Pattern of Patients Visiting Oculoplasty Clinic at Saint Paul’s Hospital Millennium Medical College
Pattern of Patients Visiting Oculoplasty Clinic at Saint Paul’s Hospital Millennium Medical College
Gebeyaw Molla*1, Asrat Sime2, Seblewongel Eshetu3, Tariku shimelis4
1,2,3,4. Saint Paul's Hospital Millennium Medical College.
*Correspondence to: Gebeyaw Molla, Saint Paul's Hospital Millennium Medical College.
Copyright
© 2024 Gebeyaw Molla. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 16 September 2024
Published: 01 October 2024
Abstract
Background: Oculoplasty is a subspecialty within ophthalmology that encompasses the medical and surgical management of conditions affecting the eyelids, lacrimal system, and orbit. It also includes procedures related to facial rejuvenation and cosmetic enhancement. Despite its relevance, there is a notable absence of published epidemiological studies in Ethiopia, as well as a limited number of research endeavors conducted across Africa.
Objective: This study aims to characterize the pattern of patients visiting Oculoplasty Clinic, Saint Paul’s Hospital Millennium Medical College from January to December 2022.
Methods: A hospital-based prospective cross-sectional study was carried out during the period from January 1, 2022, to December 1, 2022. The study enrolled 250 participants. Data collection involved the use of a structured questionnaire and a data collection format designed to document ocular examination findings. Trained residents and nurses collected the data, while ocular examinations were performed by an Oculoplasty surgeon. Data analysis was conducted using SPSS version 26. Descriptive statistics, including frequency and cross-tabulation, were employed to analyze the pattern of patients visiting Oculoplasty clinic.
Results: The study revealed a slight female predominance (53.6%) among the patient population. The majority of individuals attending the Oculoplasty clinic fell within the 31-60 age range (38.4%), followed by the 15-30 age group (28.4%). Urban residents accounted for approximately 56.4% of the patients, with a significant portion (45.4%) being employed by the government. Regarding disease onset, the majority of patients (72.4%) sought medical attention at the clinic more than 6 months after symptom onset, while 16% presented between 6 weeks and 6 months. The study's findings indicate that the most prevalent disease entity was NLDO (17.6%), followed by blepharoptosis (7.6%). Among the disease categories, lacrimal disorders (43.6%) ranked highest, succeeded by orbital disorders (25.6%), eyelid conditions (21.6%), and a combination of the aforementioned categories (9.2%).
Conclusion: The study's outcomes underscore lacrimal disorders as the foremost conditions encountered in the oculoplasty clinic, with NLDO being prominent among adults and CNLDO among pediatric patients. The results also hint at a slight bias toward female patients and a worrisome tendency of delayed presentation among individuals seeking treatment.
Key words: Ophthalmology Oculoplasty Profile Eyelid Lacrimal apparatus Orbit.
Pattern of Patients Visiting Oculoplasty Clinic at Saint Paul’s Hospital Millennium Medical College
ABBREVIATIONS
ADC: acute dacryocystitis
BCC: basal cell carcinoma
CDC: chronic dacryocystitis
CNLDO: Congenital nasolacrimal duct obstruction
CPEO: congenital progressive external ophthalmoplegia
DC: dacryo-Cutaneous
DCR: dacryocystorhinostomy
GET: Global Eradication of trachoma
ICD: International classification of disease
IOIS: idiopathic orbital inflammatory syndrome
NLDO: Nasolacrimal duct obstruction
OR: Operation room
RE: Refractive error
RLL: right lower lid
SPHMMC: Saint Paul’s hospital millennium medical college
SPSS- statistical program for social sciences
TED: Thyroid eye disease
TT: Trachomatous trichiasis
WHO: World health organization
Introduction
Oculoplasty disorders can manifest as lesions affecting various areas including the orbital, ocular, lacrimal, lid, and adnexal regions. These conditions may arise from congenital anomalies, involutional changes, trauma, metabolic disorders, and tumors. Such issues can lead to visual impairment, anatomical deformities, and aesthetically displeasing appearances, increasing the risk of psychological and socioeconomic isolation as well as educational disadvantages (1).
Diverse eyelid disorders exhibit varying clinical presentations and prognosis. Epithelial skin lesions around the eyes can result in significant cosmetic complications, obstruct vision, and alter the natural form and function of the eyelid. Eyelid lesions can be categorized as non-neoplastic or neoplastic (1). Notably, there is no consolidated prevalence study available on this topic in Ethiopia.
Lacrimal disorders encompass conditions affecting the lacrimal gland and drainage system. These disorders impact quality of life and may predispose individuals to secondary ocular infections. However, the epidemiology of lacrimal disorders remains insufficiently explored, with existing studies often limited to specific clinics, individual specialists, or single disorders (1). The same is true for orbital disorders which encompass pathologies involving structures within the bony cone.
While a number of Oculoplasty related prevalence studies have been conducted in Africa and other parts of the world, the amount of research remains limited. In a study conducted at a teaching institution in Port Harcourt, Nigeria, the most affected demographic consisted of females aged 21 to 30, and chalazion was the most common pathology (11). Another study at a tertiary care center in Singapore revealed that eyelid disorders were the most frequent, followed by orbital disorders (5).
There is a scarcity of comprehensive epidemiological studies on the incidence of Oculoplasty disorders, both in terms of quantity and scope. As far as my knowledge extends, no reports detailing the prevalence of Oculoplasty disorders in Ethiopia have been published. Therefore, this study aims to assess the prevalence of oculoplasty disorders in a tertiary hospital in Addis Ababa. The objective is to highlight the epidemiological features of Oculoplasty disorders in Ethiopia.
1.1 Background
Oculoplasty, within the realm of ophthalmology, encompasses the medical and surgical treatment of conditions involving eyelids, lacrimal system, and orbital structures. Additionally, this field includes cosmetic procedures and facial rejuvenation. The orbit, a cavity housing the globe, extraocular muscles, neurovascular components, and orbital fat, plays a pivotal role. Similarly, the eyelid, part of the orbital adnexa, comprises the skin, subcutaneous connective tissue, muscles responsible for protraction, orbital septum, orbital fat, retraction muscles, tarsus, and conjunctiva. Moreover, the lacrimal system, another element of the orbital adnexa, encompasses the lacrimal gland and drainage structures. Notably, despite the significance of these fields, no epidemiological studies have been conducted in Ethiopia, and only a limited number of research endeavors have taken place in Africa.
Objectives
General objective
To determine the pattern of patients visiting oculoplasty clinic at saint Paul’s hospital millennium medical college from Jan 2022 to Dec 2022
Specific objectives
To determine the pattern of patients with eyelid disorders in the study
To assess the pattern of patients with lacrimal disorders in the study period
To determine the pattern of patients with orbital disorders in the study period
Methodology
Study area
The research was carried out at SPHMMC, situated in Gulele sub-city, Addis Ababa, Ethiopia. SPHMMC was founded in 1969 through a partnership with the German evangelical church. Initially named St. Paul’s Hospital by Emperor Haile Sellassie I, it started with a nursing program and eventually evolved to offer undergraduate medical training in 2007, earning the name 'millennium'. It plays a significant role as a major tertiary referral center in Ethiopia. Within the college, the Ophthalmology department stands out, attending to over 40,000 patients and conducting more than 2,500 surgeries annually.
A notable unit within the Ophthalmology department is the Oculoplasty clinic, known for its active provision of both medical and surgical services.
Study design
A cross-sectional study was carried out on patients visiting oculoplasty clinic, SPHMMC from January to December 2022.
Source population
During the designated research timeframe, individuals who are new to SPHMMC and are seeking care from the Oculoplasty clinic within the Department of Ophthalmology were included in the study.
Study population
During the research timeframe, all individuals who received diagnosis related to eyelid, lacrimal and orbital disorders either separately or in combination.
Exclusion criteria
Patients managed at other clinics or minor OR and sent home,
Patients on follow up and
Patients who refused to be investigated despite the physician’s recommendation
Inclusion criteria
All new patients visiting oculoplasty clinic from January to December 2022
Study period
The study was conducted from January to December 2022
Sampling technique
Sample size was calculated using correction formula
- n=n/1+((n-1)/N)
- n = corrected sample size
- n = sample size calculated early which is 423
- N = total number of population in the study area
- 10% non respondent rate
With this formula, the sample size calculated to be 173.
Data Collection Procedures
Data was obtained through a structured questionnaire encompassing all essential variables. Pertinent historical information was gathered from the patient, their parents, legal guardian and in participants above 13 years old to 18 years old we take consent from both the participants and parents using their own language. Details regarding location and type of lesion were documented, along with any diagnostic procedures employed. Demographic information and diagnosis particulars were compiled, and the presenting conditions were categorized in accordance with the 10th Revision of the ICD introduced in 1992. Demographic data encompassed age, gender, and place of residence. All recorded cases were from an outpatient setting run by oculoplasty surgeon. The data collection process was conducted by ophthalmology residents at the department following orientation to the data collection format, and the charts were subsequently reviewed by the principal investigator
Data Quality assurance
The quality of data was assured through proper training of data collectors, careful design, proper categorization and filling. Regular supervision and checking for its accuracy and completeness was done by principal investigator.
Data analysis procedure
The collected data was cleared and checked for completeness. SPSS version 26 was used for the descriptive data analysis using cross tabulation and frequency
Result
In this study, 250 patients were included. The results indicated a slight overall female predominance, with females comprising 53.6% of the patients. When examining each category of disease, it was observed that 68.80% of patients with lacrimal disease were females, while 64.81% of patients with eyelid diseases were males. For orbital diseases, 55.5% of the patients were females.
The most common age group of patients visiting the Oculoplastics clinic was between 31-60 years, accounting for 38.4% of the cases. The second most common age group was 15-30 years of age, representing 28.4% of the cases. Children from birth to 14 years of age accounted for 18.8% of the cases, and the remaining 14.4% were patients above 60 years of age.
Upon analyzing patients with only lacrimal diseases, the majority of cases fell within the age range of 31-60 years (46.7%). For patients with eyelid diseases, the majorities were between 15-30 years of age (29.6%). In the orbital disease category, the majority of patients were seen between 31-60 years of age (34.3%).
Regarding the patients' residential areas, approximately 56.4% lived in urban areas. In terms of occupation, the majority of patients (45.4%) worked for the government, while non-governmental/self-employed patients represented a distant second at 17.6%, followed by farmers at 15.1%.
Table 1: socio-demographic data of participants visiting oculoplasty clinic from January to December 2022
|
Variables |
Category |
Number of cases |
Percent |
|
Gender |
Male |
116 |
46.4 |
|
Female |
134 |
53.6 |
|
|
Age in years |
0-14 |
47 |
18.8 |
|
15-30 |
71 |
28.4 |
|
|
31-60 |
96 |
38.4 |
|
|
>60 |
36 |
14.4 |
|
|
Residency |
Rural |
109 |
43.6 |
|
Urban |
141 |
56.4 |
|
|
Occupation |
Governmental |
93 |
37.2 |
|
Non-governmental/self employed |
36 |
14.4 |
|
|
Farmer |
31 |
12.4 |
|
|
Retired |
21 |
8.4 |
|
|
Housewife |
24 |
9.6 |
Table 2: gender and age of presentation of participants visiting oculoplasty clinic from January to December 2022
|
Variables |
Category |
Eyelid |
lacrimal |
Orbital |
combination of lacrimal, eyelid, orbital and neuroophthalmic |
|
Gender |
Male |
35 |
34 |
28 |
18 |
|
Female |
19 |
75 |
35 |
5 |
|
|
Age in years |
0-14 |
15 |
17 |
15 |
0 |
|
15-30 |
16 |
27 |
20 |
8 |
|
|
31-60 |
15 |
51 |
22 |
8 |
|
|
Above 60 |
8 |
14 |
7 |
7 |
Stratifying patients based on the duration of their complaint reveals that the majority of patients (72.4%) visited the clinic more than 6 months after the onset of their disease. The second most common timeframe for clinic visits was between 6 weeks and 6 months (16%), while the remaining patients (11.6%) sought medical attention within the initial 6 weeks of disease onset. Specifically, approximately 89.9% of patients with lacrimal disorders, as well as 61.11% and 60.93% of those with eyelid and orbital disorders respectively, presented to the clinic after 6 months of disease onset. Additionally, 81.6% of the participants in our study have had a unilateral disease.
Table 3: duration of disease onset and gender of the participants visiting oculoplasty clinic from January to December 2022
|
Variables |
Eyelid |
Orbital |
Lacrimal |
combination of lacrimal, eyelid, orbital and neuro ophthalmic |
Total |
|
less than 6 weeks |
11 |
2 |
10 |
6 |
29 |
|
6 weeks to 6 months |
10 |
9 |
15 |
6 |
40 |
|
Greater than 6 months |
33 |
98 |
39 |
11 |
181 |
|
Male |
35 |
34 |
29 |
18 |
116 |
|
Female |
19 |
75 |
35 |
5 |
134 |
Out of all the participants in the study, only 15.2% had experienced ocular trauma and just 4.8% had undergone previous ocular surgery. When examining the number of patients investigated, 13.6% had received a CT scan, 4.4% had undergone an MRI/MRV, and 4.4% had undergone histopathology
Table 4: history of trauma, surgery and investigation done for the participants visiting oculoplasty clinic from January to December 2022
|
Variables |
|
Frequency |
Percent |
|
Eye trauma |
Yes |
38 |
15.2 |
|
No |
212 |
84.8 |
|
|
Eye surgery |
Yes |
12 |
4.8 |
|
No |
238 |
95.2 |
|
|
Investigation |
CT |
11 |
4.4 |
|
MRI |
12 |
4.8 |
|
|
Histology |
11 |
4.4 |
However, when focusing on children under the age of 15, CNLDO emerged as the most prevalent condition, constituting 19.14% of cases. Following CNLDO, ptosis was the second most common presentation at 14.89%. Dermoid cyst and capillary hemangioma were equally observed, each accounting for 6.38% of cases.
Figure 1: common diagnosis of participants visiting oculoplasty clinic from January to December 2022
When observing the various disease types within their respective categories, it is evident that lacrimal disorder (43.6%) holds the highest prevalence, succeeded by orbital disorder (25.6%) and eyelid disorder (21.6%). The least prevalent category is the combination of the aforementioned disease types (9.2%).
Figure 2: category of disease of participants visiting oculoplasty clinic from January to December 2022
Discussion
Our study focused on Oculoplasty clinic visits and found that lacrimal disorders were the most frequent (43.6%), followed by orbital disorders (25.6%), then eyelid disorders (21.6%), and a smaller portion had a combination of disorders (9.2%). This contrasts with a study conducted in Port Harcourt, Nigeria, where eyelid disorders were followed by orbital and lacrimal disorders (11). A study from Glasgow, Scotland, showed eyelid disorders as the most common (56.5%), followed by lacrimal (19.5%), and orbital disorders (5.4%) (2). Another study in Singapore indicated that eyelid disorders were predominant (60.3%), followed by orbital and lacrimal disorders (5) – a different pattern from our findings. The variation in results may be attributed to factors such as the availability of professionals and infrastructure for lacrimal surgeries at secondary eye units, anatomical differences, trachoma prevalence, environmental influences, methodological variations, and genetic diversity within societies.
Within our study, the most prevalent oculoplasty disorders were NLDO (Nasolacrimal Duct Obstruction) at 17.6%, followed by blepharoptosis at 7.6%, CDC (Chronic dacryocystitis) and anophthalmic socket conditions at 5.2% each. When examining the prevalence of diseases within each category, we found that blepharoptosis was the most common eyelid disorder (31.48%), NLDO led among lacrimal disorders (40.36%), and anophthalmic socket issues were the most frequent orbital condition (20.31%). In contrast, the Port Harcourt Nigerian study reported chalazion as the most common eyelid disorder, with TED (Thyroid Eye Disease) and NLDO as the predominant orbital and lacrimal disorders, respectively (11). These differences might be attributed to disparities in study methodologies, environmental factors, racial demographics, and genetic characteristics of the studied populations.
Comparative research supports NLDO as a common etiology, as seen in a Canadian study (3) and the L.V. Prasad Eye Institute's study in India (6). Additionally, Singapore's study found ptosis to be the most prevalent overall eyelid disorder (5), which aligns with our results showing ptosis as the most common eyelid issue (31.48%). However, studies from Sao Paulo, Brazil, reported trichiasis and blepharoptosis as the most prevalent eyelid conditions (4), differing from our findings, possibly due to variations in study methodologies. In contrast, a study from MKCG Medical College, India, indicated that lid disorders constituted only 4% of cases, with chalazion being the primary disorder (7), likely influenced by differences in the study population, methodology, and environmental factors.
A research conducted at Lady Reading Hospital, Pakistan, discovered a significant male predominance (57.8%) in cases of orbital disorder, whereas our study showed a female predominance (55.5%). The age range most affected in the Pakistan study was between 28.89 +/- 22.02 years, which is comparable to our findings, where the majority of patients (38.6%) fell between 31-60 years of age. However, the most common disorders differed; in the Pakistan study, bacterial infection (35.6%) and thyroid orbitopathy (31.1%) were prevalent, while in our study, anophthalmic socket (20.31%) and dermoid cyst (15.62%) were the top conditions. These differences could be attributed to environmental factors, racial disparities, and genetic variations.
In Benin Republic, the study on orbital disorders demonstrated a male predominance of 60.8%, contrary to our findings. Additionally, the most affected age group in Benin was children, while in our study; it was adults between 31-60 years old. The primary diseases observed in Benin were orbital tumors (43.6%) and trauma (30.8%), while in our research, anophthalmic socket and dermoid cyst were more prevalent. These variations might be influenced by differences in environmental factors and study methodologies.
According to our study, Oculoplasty disorders are more common in females, accounting for 53.6% of cases. This finding is consistent with previous studies conducted in Nigeria, which reported female predominance of 52.4% and a female to male ratio of 3:2 in Port Harcourt (9, 11). The age group most frequently seeking Oculoplasty services in our study was 31-60 years old, making up 38.4% of cases. In contrast, the Nigerian study reported a higher proportion of individuals in the 21-30 years age range seeking Oculoplasty services (11). This difference in age distribution may be attributed to variations in awareness, availability of the services in the society.
We found that the majority of our patients (56.4%) reside in urban areas, with a significant percentage working for the government (37.2%). Similarly, the L.V. Prasad eye institute study in India indicated a higher prevalence of Oculoplastics diseases in urban, middle to high income families, and patients older than 30 years (6). However, it's important to note that the Indian study specifically focused on patients with lacrimal diseases.
Regarding eyelid disorders, they accounted for 21.6% of new cases in our Oculoplastics clinic. This prevalence was higher compared to the study conducted in Ekiti Nigeria, which reported 8.3% of eyelid disorders (12). In our study, the most common eyelid pathologies were ptosis (38.88%) followed by ectropion (13%). Conversely, the Ekiti Nigerian study identified infective/inflammatory lesions (50.8%) and trauma (17.7%) as the top eyelid disorders (12). These discrepancies can be attributed to differences in study methodologies and environmental factors within the respective population
Conclusion
In conclusion, our study reveals that lacrimal diseases are the most common conditions observed in the oculoplasty clinic, with NLDO being prevalent among adults and CNLDO among pediatric patients. The findings indicate a slight female predominance and a concerning trend of late patient presentation; we found that ptosis, NLDO and anophthalmic socket were the leading disease entities from eyelid, lacrimal and orbital disorders respectively.
This thesis sheds light about the profile of oculoplasty patient populations but it has its own limitations. The small sample size and the research being hospital based and single center are the two notable limitations.
Recommendation
Based on these results, we suggest the ministry of health to invest on trainning more professionals and establish the necessary infrastructure to ensure timely and optimal care for our patients.
The SPHMMC should utilizing mass media and other available platforms to educate people about ocular health and the importance of seeking early medical attention.
We suggest the scholars in the field of ophthalmology or oculoplasty to do a community based research to know the disease prevalence and the knowledge, attitude and practice of individuals both at the primary health care and at the community level.
By implementing these recommendations, we can improve the overall management of oculoplasty disorders and enhance the well-being of patients in our community.
Acknowledgmnt
The development of this thesis became a reality through the unwavering collaborative endeavors of numerous individuals, without their contributions it would not have been achievable. Hence, in this segment, I wish to extend my gratitude to those who directly or indirectly played a role in making this thesis come to fruition. Foremost, I want to convey my sincere and profound appreciation to my advisors: Dr. Asrat Sime, Dr. Seblewongel Eshetu, and Mr. Tariku Shimelis, for their wholehearted guidance and valuable insights, spanning from the initial title selection phase to the actual development of the thesis.
I am also indebted to Saint Paul’s Hospital Millennium Medical College, Department of Ophthalmology, for affording me the invaluable opportunity and exposure, as well as for their unceasing administrative support. Lastly, I would like to express my gratitude to my friends for their encouragement; the residents who actively participated in the data collection process; patients who participated in the study and my instructors who imparted essential knowledge about the fundamentals of research methodology. Without their contributions, I would not have been able to formulate this thesis.
References
1. Plastic O, Surgery O. No Title.
2. El-sheikh BYM, Chadha V. Profile of a tertiary referral oculoplastics service in the UK.
3. Mainville N, Jordan DR. Etiology of tearing: A retrospective analysis of referrals to a tertiary care oculoplastics practice. Ophthal Plast Reconstr Surg. 2011;27(3):155–7.
4. Wanzeler ACV, do Nascimento MF, Sousa RLF, Padovani CR, Schellini SA. Eyelid disorders: Frequency of occurrence and profile of carriers in a Brazilian population sample. Rev Bras Oftalmol. 2015;74(4):231–4.
5. Jin Tan MC, Young S, Amrith S, Sundar G. Epidemiology of oculoplastic conditions: The singapore experience. Orbit. 2012;31(2):107–13.
6. Das AV, Rath S, Naik MN, Ali MJ. The Incidence of Lacrimal Drainage Disorders Across a Tertiary Eye Care Network: Customization of an Indigenously Developed Electronic Medical Record System-EyeSmart. Ophthal Plast Reconstr Surg. 2019;35(4):354–6.
7. Bhoi R, Panda S, Panda J, Bnr P. Pattern of Ocular Diseases in Patients Attending To A Tertiary Eye Care Center In Southern Odisha. 2018;17(9):1–3.
8. Idris M, Yaqoob H, Khan MA, Zar A, Ullah S. Pattern of Orbital Diseases at a Tertiary Oculoplastic Center. Pakistan J Ophthalmol. 2020;37(1):70–4.
9. Balogun BG, Adekoya BJ, Balogun MM, Ehikhamen OA. Original Article Orbito–Oculoplastic Diseases in Lagos: A 4?Year Prospective Study. 2014;21(3).
10. CRA A, AB A, S M, E K, I S, Hounnou S T, et al. Epidemiological, Clinical and Therapeutic Aspects of Orbital Diseases in Ophthalmologic Hospital of Saint André de Tinré (OHSAT), in Benin Republic. J Med Surg Pathol. 2016;01(04):3–7.
11. Ejimadu CS, Chinawa NE, Theophilus B. Demographic Distribution of Oculoplastic Disorders in Port Harcourt Nigeria. Ophthalmol Res An Int J. 2019;11(2):1–5.
12. Omotoye O, Ajayi I, Ajite K, Adeleke F. Pattern of Eyelid Disorders in a Tertiary Health Centre, South Western, Nigeria. J Heal Sci Res. 2018;3(2):1–5.
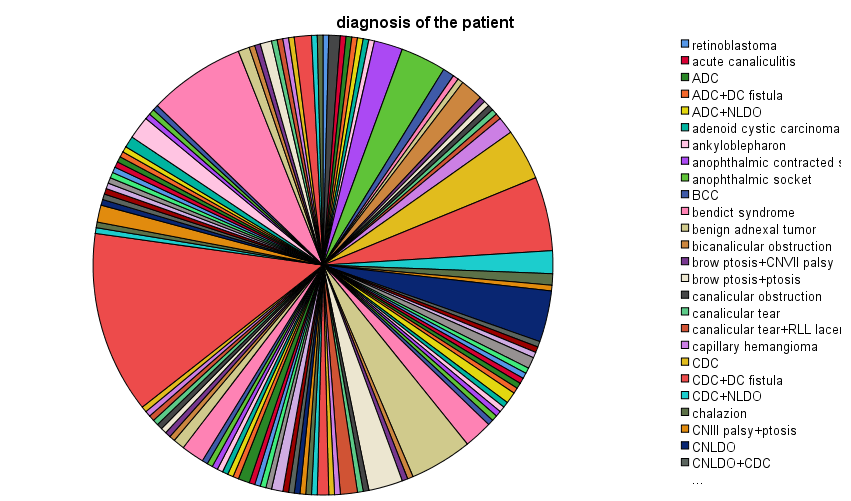
Figure 1
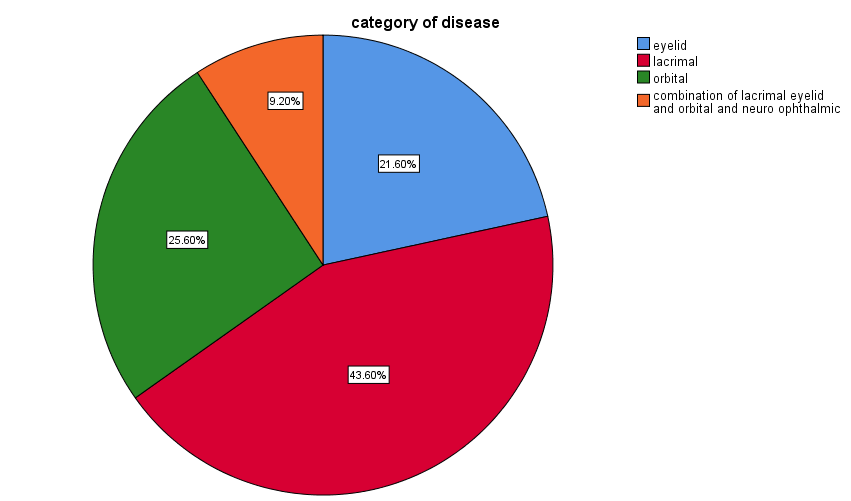
Figure 2
