Prevalence of Pseudoexfoliation Syndrome and Associated Factors among Adult Patients attended Menelik II Comprehensive Referral Hospital: Cross-Sectional Study
Prevalence of Pseudoexfoliation Syndrome and Associated Factors among Adult Patients attended Menelik II Comprehensive Referral Hospital: Cross-Sectional Study
Dr. Daniel Gebreegziabher Baraki *, Dr. Abeba Teklegiorgis Weldegiorgis2, Dr. Abiye Mulugeta Alemu3, Dr. Tesfaye Tadesse Dumecha4
1. Dr. Daniel Gebreegziabher Baraki, Glaucoma Fellow, Department Of Ophthalmology, Addis Ababa University, Ethiopia.
2. Dr. Abeba Teklegiorgis Weldegiorgis MD, Ass. Professor of Ophthalmology, Glaucoma Surgeon, CHS), Addis Ababa University, Ethiopia
3. Dr. Abiye Mulugeta Alemu MD, Ass. Professor of Ophthalmology Glaucoma Surgeon, CHS), Addis Ababa University, Ethiopia.
4. Dr. Tesfaye Tadesse Dumecha Assistant Professor of Ophthalmology Glaucoma Surgeon, CHS), Addis Ababa University, Ethiopia.
*Correspondence to: Dr. Daniel Gebreegziabher Baraki Glaucoma Fellow, Department Of Ophthalmology, Addis Ababa University, Ethiopia.
Copyright
© 2024 Dr. Daniel Gebreegziabher Baraki. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 13 September 2024
Published: 01 October 2024
Abstract
Background: Pseudoexfoliation syndrome is an age-related disorder characterized by the deposition of a distinct fibrillar extracellular material in various tissue and organs of the body. Ocular conditions including glaucoma and cataract are usually seen in patients with pseudoexfoliation syndrome. PEX etiopathogenesis involves both genetic and environmental factors. The lysyl-oxidase-like 1(LOXL1) gene, has been identified as strong genetic risk factors for PEX syndrome.
Objective To assess prevalence of pseudoexfoliation syndrome and associated factors among adult outpatients attended Menelik II Referral Hospital, Addis Ababa, Ethiopia from April to May 2024.
Methodology: A Hospital based cross sectional study was conducted among 334 adult outpatients who had attended Menelik II Referral Hospital from April to May 2024. Data was collected by PI using structured questionnaire then entered to SPSS version 26 for analysis. The descriptive statistics summarized and presented using summary statistics such as frequency tables and graphs. Binary logistic regression is used to identify candidate variables. Variables with p-value < 0.2 in binary logistic regression are further entered into a multivariable logistic regression model. Adjusted odds ratio with 95% CI is used to determine the strength of association and variables having p-values of less than 0.05 is considered as statistically significant. The final result of the analysis was presented by tables and graphs.
Result: A total of 334 adults participated in the study with a response rate of 93.3%. The median (±IQR) age of study respondents was 60(±12) years and 53.3% were males. The proportion pseudoexfoliation syndrome was 37.1% [95% CI 31.7%, 41.9%]. The mean IOP and mean age were significantly higher among patients with pseudoexfoliation syndrome. Age, high IOP, glaucoma, cataract and outdoor work were significantly associated with the proportion of pseudoexfoliation. CCT was comparable between those with and without pseudoexfoliation síndrome..Thinning of CCT identified with aging.
Conclusion: The study revealed the high prevalence of pseudoexfoliation syndrome among participants aged 40 years and older, and identified significant associations of pseudoexfoliation syndrome with age, elevated intraocular pressure (IOP), glaucoma, cataract, and outdoor work. Being hospital based study not involving large population of the various regions and ethnicity of the country limits to infer the study result to the whole population. Study at large scale representing population of the country is recommended to identify related factors to pseudoexfoliation syndrome in Ethiopia.
Key words: Pseudoexfoliation syndrome, CCT, Ethiopia, Addis Ababa.
Prevalence of Pseudoexfoliation Syndrome and Associated Factors among Adult Patients attended Menelik II Comprehensive Referral Hospital: Cross-Sectional Study
ABBREVIATIONS
CCT….CENTRAL CORNEAL THICKNESS
IOP…INTRAOCULAR PRESSURE
PEX…PSEUDOEXFOLIATION SYNDROME
PXG….PSEUDOEXFOLIATIVE GLAUCOMA
Introduction
Background
The ocular condition known as Pseudoexfoliation syndrome (PEX) was initially seen in Finnish patients in 1917(1). However, there is considerable variation in the prevalence of PEX across different regions and ethnic groups (2) and these variations may be attributed to differences in examination methods, the level of awareness among both doctors and patients and also age and demographics(3).
PEX clinically characterized by the deposition of fibrillo-granular material throughout the anterior segment of the eye. It is often accompanied by elevated intraocular pressure with or without glaucomatous optic nerve and visual field damage(4). PEX is considered not only as intraocular disease but as ocular manifestation of a systemic disorder characterized by abnormal connective tissue metabolism throughout the body(5).
Statement of the Problem
Pseudoexfoliation syndrome is an ocular disorder associated to open angle glaucoma, which is known as pseudoexfoliation glaucoma and it is the most common secondary open angle glaucoma worldwide(6). PEX is an ocular condition that can affect either one or both eyes and becomes prominent as a person gets older(7). Additionally, it shows geographical and ethnic differences(8).zonular dehiscence can cause phacodonosis, lens subluxation/dislocation, and increased risk of vitreous loss during cataract extraction, thereby impacting cataract surgery techniques (7). The prevalence of pseudoexfoliation syndrome varies significantly among different ethnicities, reaching to approximately 30% in individuals from Scandinavian countries(9).
Rational of the Study
Pseudoexfoliation syndrome is an ocular disorder which varies among different regions and ethnic groups in ethiopia,and it is connected to multiple surgical complications and glaucoma. This research has several significant implications, Determining the prevalence and associated risk factors of PEX can contribute to the development intervention strategies and preventive measures to reduce the burden of PEX-related ocular complications in Ethiopia. Assessing the impact of PEX on visual acuity will help eye care professionals in Ethiopia enhance diagnostic approaches and management protocols targeted to the local population Hence, by evaluating the occurrence of pseudoexfoliation syndrome in Menelik II Referral Hospital, Addis Abeba,ethiopia it will provide valuable information about the ethnic and environmental factors distribution and clinical significance of this ocular condition and the study will contribute as valuable input for future research in this ocular condition.
Methods and Materials
Study Area
Menelik II Referral Hospital is located in Addis Ababa, the capital city of Ethiopia .It is one of the oldest hospitals in the country ,established and named after Emperor Menelik II in the late 19th century.it is tertiary eye care hospital . Moreover, Menelik II Referral Hospital is a peculiar institution in Ethiopia eye health care system, contributing tremendously in training residents and fellowship programs , research and eye care . The study has conducted among adult outpatient attending at this hospital.
Study design and period
Hospital based cross sectional study was conducted to assess the prevalence and associated factors of pseudoexfoliation syndrome among adult outpatients visiting Minilik-II Referral Hospital Addis Abeba, Ethiopia from April to May 2024
Source and study population
Source of population
All patients visiting outpatient department of Menelik II Referral Hospital during the study period
Study population
All adult patients (age >40) who visit ophthalmology department of Menelik II Referral Hospital during the study period were included.
Study unit
Consecutive patients age 40 and above visiting ophthalmology department of Menelik II Referral Hospital during the study period
Eligibility criteria
Inclusion criteria
All adult patients age above 40 were included
Exclusion criteria
Mentally or seriously ill
Patients with corneal opacity which hinders anterior segment examination
Sample size and sampling technique
The sample size needed for determining is calculated based on single population proportion formula.
By using the following assumptions:
n= (Zα/2)2 * p * (1-p) / d2
Where: n=Sample size, Z= 1.96, 95% confidence level
P=34.6%, q =1-p, d= 5%
the sample size is calculated using the single population formula above considering the proportion of PXF ,p=34.6% which is taken from a study done in Gondar ,Ethiopia 95 % confidence interval and margin error of 5%. Then the calculated sample size is N =341 plus 5% non-response rate final sample size is 358.
All consecutive patients who came during the study period were included until the required sample size obtained.
STUDY VARIABLES
Dependent variable
Pseudoexfoliation syndrome
Independent variable
Socioeconomic and demographic characteristic
Age, Sex, Occupation, personal Income, outdoor activity, coffee consumption, smoking,
Ocular characteristics IOP, VA, CCT, cataract, glaucoma
OPERATIONAL DEFINITION
Participants were identified as having pseudoexfoliation syndrome if they showed any signs of pseudoexfoliative material on the iris, pupil, or lens capsule in either eye, observed both before and after a dilated eye examination. Glaucoma was diagnosed in those with characteristic optic nerve damage or visual field defects, history of using anti-glaucoma medications or history of glaucoma surgery. participants who were exposed to direct sunlight( outdoor workers) were as considered as exposed to the sun. Additionally, individuals who consumed more than three cups of coffee daily were classified as coffee consumers.
DATA PROCESSING AND ANALYSIS
Data collection tools and procedures
After getting written informed consent a structured questionnaire was used and administered to collect demographic, lifestyle, and systemic health information. All participants were new patients taken from triage clinic. All ophthalmic examination was done by first investigator. Intraocular pressure measurement was done using Zeiss Visu plan 500(air puff tonometer), and visual acuity was assessed using illuminated Snellen chart. Comprehensive Ophthalmic examinations, slit-lamp bio-microscopy consisting full anterior segment examination to identify PEX and hand held ultrasound pachymeter ( (Keeler PachPen ) was performed after applying topical tetracaine to measure central corneal thickness. Posterior segment was assessed with Volk 90D lens after pupillary dilation with 1% tropicamide.
Data quality assurance
At the end of each day, all of the collected data was reviewed and checked for completeness and entered into a prepared data analysis software using SPSS Version 26 by the first investigator
Data processing and analysis
-> Data was entered, coded and analyzed using SPSS Version 26. Variables were compared using the appropriate statistical tests. P Values <0.05 was considered statistically significant.
-> Data was analyzed for frequency, range, mean and standard deviation of the different sociodemographic characteristics.
-> Any association of sociodemographic characters with the frequency psudoexfoliation was analyzed
Result
1. Socio-demographic Characteristics of Study Participants
This study consisted of 334 adults who are age of 40 and above, which represents 93.3% response rate and 178 of them were males and 156 were females. The mean and median age of participants was 60±11.89 and 60 respectively. The majority of the study participants were Orthodox (66.8%) followed by Muslim (21.3%), Protestant (9.9%) and Others (2.1%).
Table 1: Scio-demographic characteristics of the study participants, Menelik II Referral Hospital, Addis Ababa, Ethiopia 2024
|
Variable |
Frequency |
Percentage (%) |
|
Age(years) 40-50 51-60 61-70 >70 |
87 96 89 62 |
26.0 28.7 26.6 18.6 |
|
Sex Male Female |
178 156 |
53.3 46.7 |
|
Residence Rural Urban |
99 235 |
29.6 70.4 |
|
Religion Orthodox Muslim Protestant Other |
223 71 33 7 |
66.8 21.25 9.9 2.1 |
|
Educational level Unable to read and write Only able to read and write Primary education Secondary education College/University |
106 73 51 46 58 |
31.7 21.9 15.3 13.8 17.4 |
|
Occupation Farmer Merchant Civil servant Other |
53 22 43 216 |
15.9 6.6 12.9 64.7 |
|
Martials status Single Married Divorced Widowed Others |
19 240 18 56 1 |
5.7 71.9 5.4 16.8 0.3 |
|
Monthly income <1000 1000-2000 2001-3000 >3000 |
186 34 31 83 |
55.7 10.2 9.3 24.9 |
Pseudoexfoliation material was identified in 124 participants, representing 37.1% of the study group. Among these, 84 participants (67.74%) had bilateral pseudoexfoliation, while 40 participants (32.26%) had unilateral pseudoexfoliation.
Fig 1: Prevalence of Pseudoexfoliation Syndrome
Table 2: Ocular, Systemic and Behavioral characteristics of the study participants in Menelik II Referral Hospital, Addis Ababa, Ethiopia 2024
|
Variables |
Frequency |
Percentage (%) |
|
IOP (mmHg) OD ≤21 >21 OS ≤21 >21 |
238 96 239 95 |
71.3 28.7 71.6 28.4 |
|
Ocular condition Glaucoma Cataract |
73 166 |
21.9 49.7 |
|
Hypertension Yes No |
78 256 |
23.4 76.6 |
|
DM Yes No |
57 227 |
17.1 85.9 |
|
Sun exposure Yes No |
131 203 |
39.2 60.8 |
|
Coffee consumption Yes No |
233 101 |
69.8 30.2 |
Fig 2: Prevalence of Pseudo-exfoliation Syndrome with respect to Age
The prevalence of PXF increases as visual acuity decreases. A statistical significance association was found between lower visual acuity and a likelihood of having PXF, P Value <0.05
Table 3: Association between the level of uncorrected visual acuity and the prevalence of PXF , Menelik II Referral Hospital Addis Ababa, Ethiopia 2024
|
|
PXF PREVALENCE |
P-value |
||
|
Positive no (%) |
Negative no (%) |
?0.001 |
||
|
VA OD |
>6/18 6/18-6/60 6/60-3/60 <3/60 |
21(18.4) 21(26.6) 33(57.9) 49(58.3) |
93(81.6) 58(73.4) 24(42.1) 35(41.7) |
|
|
VA OS |
>6/18 6/18-6/60 6/60-3/60 <3/60 |
23(19.7) 14(21.9) 24(48.0) 63(61.2) |
94(80.3) 50(78.1) 26(52.0) 40(38.8) |
?0.001 |
3 Central Corneal Thickness of Study Participants
Regarding the central corneal thickness the results shows the following measurements ,Mean CCT for overall patient population was 519± 33.19( Range 421-630) microns in the right eye and 520 ±34.31 (Range 420-665) in the left eye.
Figure 3: OD Central Corneal Thickness
There was no statistically significant difference in the mean Central Corneal Thickness (CCT) between the pseudoexfoliative group (517±36) and the non-pseudoexfoliative group (520±31), with a p-value of 0.456. Similarly, there was no statistically significant difference in CCT between both eyes and across sexes (P>0.05).
A one-way ANOVA with post hoc analysis was conducted to compare the mean Central Corneal Thickness (CCT) across different age groups. The results showed that the mean CCT significantly decreases with increasing age:
• Ages 40-50: 528±33
• Ages 51-60: 522±31
• Ages 61-70: 516±32
• Ages >71: 504±31
The p-value for these differences was less than 0.05.
Figure 4: Mean CCT difference between Age groups
Table 4: Binary and multivariate logistic regression showing associated factors for Pseudo-exfoliation Syndrome among adults Addis Ababa, Ethiopia
|
Variables |
PSEUDOEXFOLIATION |
COR(95%CI) |
AOR(95%CI) |
p-value |
|
|
Positive no (%) |
Negative no (%) |
||||
|
Age (in years) 40-50 51-60 61-70 >70 |
17(19.5) 30(31.2) 37(41.6) 40(64.5) |
70(80.5) 66(68.8) 52(58.4) 22(35.5) |
7.49(3.56,15.73) 4.00(2.04,7.86) 2.56(1.31,4.99) 1.00(1.00,1.00) |
4.22(1.61,11.09) 4.35(1.79,10.58) 3.43(1.41,8.30) 1.00(1.00,1.00) |
0.003 0.001 0.006 0.005 |
|
Sex Female Male |
51(32.7) 73(41) |
105(67.3) 105(59) |
1.43(0.91,2.24) 1.00(1.00,1.00) |
0.89(0.46,1.71) 1.00(1.00,1.00) |
0.716 |
|
Occupation Outdoor work Indoor work |
83(63.4) 41(20.2) |
48(36.6) 162(79.8) |
1.00(1.00,1.00) 6.83(4.17,11.19) |
1.00(1.00,1.00) 6.39(3.36,12.16) |
0.000 |
|
Educational status Unable to read and write Able to read and write Primary education Secondary education Higher education |
65(61.3) 19(26.0) 17(33.3) 11(23.9) 12(20.7) |
41(38.7) 54(74.0) 34(66.7) 35(76.1) 46(79.3) |
1.00(1.00,1.00) 4.51(2.35,8.66) 3.17(1.57,6.39) 5.04(2.31,11,03) 6.08(2.88,12.81) |
1.00(1.00,1.00) 3.47(1.46,8.25) 2.30(0.96,5.52) 2.90(1.00,8.39) 2.62(0.95,7.23) |
0.047 0.005 0.063 0.049 0.064 |
|
Residence Rural Urban |
56(56.6) 68(28.9) |
43(43.4) 167(71.1) |
1.00(1.00,1.00) 3.20(1.97,5.21) |
1.00(1.00,1.00) 1.49(0.72,3.08) |
0.278 |
|
IOP >21 mmHg ≤21 mmHg |
56(58.3) 68(28.6) |
40(41.7) 170(71.4) |
1.00(1.00,1.00) 3.50(2.14,5.73) |
1.00(1.00,1.00) 3.54(1.80,6.95) |
0.000 |
|
Glaucoma Yes No |
42(57.5) 82(31.4) |
31(42.5) 179(68.6) |
1.00(1.00,1.00) 2.96(1.74,5.04) |
1.00(1.00,1.00) 2.43(1.19,4.97) |
0.015 |
|
Cataract Yes No |
87(52.4) 37(22.0) |
79(47.6) 131(78.0) |
1.00(1.00,1.00) 3.90(2.42,6.27) |
1.00(1.00,1.00) 2.06(1.07,3.97) |
0.030 |
|
Hypertension Yes No |
30(38.5) 94(36.7) |
48(61.5) 162(63.3) |
1.00(1.00,1.00) 1.08(0.64,1.82) |
1.00(1.00,1.00) 1.71(0.81,3.60) |
0.159 |
|
DM Yes No |
14(24.6) 110(39.7) |
43(75.4) 167(60.3) |
1.00(1.00,1.00) 0.49(0.26,0.95) |
1.00(1.00,1.00) 0.89(0.36,2.18) |
0.802 |
|
Coffee Yes No |
98(42.1) 26(25.7) |
135(57.9) 75(74.3) |
1.00(1.00,1.00) 2.29(1.40,3.76) |
1.00(1.00,1.00) 1.78(0.91,4.50) |
0.093 |
In patients with PEX, the average intraocular pressure (IOP) was 22±10.3, significantly higher than the 17.2±5.4 observed in those without PEX (p-value ?0.001). Additionally, the proportion of PEX among patients with an IOP greater than 21 mmHg was 58.3%, significantly higher compared to the 28.6% in patients with an IOP of 21 mmHg or less (p-value ?0.001).
Similarly the proportion of PXF was significantly higher in patients with glaucoma (57.5%) compared to those without glaucoma (31.4%).
The average age of patients with PEX was significantly higher at 65±12 years compared to 57±11 years for those without PEX (p-value ?0.001). Furthermore, the prevalence of PEX increased with age significantly (p-value<0.05): 19.5% among patients under 50 years, rising to 64.5% in patients over 70 years.
The proportion of PXF did not show a statistically significant difference between males and females.
The proportion of PXF was significantly higher in participants who had outdoor occupation (63.4%) than those who have indoor occupations (20.2%). Moreover the proportion of PEX was significantly higher among illiterate participants and there was no statistically significant association between PXF and coffee users (p value 0.093).
Discussion
In this study, the proportion of PEX among adults over 40 years old was 37.1% [95% CI 31.7%, 41.9%]. This is comparable to a study conducted in Gondar in 2019, which reported a prevalence of 34.6%(12), and another study in Jimma in 2009, which found a prevalence of 35.82%(7). This consistency may be attributed to the fact that these are hospital-based studies. However, this study's prevalence is higher compared to other researchs, such as studies from central Ethiopia (Baso and Worena) at 13.2% (13) , Egypt in 2009 at 4.14% (15), Greenland at 4.5% (21), and Saudi Arabia at 3.5% (22). This variation may be explained by differences in study design, with the latter studies being community-based rather than hospital-based.
In this study, the proportion of PXF significantly increases as the age increases similar to studies done between February 2005 and June 2008, in Kinshasa (16), central Ethiopia, Baso and Worena (13) 2009 and 2011 in Western India (23) and this strengthen that PEX strongly age related process.
There was no significant gender predominance in our study ,in contrast a study done in 2005 and June 2008 Kinshasa(16) showed it was higher among females This may perhaps be due to women spending most of their time carrying out more outdoor activities compared with men but a study done in Gondar,2019 showed male predominance (12).
The result of this study showed that the mean IOP was significantly high among patients with PXF and the proportion of PXF among study participants with IOP >21mmHg 58.3 %was significantly higher than those having IOP ≤21mmHg 28.6%. this result is consistent with the study done in Baso and Worena(13),Gondar (12) and Mogadishu(14).
Previous studies have demonstrated an association between glaucoma and PXF, as seen in research from Gondar(12), Egypt,(15) and Kinshasa(16). Similarly, this study also found a significantly higher proportion of glaucoma among participants with PXF (57.5%) compared to those without it (42.5%). Therefore, identifying PXF is crucial for diagnosing and managing PXG, which is an aggressive form of glaucoma.
Participants who worked outdoors had a higher proportion of PXF compared to those working indoors, consistent with findings from studies conducted in Gondar and Korea(12,19). This may be attributed to increased sun exposure, which could contribute to a higher incidence of PXF.
In this study, there was no statistically significant difference in mean central corneal thickness (CCT) between the pseudoexfoliative group (517±36) and the non-pseudoexfoliative group (520±31) with a p-value of 0.456. This contrasts with research from India(23), which found that the pseudoexfoliative group had a thinner cornea. Additionally, this study observed that corneal thickness decreases significantly with age, aligning with findings from study conducted in Lithuanian adults(28). The thinning of the cornea with age may be attributed to reduction in keratocyte density and dehydration over time.
Conclusions
The study revealed the high prevalence of pseudoexfoliation syndrome among participants aged 40 years and older, and identified significant associations of pseudoexfoliation syndrome with age, elevated intraocular pressure (IOP), glaucoma, cataract, and outdoor work. Being hospital based study not involving large population of the various regions and ethnicity of the country limits to infer the study result to the whole population. Study at large scale representing population of the country is recommended to identify related factors to pseudoexfoliation syndrome in Ethiopia
Acknowledgmnt
We want to extend our heartfelt thanks to all the staff who were supportive throughout the study. We are also deeply grateful to the study participants for their cooperation and willingness which made this study possible. Our appreciation goes to the Department of Ophthalmology for the opportunity to carry out this research.
References
1. Lindberg JG. Clinical investigations on depigmentation of the pupillary border and translucency of the iris in cases of senile cataract and in normal eyes in elderly persons. Acta Ophthalmol Suppl. 1989;190:1–96. https://europepmc.org/article/med/2541596
2. Forsius H. Exfoliation syndrome in various ethnic populations. Acta Ophthalmol (Copenh). 1988;66(S184):71–85. https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1755-3768.1988.tb02633.x
3. AASVED H. THE GEOGRAPHICAL DISTRIBUTION OF FIBRILLOPATHIA EPITHELIOCAPSULARIS: so?called senil exfoliation or Pseudoexfoliation of the anterior lens capsule. Acta Ophthalmol (Copenh). 1969;47(3):792–810. https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1755-3768.1969.tb08170.x
4. Prince AM, Ritch R. Clinical signs of the pseudoexfoliation syndrome. Ophthalmology. 1986;93(6):803–7. https://www.sciencedirect.com/science/article/pii/S0161642086336649
5. Streeten BW, Li ZY, Wallace RN, Eagle RC, Keshgegian AA. Pseudoexfoliative fibrillopathy in visceral organs of a patient with pseudoexfoliation syndrome. Arch Ophthalmol. 1992;110(12):1757–62. https://jamanetwork.com/journals/jamaophthalmology/article-abstract/639982
6. Ritch R, Schlötzer-Schrehardt U. Exfoliation syndrome. Surv Ophthalmol. 2001;45(4):265–315. https://www.sciencedirect.com/science/article/pii/S003962570000196X
7. Yeshigeta G, Yemariamwork T. Clinical Characteristics of Cataract Patients with Pseudoexfoliation Syndrome at Jimma University Specialist Hospital, South West Ethiopia. Ethiop J Health Sci. 2012;22:1–6. https://www.ajol.info/index.php/ejhs/article/view/77665
8. Jackson TL. Moorfields manual of ophthalmology. JP Medical Ltd; 2019. https://books.google.com/books?hl=en&lr=&id=qTcTEAAAQBAJ&oi=fnd&pg=PR1&dq=8.+Jackson+TL.+Moorfields+manual+of+ophthalmology.+JP+Medical+Ltd%3B+2019.&ots=KfiYDKBT1k&sig=FYowK7g-DnkAVjsowWz-lQMOR5k
9. Rhee DJ. Color Atlas and Synopsis of Clinical Ophthalmology--Wills Eye Institute--Glaucoma. Lippincott Williams & Wilkins; 2012. https://books.google.com/books?hl=en&lr=&id=vbWWuX1dgjYC&oi=fnd&pg=PP2&dq=9.+Rhee+DJ.+Color+Atlas+and+Synopsis+of+Clinical+Ophthalmology--Wills+Eye+Institute--Glaucoma.+Lippincott+Williams+%26+Wilkins%3B+2012.&ots=UWo0JSVVCs&sig=VCoxGY6tKqCpot0rYUMiuKAsASg
10. Teshome T, Regassa K. Prevalence of pseudoexfoliation syndrome in Ethiopian patients scheduled for cataract surgery. Acta Ophthalmol Scand. 2004;82(3p1):254–8. https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1395-3907.2004.00263.x
11. Bedri A. Pseudoexfoliation syndrome in Ethiopian glaucoma patients. East Afr Med J. 1999;76(5). https://www.ajol.info/index.php/eamj/article/view/159535
12. Yibekal BT, Adimassu NF, Ayele FA. Pseudoexfoliation syndrome and associated factors among adults at Gondar University comprehensive specialized hospital tertiary eye care and training center: a cross-sectional study. Clin Optom. 2021;249–55. https://www.tandfonline.com/doi/abs/10.2147/OPTO.S321716
13. Berhanu YA, Giorgis AT, Alemu AM. Prevalence of ocular pseudoexfoliation in Baso and Worena District, central Ethiopia. Ethiop J Health Dev. 2020;34(1). https://www.ajol.info/index.php/ejhd/article/view/201291
14. Kalayc? M. Pseudoexfoliation syndrome prevalence in Somali patients with senile cataract. Istanb Med J Istanb Tip Derg. 2020;21(5):380. https://www.researchgate.net/profile/Mustafa_Kalayci5/publication/344194681_Pseudoexfoliation_Syndrome_Prevalence_in_Somali_Patients_with_Senile_Cataract/links/5f5a8658a6fdcc1164092580/Pseudoexfoliation-Syndrome-Prevalence-in-Somali-Patients-with-Senile-Cataract.pdf
15. Shazly TA, Farrag AN, Kamel A, Al-Hussaini AK. Prevalence of pseudoexfoliation syndrome and pseudoexfoliation glaucoma in Upper Egypt. BMC Ophthalmol. 2011;11(1):1–6. https://link.springer.com/article/10.1186/1471-2415-11-18
16. Kaimbo W, Kaimbo D. Pseudoexfoliation syndrome in Congolese patients. J Fran Ophthalmol. 2012; 35 (1): 40-5. https://www.sciencedirect.com/science/article/pii/S0181551211003135
17. Romero-Aroca P, Masip-Serra R, Martínez-Salcedo I, Salvat-Serra M, Fernández-Ballart J, Bautista-Pérez Á. High prevalence of pseudoexfoliation syndrome and its complications in Tarragona in northeast Spain. Eur J Ophthalmol. 2011;21(5):580–8. https://journals.sagepub.com/doi/abs/10.5301/EJO.2011.6254
18. Rao RQ, Arain TM, Ahad MA. The prevalence of pseudoexfoliation syndrome in Pakistan. Hospital based study. BMC Ophthalmol. 2006;6(1):1–5. https://link.springer.com/article/10.1186/1471-2415-6-27
19. Kim S, Lim SH, Sung KR, Yun SC, Kim CY, Park KH, et al. Prevalence of pseudoexfoliation syndrome and associated factors in south koreans: the korean national health and nutrition examination survey. Ophthalmic Epidemiol. 2016;23(5):298–302. https://www.tandfonline.com/doi/abs/10.3109/09286586.2015.1131992
20. Åström S. Long-term follow-up of pseudoexfoliation, intraocular pressure and glaucoma: epidemiological studies in northern Sweden. 2013; https://www.diva-portal.org/smash/record.jsf?pid=diva2:599875
21. Ostenfeld?Åkerblom A. Pseudoexfoliation in Eskimos (Inuit) in Greenland. Acta Ophthalmol (Copenh). 1988;66(4):467–8. https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1755-3768.1988.tb04042.x
22. Al-Saleh SA, Al-Dabbagh NM, Al-Shamrani SM, Khan NM, Arfin M, Tariq M, et al. Prevalence of ocular pseudoexfoliation syndrome and associated complications in Riyadh, Saudi Arabia. Saudi Med J. 2015;36(1):108. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4362197/
23. Rao V, Doctor M, Rao G. Prevalence and prognosis of pseudoexfoliation glaucoma in western India. Asia-Pac J Ophthalmol. 2015;4(2):121–7. https://journals.lww.com/apjoo/fulltext/2015/03000/Prevalence_and_Prognosis_of_Pseudoexfoliation.14.aspx
24. Mitchell P, Wang JJ, Hourihan F. The relationship between glaucoma and pseudoexfoliation: the Blue Mountains Eye Study. Arch Ophthalmol. 1999;117(10):1319–24. https://jamanetwork.com/journals/jamaophthalmology/article-abstract/412473
25. Young A, Tang W, Lam D. The prevalence of pseudoexfoliation syndrome in Chinese people. Br J Ophthalmol. 2004;88(2):193. https://bjo.bmj.com/content/88/2/193.short
26. Lee J, Ho S. The Prevalence of Pseudoexfoliation Syndrome in a Singapore Eye Clinic. Invest Ophthalmol Vis Sci. 2010;51(13):1313–1313. https://iovs.arvojournals.org/article.aspx?articleid=2370006
27. Nishat Sultana S. Evaluation of Central Corneal Thickness and clinical ocular profile of Patients presenting with Pseudoexfoliation at a tertiary care centre. Indian J Clin Exp Ophthalmol. 2019;5(4):543–51. https://www.academia.edu/download/63370709/IJCEO-5-4-543-55120200520-12935-1yvr6m1.pdf
28. Galgauskas S, Juodkaite G, Tutkuvien? J. Age-related changes in central corneal thickness in normal eyes among the adult Lithuanian population. Clin Interv Aging. 2014;1145–51. https://www.tandfonline.com/doi/abs/10.2147/CIA.S61790.
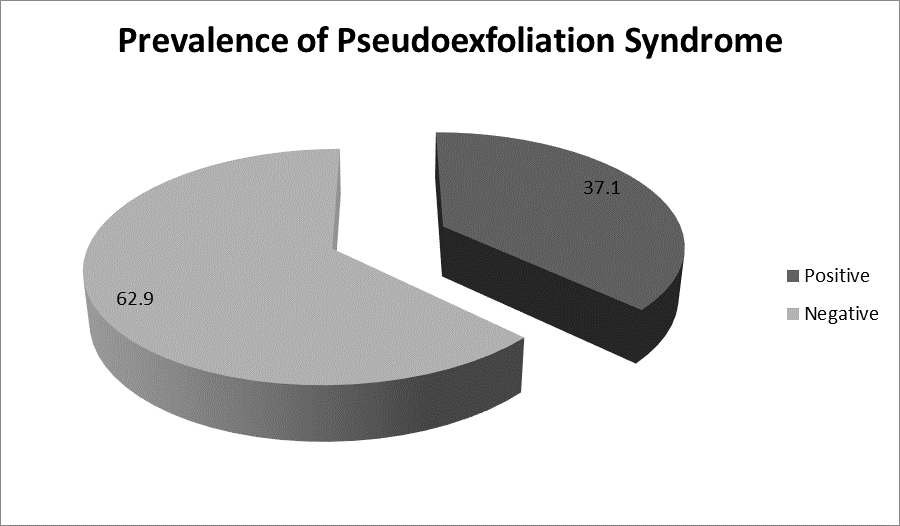
Figure 1
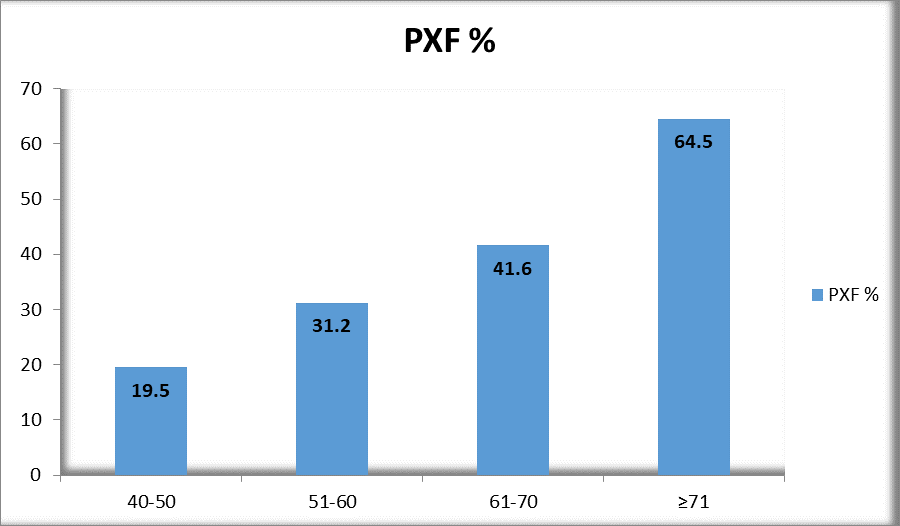
Figure 2
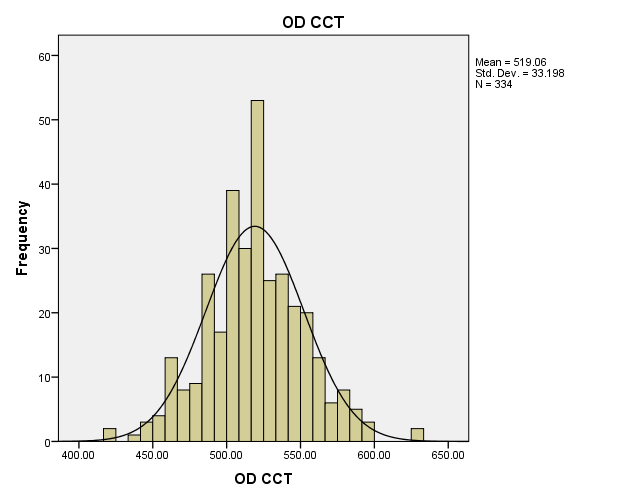
Figure 3
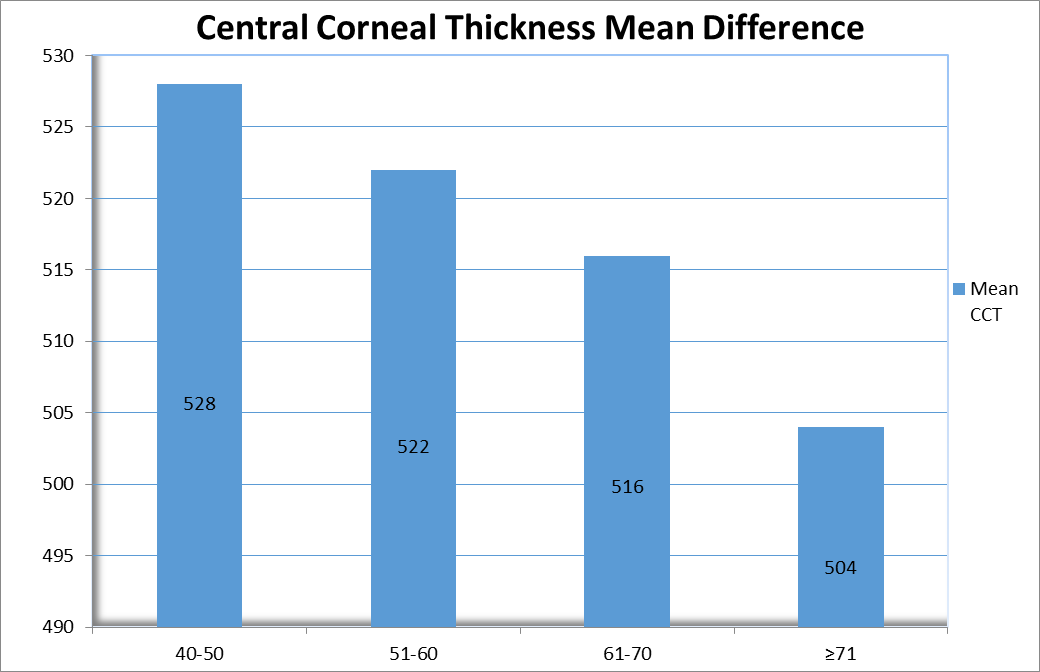
Figure 4
