The use of ICSI for the Treatment of Blastocysts, Pregnancy
The use of ICSI for the Treatment of Blastocysts, Pregnancy
Dr. Archana Singh1, Dr. Varsha Ojha’s*
1. Dr Archana Singh, IVF specialist, Obstetrician and Gynecologist, IndraIVF, Jodhpur, India.
*Correspondence to: Dr .Varsha Ojha, Specialist Obstetrician and Gynecologist, Prime Hospital, Dubai, UAE.
Copyright
© 2024 Dr Varsha Ojha. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 21 Sept 2024
Published: 27 Sept 2024
The use of ICSI for the Treatment of Blastocysts, Pregnancy
Introduction
ICSI has given lot of hope to male infertility patients, this revolutionary technique gave smiles to millions of childless couples.
ICSI: Intracytoplasmic Sperm Injection (ICSI) is performed as an additional part of an IVF treatment cycle where a single sperm is injected into each egg to assist fertilization using very fine micro-manipulation equipment. In most cases, ICSI can be used to overcome severe male infertility.
ICSI for low sperm count : ICSI involves collecting a sperm sample and cleansing it to isolate the strongest, healthiest sperm. Then a single sperm is collected and injected directly into the egg for fertilization. IVF with ICSI is often the best treatment option for men with low sperm count.
ICSI for OLIGOASTHENOTERATO: Oligoasthenoteratozoospermia (OAT) is a condition that includes oligozoospermia (low number of sperm), asthenozoospermia (poor sperm movement), and teratozoospermia (abnormal sperm shape). OAT is the most common cause of male subfertility.
ICSI for AZOOSPERMIA: Azoospermia is the medical term used when there are no sperm in the ejaculate. It can be “obstructive,” where there is a blockage preventing sperm from entering the ejaculate, or it can be “nonobstructive” when it is due to decreased sperm production by the testis.
ICSI for Unexplained infertility: Intra-Cytoplasmic Sperm Injection (ICSI) has been suggested for couples whose infertility is unexplained, as its use may bypass potential fertilization barriers causing the couples' infertility [8]. ICSI was introduced in 1992 to treat couples with male factor infertility
ICSI for TESA TESE PESA: PESA involves passing a fine needle through the skin into the epididymis to obtain sperm. TESA involves passing a fine needle through the skin directly into the testes and retrieving a small number of the seminiferous tubules themselves.
TESA or testicular sperm aspiration is performed by inserting a needle in the testis and aspirating fluid and tissue with negative pressure. The aspirated tissue is then processed in the embryology laboratory and the sperm cells extracted are used for ICSI.
ICSI for Cryptozoospermia: Intracytoplasmic sperm injection (ICSI) is well established and provides patients with severely impaired sperm quality with an opportunity to father a child. However, previous studies do not clearly indicate whether male with cryptozoospermia should use testicular sperm or ejaculated sperm for ICSI
ICSI for Obstructive & Non-obstructive cases: ICSI using spermatozoa from patients with acquired obstructive azoospermia resulted in significantly higher fertilization and pregnancy rates as compared to CAVD and non-obstructive cases.
Figure 1, 2,3
Conclusion
The progression to blastocyst and the likelihood of conceiving a viable pregnancy were unaltered by ICSI. Thus, it seems appropriate for programs to offer BT to patients undergoing ICSI using the same inclusion criteria applied to the patients.
References
1. Gardner DK, Schoolcraft WB, Wagley L, Schlenker T, Stevens J, Hesla J. A prospective randomized trial of blastocyst culture and transfer in in-vitro fertilization. Hum Reprod. 1998;13:3434–3440. [PubMed] [Google Scholar]
2. Patton PE, Sadler-Fredd K, Burry KA, Gorrill MJ, Johnson A, Larson JM, Wolf DP. Development and integration of an extended embryo culture program. Fertil Steril. 1999;72:418–422. [PubMed] [Google Scholar]
3. Milki AA, Hinckley MD, Fisch JD, Dasig D, Behr B. Comparison of blastocyst transfer with day 3 embryo transfer in similar patient populations. Fertil Steril. 2000;73:126–129. [PubMed] [Google Scholar]
4. Racowsky C, Jackson K, Celeniak NA, Fox JH, Hornstein MD, Ginsburg ES. The number of eight-cell embryos is a key determinant for selecting day 3 or day 5 transfer. Fertil Steril. 2000;73:558–564. [PubMed] [Google Scholar]
5. Toledo AA, Wright G, Jones AE, Smith SS, Johnson-Ward J, Brockman WW, Ng F, Wininger JD. Blastocyst transfer: A useful tool for reduction of high-order multiple gestations in a human assisted reproduction program. Am J Obstet Gynecol. 2000;183:377–379. [PubMed] [Google Scholar].

Figure 1
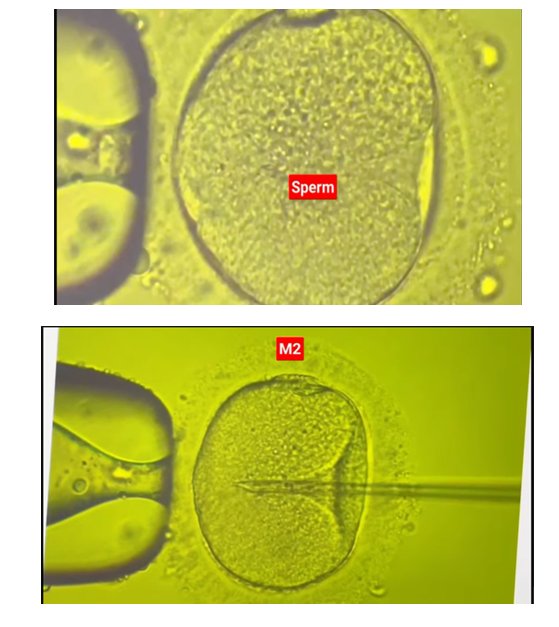
Figure 2
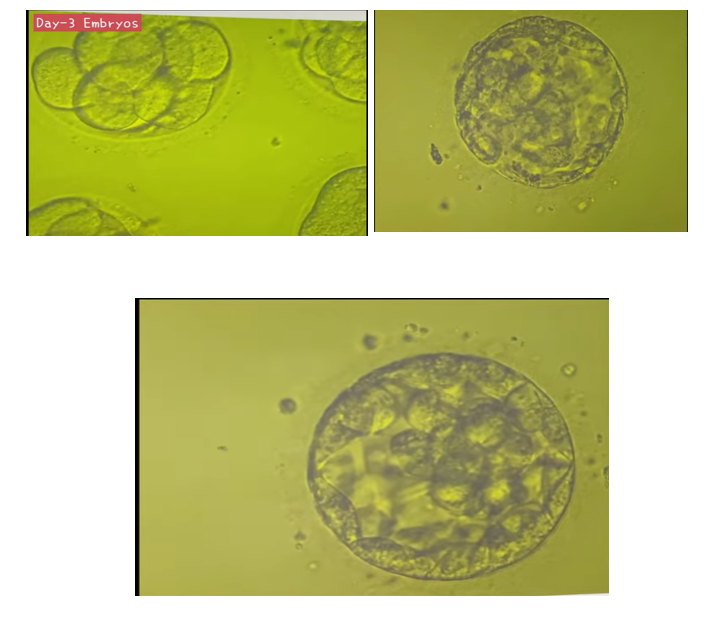
Figure 3
