A Short-Term Prospective Clinical Study on Sigmoid Volvulus
A Short-Term Prospective Clinical Study on Sigmoid Volvulus
Vinod Kumar Singhal 1*, Adil Mohammed Suleman 2, Nufra Senopher 3, Faris Dawood Alaswad4, Riya Singhal5
1. Vinod Kumar Singhal, Consultant surgeon, Department of General Surgery, Prime hospital, Dubai, UAE.
2. Adil Mohammed Suleman, Specialist General Surgeon, Department of General Surgery, Prime Hospital, Dubai, UAE.
3. Nufra Senopher, Department of General Surgery, Prime Hospital, Dubai, UAE.
4. Faris Dawood Alaswad, Consultant General Surgeon, Department of Surgery, Gladstone Hospital, Perth, Australia.
5. Riya Singhal, Student, SMCH, Dubai, UAE.
*Correspondence to: Vinod Kumar Singhal, Consultant surgeon, Department of General Surgery, Prime hospital, Dubai, UAE.
Copyright.
© 2024 Vinod Kumar Singhal. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 18 Sep 2024
Published: 21 Sep 2024
Abstract
The study aimed to investigate the presentation, investigative modalities, clinical management, and intervention outcomes of sigmoid volvulus in 20 cases over two years. Results showed that sigmoid volvulus is common in the 40-60 age group, with a slight male predominance. The best procedure for gangrenous volvulus is Hartmann's procedure followed by elective colostomy closure. For non-gangrenous volvulus, resection and primary anastomosis are the best options. Sigmoidopexy has a high incidence of early and late recurrence, wound infection, burst abdomen, and stoma retraction. Mortality related to the disease process is high after primary resection and EEA in the gangrenous group. The study concluded that resection with Hartmann's is the safest procedure when bowel conditions prevent primary anastomosis.
KEYWORDS: Hartmann’s Procedure, Sigmoid Volvulus, Mortality, EEA
A Short-Term Prospective Clinical Study on Sigmoid Volvulus
Introduction
Volvulus is abnormal twisting or rotation of a portion of the bowel around its mesenteric axis. The twist causes lumen occlusion with resultant obstruction and vascular compromise. ( 1 )
The earliest description of volvulus dates back to 1500 BC where it finds mention in the Ebers Papyrus. Various forms of colonic volvulus were described by Von Rakitansky in mid-nineteenth century. Sigmoid colon, Caecum or right colon, transverse colon and splenic flexure are involved in descending order of frequency. Colonic volvulus occurs in the setting of a dilated redundant colonic segment with a narrow mesenteric base which serves as a fulcrum for the development of volvulus. ( 2,3 ) The pre-dispoisng factors may be acquired as in sigmoid volvulus or congenital in origin like in cases of caecal volvulus. Left untreated, volvulus progresses from colonic obstruction to strangulation, gangrene and perforation with fecal peritonitis.
Sigmoid volvulus is a surgical emergency. The disease is frequently reported in the volvulus belt which includes countries in the Middle East, Africa, the Indian subcontinent, Turkey and South America where it accounts for almost half of all cases of large bowel obstructions. ( 4 )
It is the third leading cause of large bowel obstruction in North America and is frequently recognized as a cause of acute abdomen in the elderly and institutionalized patients in the USA and UK. Some Indian states like Bihar, Madhya Pradesh, Uttar Pradesh and some parts of Maharashtra have reported a higher incidence of Sigmoid Volvulus cases.
Materials and Methods
This Multi centre study was undertaken in the Department of General Surgery, in various hospitals over a period of two years. It enrolled 164 cases of acute intestinal obstruction, which comprised of 20 cases of sigmoid volvulus (12.9%).
Maximum number of patients belong to age of 41 to 60 years of age. Majority of the patients were males (11/20).
All the patients who were admitted with clinical features of acute intestinal obstruction were subjected to emergency surgery after resuscitation.
In all the patients, apart from routine blood workup, serum albumin and CECT ABDOMEN AND PELVIS was taken.
Various modalities of surgeries performed depending upon the viability of bowel (gangrenous or non gangrenous), albumin status, bowel edema and duration of presentation.
In all the ases, intra-abdominal findings during surgery including any predisposing factors were noted. Subsequently to the procedure, they were placed in post-operative ward. All post-operative complications were noted and dealt appropriately. Mean followup upto 12 months noted and outcome assessed interms of recurrence of symptoms.
As most of the patients didn't come for follow up, only immediate outcome of the management were studied. One patient came with recurrence after sigmoidopexy were subjected to sigmoid resection.
Results
Out of 164 cases of intestinal obstruction, 20 cases of Sigmoid volvulus were noted (12.19%).
Peak incidence was within the age group of 41-60 years with males comprised majority of cases (11/20).
Pain abdomen, absolute constipation and abdominal distention were the main presenting complaints and were present in all the patients of Sigmoid Volvulus. History suggestive of recurrent episodes of intestinal obstruction was present in about 15 % of the cases.
Majority of the cases presented between third and fourth day of the onset of symptoms. However, no correlation was found between duration of onset of symptoms and the presence of gangrenous bowel.
All patients were subject to routine biochemical evaluation. Increased leukocyte count and hypokalemia were the only two persistent findings.
Abdominal X rays could diagnose only 40% (8 cases) of cases with sigmoid volvulus with features of inner bent tube appearance and omega appearance. Rest of cases showed dilated large bowel with air fluid levels. No other cross sectional imaging was done.
In 30% of cases, conservative management was attempted with insertion of flatus tube. The results of conservative measures were not very successful in present series. Sinha et al reported a success rate of 13.7 % with decompression by non-operative methods (sigmoidoscopic decompression) (5). Similarly Anderson and Lee et al shows a success rate 85% (6). The failure of conservative measures in present series can be explained by non-availability of emergency sigmoidoscopy. Ultimately all patients underwent laparotomy. In the present series no cases underwent full conservative management. The incidence of recurrence has been cited differently in literature and varies between 25 to 43 % (7,8).
PREDISPOSING FACTORS
1. Long pelvic mesocolon was observed in 80% of cases.
2. Elongated dilated, redundant sigmoid colon was seen in all elderly patients indicating there is elongation and distension of sigmoid colon with advancing age.
3. Enlarged lymph nodes with fibrosis of mesosigmoid found in two case indicating colonic infection in 10% of cases predisposing to sigmoid volvulus
4. Chronic constipation was seen in one case.
Anatomical factors are the main predisposing factors found in the study.
MANAGEMENT
All cases presented with acute intestinal obstruction were subjected to immediate lapartomy. Only 30% of cases were attempted conservative management.
Preoperatively:
a) Of which only 6 were attempted conservative management with flatus tube (sigmoidoscopy not available in emergency).
b) Conservative measures were not successful in present series. The R.S.Sinha series, in which decompression by Non-operative methods (sigmoidoscopic decompression) was successful in 13.74%, whereas in J.R. Anderson and D.Lee series shows a success rate 85%. The failure of conservative measures in present series can be explained by Non availability of emergency sigmoidoscopy. Finally all the cases were subjected to lapartomy.
c) No cases were attempted for conservative management due to high recurrence rate. 43% from Lau et al study and Atamanalap study reports 25.8% recurrence.
Table 2- Types of procedures performed
|
Procedure |
Number of patients |
% of patients |
Cured (%) |
Expired (%) |
|
Derotation and sigmoidopexy |
5 |
25 |
100 |
0 |
|
Resection and EEA |
12 |
60 |
66.6 |
33.4 |
|
Hartmann’s procedure |
3 |
15 |
100 |
0 |
OPERATIONS PERFORMED IN GANGRENOUS SIGMOID COLONIC VOLVULUS
1. Resection of gangrenous sigmoid colon with Hartmann's procedure in 15% (3cases) of cases.
2. Resection of gangrenous sigmoid colon with EEA in 10% (2 cases) of cases.
OPERATION PERFORMED FOR VIABLE SIGMOID COLONIC VOLVULUS
1. Resection with EEA in 50% (10 cases) of cases.
2. Derotation and Sigmoidopexy in 25% (5 cases) of cases.
Fig 1. Management of non-gangrenous sigmoid volvulus
COMPLICATIONS - POST OPERATION MORBIDITY AND MORTALITY
Mortality: Of the 20 Patients 4 deaths (20%) were observed.
1. Two in gangrenous group i.e., two out of 5 —> 40%. mortality due to sepsis
2. Two in viable group i.e., two out of 15 —» 13.5% mortality, mortality is not due to anastomotic leak.
Recurrent obstruction developed in 1 case out of 5 cases which was subjected to Resection and end to end anastomosis.
Stoma retraction was observed in two cases of Hartmann’s procedure.
Wound infection with burst abdomen was observed in three cases .Two cases in patients who undergone Hartmann’s procedure
No focal fistula observed in any case.
Discussion
20 cases of sigmoid volvulus that have presented to emergency department during the period from October 2010 to September 2012 were studied.
INCIDENCE
Of the 164 cases of Intestinal obstruction(small and large intestine) , incidence of Sigmoid volvulus is 12.19% (20 cases).
Griffin w et al 6 series states that incidence of sigmoid volvulus is 2.2% of intestinal obstruction as a whole. Present study, it is 12.19%. Eventhough higher than Griffin study, incidence of sigmoid volvulus is less in our part of state when compared to other parts of country.
SEX INCIDENCE
In the present series out of 20 cases, male to female ratio is 1.2:1 which are in agree with results shown by R.S.Sinha8 i.e., male preponderance with male to female ration of 3.5:1 was reported.
Table 3. Sex Incidence
|
Authors |
M:F Ratio |
|
Khanna AK et al 7 |
2.5:1 |
|
R S Sinha8 |
3.5:1 |
|
Present study |
1.2:1 |
AGE INCIDENCE
In the study majority of patients were in 5th& 6th decades. Which are in agreement with the figures put forward Khanna AK et al 7 and in contrary to the Western series J.R. Anderson &D.Lee Series. 9
Table 4- Age incidence by various authors
|
AUTHORS |
MEAN AGE IN YEARS |
|
Khanna AK et al 7 |
55.5 |
|
Deu 10 |
45.6 |
|
Present study |
47.6 |
SOCIO-ECONOMIC STATUS
All patients were from low socio-economic status, in agreement with R S Sinha series. 8
CLINICAL FEATURES
All the patients presented with Pain abdomen, Constipation and Abdominal distention. Only 50% (10 cases) of patients presented with Vomiting,
Table 5. Clinical Features
|
Clinical Features |
Percentage (No. of cases) |
S.R.Anderson 9 |
|
Pain abdomen |
100% |
73.9% |
|
Constipation |
100% |
47.8% |
|
Abdominal distension |
100% |
65.7% |
|
Vomiting |
50% |
65.7% |
TIME OF PRESENTATION
There was no relation between the onset of symptoms to the appearance of gangrene. In fact, cases which presented within 24 hrs, have progressed to gangrene. Anderson JR 9 study states that duration of symptoms averages 5-7 days, of 14 patients.
Table -6 Time of Presentation
|
Time of Presentation |
Cases |
Percentage of cases presented with Gangrene |
Cases presented with gangrene |
|
<24 hours |
3 |
66.6 % |
2 cases |
|
25-48 hours |
3 |
- |
- |
|
49-72 hours |
9 |
33.3% |
3 cases |
|
73-96 hours |
5 |
- |
- |
OPERATIVE FINDINGS
1. In 20 cases, volvulus occurred in anti-clockwise direction
2. In 80% of cases there was a long mesosigmoid with elongated dilated sigmoid colon.
3. In 10% of cases enlarged lymph nodes with fibrosis of mesosigmoid was found.
4. In all the cases of gangrenous sigmoid colon, there was more than 2 turns of anti-clockwise rotation.
5. In one case, which give H/o previous surgery, there was a post-operative adhesive band which attached to anti-mesenteric border of sigmoid to anterior abdominal wall.
MANAGEMENT
As it differs depending upon whether sigmoid colon is Gangrenous or Non- gangrenous, it is discussed separately for both.
MANAGEMENT OF GANGRENOUS SIGMOID VOLVULUS
In the study group 5 out of 20 cases were gangrenous. Following table shows the different surgeries done and their complications.
Table 7. Management of gangrenous sigmoid volvulus
|
No. of cases |
Surgery |
Complications |
|
3 |
Hartmann’s procedure |
Wound infection with burst abdomen. Retraction of end Colostomy |
|
2. |
Resection with primary End-to-End anastomosis |
Both cases developed anastomotic Both cases died of septicaemic shock. |
Postoperative complication after Hartmann’s procedure is more related to stoma and wound. But no mortality observed.
Table 8. Hartmann’s procedures
|
Authors |
Number of patients |
% of patients |
Cured (%) |
Expired (%) |
|
Diaz plasencia et al 11 |
35 |
28.7 |
60.6 |
37.4 |
|
People JB et al 12 |
15 |
26.6 |
87 |
13 |
|
Present study |
3 |
15 |
100 |
0 |
Diaz plasencia et al11 subjected 28.7% of patients for this treatment and found 68.6% cure rate and 37.4% mortality. People’s J.B et al12 study 26.6% of patients were subjected to Hartmann’s procedure 87% cure rate and 13% mortality. In present study 15% of patients were subjected to Hartmann’s procedure, cure rate 100% and no morality.
Table 9. MANAGEMENT OF NON-GANGRENOUS SIGMOID VOLVULUS
|
No. of cases |
Surgery |
Complications |
|
5 |
Sigmoidopexy |
One case had recurrence followed by Resection and EEA |
|
10 |
Resection and EEA |
Death occurred in 2 cases. One died of Acute Myocardial Infarction and other of pulmonary embolism. Rest of cases immediate post-operative period was uneventful. |
Table 10. Derotation and Sigmoidopexy
|
Authors |
No of Patients (%) |
Cured (%) |
Expired (%) |
|
Diaz plasencia et al11 |
15.4 |
100 |
0 |
|
Present study |
25 |
100 |
0 |
Diaz plasenciaet al11 subjected 15.4% of patient for this treatment and found 100% cure rate. In our present study 20% patients underwent Derotation and fixation to abdominal wall procedure with 100% cure rate.
Table - 11 Primary sigmoid resection and end to end anastomosis
|
Authors |
No of Patients |
% of Patients |
Cured (%) |
Expired(%) |
|
Larkin JO et aj13 |
27 |
55.5 |
100 |
0 |
|
People JB et al12 |
19 |
47.5 |
73.7 |
26.3 |
|
Diaz plasencia et al11 |
69 |
56.9 |
87 |
13 |
|
Present study |
12 |
60 |
66.6 |
33.4 |
Diaz plasencia et al11 subjected 56.9% of patients for this treatment and found 87% cure rate and 13% mortality. People’s J.B. et al12 study 47.6% of patients were subjected to primary resection and end to end anastomosis however73.7% of patients were cured and 26.3% mortality. In our present study 60% of patients underwent Primary resection and end to end anastomosis with cure rate 66.6% and mortality 33.4% in which 100% mortality in gangrenous patients due to sepsis and mortality observed in non-gangrenous group were not related to the anastomotic leak or sepsis.
MORTALITY
Our of 20 cases analysed, there were 4 deaths giving a mortality of 20% . whereas mortality in J.R.Anderson&Lee series 10 was 20.9%.
Griffin series6 -mortality is 40% . Sankaran V14- mortality is 25%.
Gangrenous —> 2 deaths out of 5 patients (40%.) 15
Viable - 2 deaths out of 15 patients ( 13.3%). 16
In the gangrenous groups, both the deaths were due to septicaemic shock. 17-19
MORTALITY AND AGE
Out of 4 deaths in a series of 20 cases analysed, following was the percentage of mortality in different age groups.
Table 12. Mortality and age
|
Age group |
Mortality |
Percentage |
|
11-30 (5 cases) |
Nil |
0% |
|
31-50 (7 cases) |
2 |
14.3% |
|
51-70 (6 cases) |
2 |
33.4% |
|
71-80 (2 cases) |
Nil |
0% |
Conclusion
Sigmoid volvulus is common in old age group in 5th and 6th decade with almost equal incidence in both sexes. Most common predisposing factor is long mesosigmoid with redundant colon. In gangrenous colon, procedure of choice is hartmanns procedure and in non gangrenous colon, presection and anastomosis or sigmoidopexy and derotation can be done though derotation is associated with risk of recurrence.
References
1. Richard M. Devine, M.D., F.A.C.S. Mayo Clinic Rochester, Minnesota Colonic volvulus.
2. Hughes L.E FRCS,FRACS .Royal Brisbane Hospital, Australia The Medical Journal of Australia, The Place of immediate resection in the management of sigmoid volvulus. 1968;268-273.
3. Atamanalp S S, Yildirgan M I, Bas.ogluM.MecitKantarci, Ismail Yilmaz Ataturk University School of Medicine Turkey Sigmoid colon volvulus in children: Review of 19 cases Paed Surg lnt 2004;20:492-495
5. R.S.Sinha. A clinical appraisal of volvulus of the pelvic colon with special reference to aetiology and treatment. British Journal of Surgery 1969;59(11).
6. J.R.Anderson and D.Lee. The management of acute sigmoid volvulus : British Journal of Surgery 1981;68.
Griffin, W.D., Barton J.R. and Meyer, K.A. “Volvulus to the sigmoid colon, a report of 25 cases. “SurgGynecObstct 1945; 181, 287.
7.Khanna AK, Kumar P, Khanna R. Sigmoid volvulus: study from a north Indian hospital. Dis Colon Rectum. 1999 Aug; 42(8): 1081-4.
8.R.S.Sinha. A clinical appraisal of volvulus of the pelvic colon with special reference to aetiology and treatment. British Journal of Surgery : 1969 : Vol: 59 No. 11 November.
9.J.R.Anderson and D.LeeThe management of acute sigmodvolvulus : British Journal of Surgery : Vol:68 (1981)..
10.De. U. Sigmoid volvulus in rural Bengal. Trop Doct. 2002. Apr; 32(2): 80-2.
11.Diaz-Plasencia J, Sanchez C, Bardales M et al. Operative mortality in sigmoid volvulus. Rev Gastroenterol Peru. 1993; 13 (1) : 37-44.
12.Peoples JB, McCafferty JC, Scher KS. Operative therapy for sigmoid volvulus. Identification of risk factors affecting outcome. Dis Colon Rectum 1990;33:643-6.
13.LarkimoJO, ThakisoTB, WaidronR, Barry K;Recurrent sigmoid volvulus- early resection may obviate later emergency resection. 2009 April 91(3); 2059.
14.Sankaran V. Volvulus in South India, IndJrSurg, 1962; 24: 784-90.
15.Khan M, Ullah S, Jan MAU, Naseer A, Ahmad S, Rehman A. Primary anastomosis in the management of acute sigmoid volvulus with out colonic lavage. J Postgard Med Inst 2007; 21:305-8.
16.Agaoglu N, Yucel Y, Turkyilmaz S, Surgical treatment of the sigmoid volvulus. Acta Chir Belg 2005 Aug; 105(4):365-8.
17.Lau KC, Miller BJ, Schache DJ, Cohen JR. A study of large-bowel volvulus in urban Australia. Can J Surg 2006 Jun; 49(3):203-7.
18.Turan M1, Sen M, Karadayi K et al. Our sigmoid colon volvulus experience and benefits of colonoscope in detortion process. Rev Esp Enferm Dig. 2004 Jan;96(1):32-5.
19.Hadi A, KHAN N, Shah SMA, Bangash A, Emergency management of sigmoid Volvulus: experience of Lady Reading Hospital Peshawar. J Postgrad Med Inst Jan – Mar 2006; 20(1):82-5.
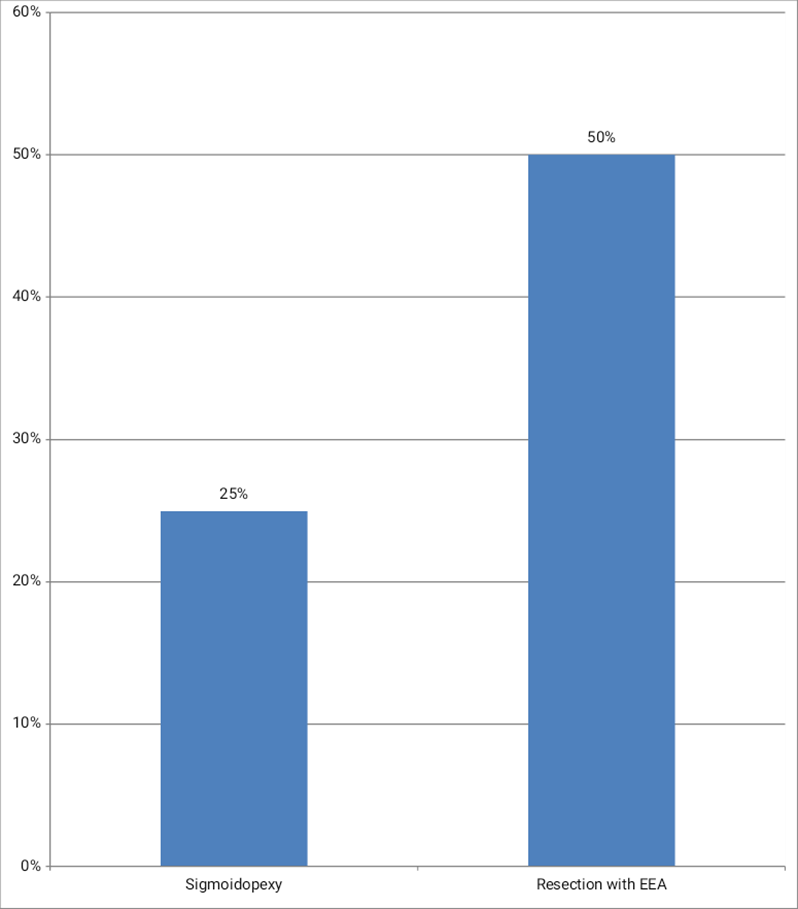
Figure 1
