Prevention of Biliary Stent Obstruction: Findings from a Randomized Controlled Trial
Prevention of Biliary Stent Obstruction: Findings from a Randomized Controlled Trial
Vinod Kumar Singhal 1*, Adil Mohammed Suleman 2, Nufra Senopher 3, Faris Dawood Alaswad4, Riya Singhal5
1. Vinod Kumar Singhal, Consultant surgeon, Department of General Surgery, Prime hospital, Dubai, UAE.
2. Adil Mohammed Suleman, Specialist General Surgeon, Department of General Surgery, Prime Hospital, Dubai, UAE.
3. Nufra Senopher, Department of General Surgery, Prime Hospital, Dubai, UAE.
4. Faris Dawood Alaswad, Consultant General Surgeon, Department of Surgery, Gladstone Hospital, Perth, Australia.
5. Riya Singhal, Student, SMCH, Dubai, UAE.
*Correspondence to: Vinod Kumar Singhal, Consultant surgeon, Department of General Surgery, Prime hospital, Dubai, UAE.
Copyright.
© 2024 Vinod Kumar Singhal. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 18 Sep 2024
Published: 21 Sep 2024
Prevention of Biliary Stent Obstruction: Findings from a Randomized Controlled Trial
Educational objectives
- Know the reasons for obstruction of plastic biliary prostheses
- Know the factors acting on the permeability of plastic prostheses
- Propose a therapeutic approach to increase the permeability of digestive prostheses
Keywords: Plastic biliary prosthesis, biliary stenoses
Abbreviations
ICM: ipp, cefalexin, metronidazole
IE= Occurring Events
IN = Events Not Occurring
CE = Events Occurring Control Group
CN = Events Not Occurring in the Control Group
Introduction
The frequency of cholangiocarcinoma is 2 per 100,000 people, most often the diagnosis is made at the stage of cholestatic jaundice or cholangitis, treatment is focused on surgery and chemotherapy and targeted therapies, endoscopic treatment with prosthesis Plastic or metallic bile is essential to relieve jaundice or cholangitis in order to prepare the patient for invasive therapies.
However, the use of plastic and even metal prostheses is burdened with a significant rate of early or late obstruction with a lower rate for metal prostheses.
Under our skies the problem of availability and non-reimbursement of metal prostheses forces us to use plastic prostheses.
Obstruction of biliary prostheses is responsible for the recurrence of jaundice or the appearance of cholangitis depriving the patient of chemotherapy.
Why this test and its pathophysiological bases
We have noted over the years an inter-individual variability in terms of biliary obstruction in patients with some whose prosthesis is obstructed in the month following its installation and others who keep their prostheses permeable for several months suggesting a exogenous factor independent of the type of prosthesis.
just as the obstruction or the appearance of lithiasis in metal biliary prostheses in the months following the installation of these prostheses in patients who have never had biliary lithiasis makes us think of a local interaction with the bile salts.
The other element which supports these hypotheses is the macroscopic analysis of the obstructed prostheses after their removal shows a rather distal obstruction of the prosthesis on its free edge in the duodenal lumen, and especially the very low rate of obstruction of the prostheses. plastics that migrate into the bile ducts.
Hypothesis mentioned
Acid reflux into the bile ducts.
Chemical interaction between acidic gastric juice and bile in the bile ducts which creates a precipitate which obstructs the prostheses or allows the appearance of lithiasis in the biliary prostheses.
Pathophysiological bases
Bile acids are produced in the liver by the oxidation of cholesterol.
Bile acids also serve the purpose of breaking down fats.
They become bile salts following the drop in pH.
The bile salts formed under the action of acid reflux in the bile ducts induce precipitates which obstruct the prostheses “theory”
Retrograde acid reflux
Hypothesis to be demonstrated: retrograde acid reflux in the bile ducts
The sphincter of ODDI: is a sphincter which regulates bile flow by inducing hyperpressure in the bile ducts and thereby prevents the reflux of duodenal fluid into the bile ducts.
The cancellation of this pressure guard under the effect of sphincterotomy and the prosthesis induces acid reflux in the bile ducts.
This explains the appearance of cholelithiasis after sphincterotomy as well as the obstruction of plastic and metal prostheses.
Suppression of this acid bile reflux by proton pump inhibitors was chosen as the basis for this trial.
Choice of test type
RANDOMIZED CONTROL TEST
Because it is a therapeutic intervention that is tested
Allows you to test the validity of a specific hypothesis
Objective
To evaluate the effectiveness of PPI treatment with double antibiotic therapy on the lifespan without obstruction of a plastic biliary prosthesis after its installation by ERCP.
Study
Monocentric, single-blind randomized
Inclusion and exclusion criteria defined.
Strict monitoring criteria
Criteria for stopping tracking
Inclusion criteria
OBSTRUCTION OF BILIARY TUMORS OF NEOPLASTIC ORIGIN
PANCREAS CANCER
BILIARY TRACT TUMORS
EXTRINSIC COMPRESSION OF THE VBP BY METASTATIC ADPs
“Post-operative” BENIGN STENOSES 03 liver transplant patient
Exclusion criteria
Non-compliance with treatment
Side effects leading to treatment interruption
Loss of vision of the patient
Absence of initial cholestasis
Tracking Discontinuation Criteria
• Operated patient
• Death
• Obstruction of the prosthesis and its replacement
Objective of the protocol
1- EXTEND THE LIFE OF THE PROSTHESIS
Absence of jaundice per protocol.
Patient arrives at surgery without resorting to prosthesis replacement
No interruption of chemotherapy
2- DECREASE THE FREQUENCY OF EXPECTED POST DRAINAGE EVENTS
Occurrence of expected events after placement of the prosthesis
The occurrence of an expected accident is an emergency replacement of the prosthesis because it is fatal
Expected events after placement of the prosthesis
1. Reappearance of jaundice
2. Early cholangitis: sign of contamination per procedure
3. Late cholangitis: sign of obstruction
4. Elevation of bilirubin: indicator of obstruction
5. Migration of the prosthesis: caused by obstruction and hyperpressure upstream
6. Appearance of liver metastases “monitoring stopped”
TEST PHASE
Trial start date 03/2023 followed until April 2024
Number of patients included 131
Age ranges from 33 years to 97 years
SIMPLE BLIND RANDOMIZATION
Patients without PPI vs. patients included in the ICM protocol
All patients were drained by plastic biliary prosthesis, 47 patients were placed under the ICM arm, 49 patients without ICM, 25 patients were lost to follow-up, 10 patients were excluded due to poor compliance with treatment.
In the control group there were 33 men and 16 women with an age varying from 33 to 97 years vs. 26 men and 21 women in the ICM group with an average age of 34 to 95 years, the strict follow-up criteria were the appearance of symptoms of cholangitis, with collection of monthly bilirubin levels and follow-up until obstruction or death
Table 1: Age ranges from 34 years to 95 years Average Age 64 years
The indications were mainly pancreatic cancer and bile ducts with 28 pancreatic cancers in the ICM group and 30 bile duct cancers.
Table 2: duration of follow-up for each patient
30 patients died during follow-up
Life expectancy after placement of the prosthesis is 1 day to 142 days without obstruction of the prosthesis
Average survival is 85 days
Functional prosthesis until the day of death in 80% of patients.
15 Patients Still Alive Without Obstruction of the Prosthesis at the end of the study with a Follow-up of 106 Days to 349 Days
Average 199.86 Days
Table 3; on the left followed by the bilirubin level in the ICM group, on the right the control group
The results of follow-up of the patients at one month, in the control group, 06 patients out of 40 presented an obstruction of the prosthesis, i.e. 15% of patients vs. 03 patients out of 32 in the ICM group, i.e. 9.3%, at the second month eight additional patients in the control group had obstruction of the prosthesis, i.e. a total of 35% of patients vs. 02 additional patients in the ICM group, i.e. 15.6% of patients, at the third month 12 additional patients presented obstruction of the prosthesis, i.e. a total of 65% of patients vs. an additional patient in the ICM group, i.e. a total of 15.6% of patients, after 05 months all patients in the control group had prosthesis dysfunction vs. the rate remained unchanged in the ICM group.
The main manifestations of prosthesis obstructions at one month in the control group were as follows, 2.1% early cholangitis (less than a week after placement of the prosthesis) 13% late cholangitis, 6 .52% migration and 13% jaundice vs. 2.12% early cholangitis, 6.32% late cholangitis, no migration and 6.32% migration in the ICM group, at the second month of follow-up the control group presented 28.56% of late cholangitis vs. 10.6% in the ICM group, 8.1% of migration in the control group vs. 2.2% in the ICM group, 28% of jaundice in the control group vs 10.6% in the ICM group, the disparity widens in the third month with 65% late cholangitis vs 12.7% in the ICM group, 16% migration in the control group vs 2% in the ICM group ICM, and 65% jaundice in the control group vs. 12.7% in the ICM group.
The statistical analysis of this study shows the following
Calculation of relative risk according to this formula
RR= (IE/ (IE+IN))/ (CE/ (CE+CN))
RELATIVE RISK OF OBSTRUCTION OF THE PROSTHESIS AT M1 is 0.52
This means that the result is reduced by exposure which constitutes a protective factor.
The risk relative to M2 is 0.37 which constitutes a protection factor
The risk relative to M3 is calculated at 0.23 which constitutes a protection factor.
In conclusion
The absence of prosthesis obstruction allows the patient to benefit from chemotherapy and possibly extend lifespan without incident requiring its interruption.
This original work demonstrates the protective effect of PPIs on the maintenance of function of plastic biliary prostheses, this trial opens the way to other larger-scale multicenter studies possibly paving the way for a recommendation.
References
1. van Berkel AM, van Marle J, van Veen H, Groen AK, Huibregtse K. A scanning electron microscopic study of biliary stent materials. Gastrointest Endosc 2000;51:19-22.
2.Maillot M, Aucher P, Robert S, Richer JP, Bon D, Moesch C, et al. Polyethylene stent blockage: a porcine model. Gastrointest Endosc 2000;51:12-8.
3.Libby ED, Leung JW. Prevention of biliary stent clogging: a clinical review. Am J Gastroenterol 1996;91:1301-8.
4.Speer AG, Cotton PB, MacRae KD. Endoscopic management of malignant biliary obstruction: stents of 10 French gauge are preferrable to stents of 8 French gauge. Gastrointest Endosc 1988;34:412-7.
5.Gilbert DA, DiMarino AJ, Jensen DM, Katon R, Kimmey MB, Laine L, et al. Status evaluation: biliary stents. Gastrointest Endosc 1992;38:750-2.
6.Dowidar N, Kolmos HJ, Matzen P. Experimental clogging of biliary endoprostheses: role of bacteria, endoprosthesis material and design. Scand J Gastroenterol 1992;27:77-80.
7.Jansen B, Goodman LP, Ruiten D. Bacterial adherence to hydrophilic polymer-coated polyurethane stents. Gastrointest Endosc 1993;39:670-3.
8.Sung JJ, Chung SC, Tsui C, Co AL, Li AK. Omitting side-holes in biliary stents does not improve drainage of the obstructed biliary system: a prospective randomized trial. Gastrointest Endosc 1994;40:321-5.
9.van Berkel AM, Boland C, Redekop WK, Bergman JJ, Groen AK, Tytgat GNJ, Huibregtse K. A prospective randomized trial of teflon versus polyethylene stents for distal malignant biliary obstruction. Endoscopy 1998;30:681-6.
10.Terruzzi V, Comin U, De Grazia F, Toti GL, Zambelli A, Beretta S, Minoli G. Propsective randomized trial comparing “Tannenbaum” teflon and traditional polyethylene stents in distal malignant biliary stenosis. Gastrointest Endosc 2000;51:23-7.
11.Georghegan JG, Branch MS, Costerton JW, Pappas TN, Cotton PB. Placement of biliary stents above the sphincter of Oddi prolongs stent patency in dogs [abstract]. Gut 1991;32: A1232.
12.Pedersen FM, Lassen AT, Schaffalitzky de Muckadell OB. Randomized trial of stent placed above and across the sphincter of Oddi in malignant bile duct obstruction. Gastrointest Endosc 1998;48:574-9.
13.Barrioz T, Ingrand P, Besson I, de Ledinghen V, Silvain C, Beauchant M. Randomised trial of prevention of biliary stent occlusion by ursodeoxycholic acid plus norfloxacin. Lancet 1994;344:581-2.
14.Ghosh S, Palmer KR. Prevention of biliary stent occlusion using cyclical antibiotics and ursodeoxycholic acid. Gut 1994;35:1757-9.
15.Luman W, Ghosh S, Palmer KR. A combination of ciprofloxacin and rowachol does not prevent biliary stent occlusion. Gastrointest Endosc 1999;49:316-21.
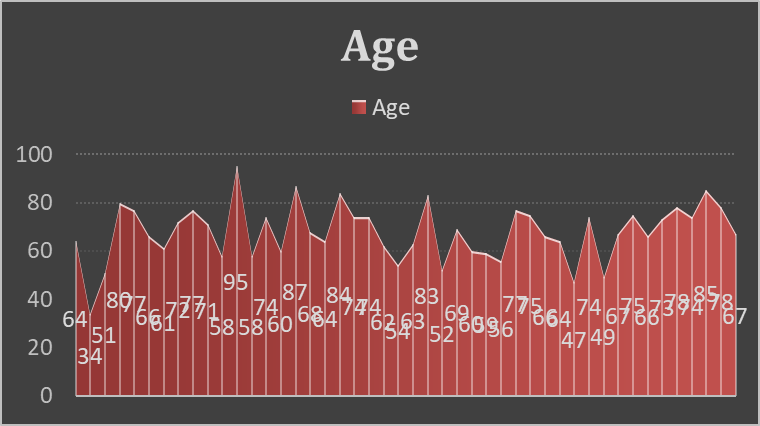
Figure 1
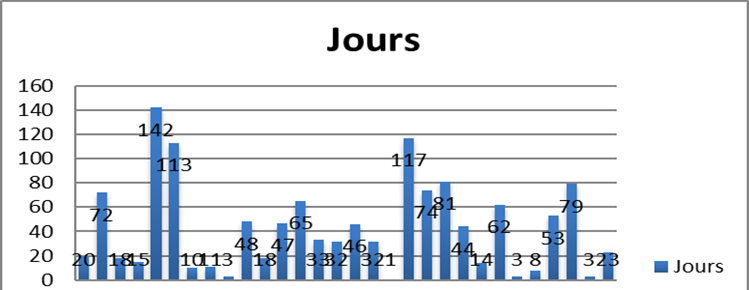
Figure 2
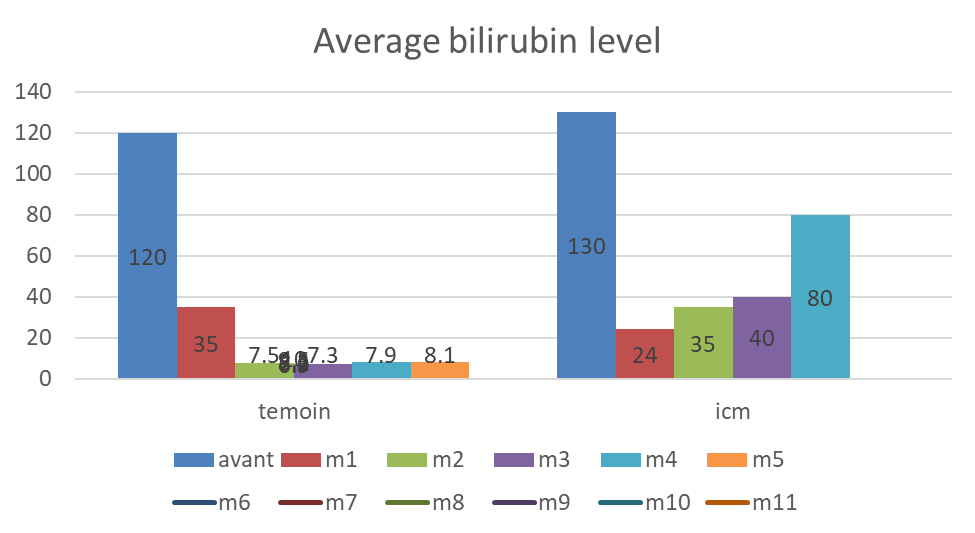
Figure 3
