Report
A 42-year-old woman has had abdominal pain, vomiting, and loose stools (10 to 12 times per day) for the past 6 months. She has also noticed hair loss, bad breath, changes in her nails, and dark skin all over her body. She has also had bloating, extreme fatigue, and loss of appetite for a month. She reports no bloody stools, fever, arthritis, weakness, or mouth sores. She has no family history of similar illnesses. On examination, he was unconscious but agitated. He has a low body weight (19.6 Kg/m2), pale, dark skin all over the body, frontal alopecia, diffuse skin pigmentation and dystrophic finger and toenails (Figure 1). Blood test showed red blood, hemoglobin 9.5g/dL (12 - 14 gm/dL; - 4.5 gm/dL), persistent hypokalemia, serum concentration 2.8-3.2 meq/dL). Small amount of pleural effusion and mild ascites. Disease markers including ESR and CRP are within normal limits. HIV serology and ANA were negative. Stool tests and immunoglobulin profile were within normal limits. Esophagogastroduodenoscopy (EGD) revealed multiple small masses throughout the stomach (Figure 2A) and duodenum (Figure 2B). Mucosal sections were obtained from the stomach and duodenal polyps. Ileocolonoscopy also revealed multiple intestinal polyps of varying sizes (Figure 2C) and a large polyp (approximately 1.5 cm) in the terminal ileum. Segmental biopsies were performed from polyps and normal mucosa. Colonic polyp section results revealed hamartomatous polyps and tubular adenomas with mild dysplasia (Figure 3A). Mucosal findings were remarkable, with marked edema, mild lymphoplasmacytic infiltration, and cystically dilated tumor with concentrated mucin. (Figure 3B) Gastric and duodenal biopsies also showed hamartomatous polyps, and immunohistochemistry showed a few plasma cells positive for IgG4. It is classified as gastrointestinal polyposis. The combination of the polyposis, ectodermal features, and histopathologic findings led to a definitive diagnosis of Clonket-Canada syndrome. We gave her oral prednisolone 40 mg/day for 1 month, then tapered by 5 mg every 2 weeks to reach a final treatment dose of 5 mg/day for 1 month. She has a severe reaction to steroids. Azathioprine was used with a steroid dose of 50 mg/day for 3 months and continued thereafter. After 3 months of treatment, stool frequency and consistency improved. Generalized edema decreased, appetite increased, and hyperpigmentation decreased. The patient is currently taking azathioprine 50 mg. There has been no recurrence in the last 36 months.
Figure 1: Onychodystrophy of finger nails.
Figure 2: Endoscopic images: Gastric body numerous polyps (2A), Duodenal / D2 polyps (2B), Colonic polyps (2C).
Figure 3: Colonic histopathology: Features of the hamartomatous polyp and tubular adenoma with mild dysplasia (3A), Intervening mucosal biopsy showing marked edema, mild lymphoplasmacytic infiltrates, and cystically dilated glands with inspissated mucin (3B). [Hematoxylin and Eosin stain]
Discussion
CCS is a nonmalignant intestinal polyposis characterized by hamartomatous polyposis, alopecia, onychodystrophy, hyperpigmentation, and diarrhea (1). All these features were present in our patients. It is associated with severe pain and is often caused by PLE. Delay in diagnosis is common, mainly due to physician unawareness of this rare condition, which leads to poor outcomes. Its pathogenesis remains unclear. However, the presence of IgG4 staining in polyps often predicts an autoimmune history, and this is confirmed by their clinical and endoscopic response to steroids and other anti-inflammatory drugs [2]. These polyps are usually benign hamartomatous polyps, but there is also a risk of adenomatous dysplasia. Diagnosis is based on clinical, endoscopic, and histopathological findings (3). The difference between the two is the histology of the affected mucosa, which shows edema, congestion, and inflammation of the lamina propria in CCS (as seen in our case), but is normal in pediatric polyps [4]. Various treatments have been tried in CCS patients with varying degrees of success. These treatments include corticosteroids, H2-receptor antagonists, cromolyn sodium, overfeeding, and surgery [5]. Corticosteroids are considered the mainstay of treatment. The official treatment is prednisone 40 mg per week, tapered by 5 mg per week until the patient is tapered. In one study, 10 of 11 patients treated with this technique showed improvement in symptoms within three months [3]. However, recurrence of symptoms is common, so patients are often treated with maintenance immunomodulators such as azathioprine [2,6]. Three patients responded to steroids and had no relapses on azathioprine.
Although there is no general consensus for colonoscopy with CCS, polyps > 10 mm in size should be removed because of the high risk of dysplasia and malignancy [7]. In this case, our goal is to perform annual EGD and colonoscopy to detect malignant growth and/or mucosal remission of adenomatous polyps in terms of size reduction or gastrointestinal polyp count.
References
1. Cronkhite LW Jr, Canada WJ. Generalized gastrointestinal poyposis; an unusual syndrome of polyposis, pigmentation, alopecia, and onychotrophia. N Engl J Med. 1955; 252(24):1011-1015. 10.1056/NEJM195506162522401
2. Sweetser S, Ahlquist DA, Osborn NK, et al. Clinicopathologic features and treatment outcomes in Cronkhite-Canada syndrome: support for autoimmunity. Dig Dis Sci. 2011 Sep 1. 10.1007/s10620-011-1874-9
3. Seshadri D, Karagiorgos N, Hyser MJ. A case of Cronkhite-Canada syndrome and a review of gastrointestinal polyposis syndromes. Gastroenterol Hepatol (NY) 2012;8:197–201.
4. Burke AP, Sobin LH. The pathology of Cronkhite-Canada polyps. A comparison to juvenile polyposis. Am J Surg Pathol. 1989;13:940–946. 10.1097/00000478-198911000-00004
5. Ward EM, Wolfsen HC. Pharmacological management of Cronkhite-Canada syndrome. Expert Opin Pharmacother. 2003;4:385–389. 10.1517/14656566.4.3.385
6. Mao EJ, Hyder SM, DeNucci TD, Fine S. A Successful Steroid-Sparing Approach in Cronkhite-Canada Syndrome. ACG Case Reports J. 2019;6(3):e00055. 10.14309/crj.0000000000000055
7. Sweetser S, Alexander GL, Boardman LA. A case of Cronkhite-Canada syndrome presenting with adenomatous and inflammatory colon polyps. Nat Rev Gastroenterol Hepatol. 2010;7:460–464. 10.1038/nrgastro.2010.112

Figure 1
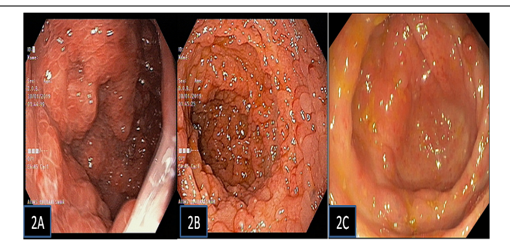
Figure 2
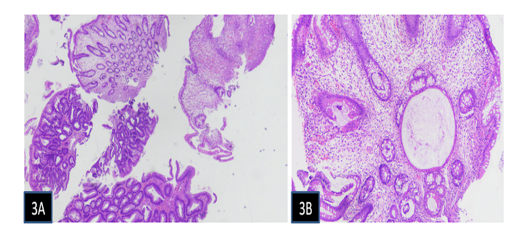
Figure 3
