An Overview of Total Hip Arthroplasty Surgery
An Overview of Total Hip Arthroplasty Surgery
Pratham Surya*
*Correspondence to: Pratham Surya, Consultant Orthopaedic Surgeon.
Copyright
© 2024 Pratham Surya. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 12 Sep 2024
Published: 01 Oct 2024
Abstract
Total Hip Arthroplasty (THA) is a reliable surgical intervention that improves patients' quality of life by increasing mobility, range of motion, and reducing pain in degenerative hip joints. It is effective for treating chronic conditions affecting the hip joint. However, selecting the right approach for THA is crucial in pre-operative planning, as each approach has its own challenges, success rates, and limitations. To understand the advantages and disadvantages of different surgical approaches and the causes of THA procedure failure, a critical review of each approach is recommended.
Keywords: Anterolateral approach, Direct anterior approach, Direct lateral approach, Periprosthetic joint infection, Posterior approach, THA dislocation, Total hip arthroplasty.
An Overview of Total Hip Arthroplasty Surgery
Introduction
Total hip arthroplasty (THA) is a surgical procedure that reduces pain and improves quality of life in patients with hip osteoarthritis. With over one million THAs performed annually, it is projected to reach two million by 2030. There are three surgical approaches: Direct Anterior Approach (DAA), Posterior Approach (PA), and Lateral Approach (LA). PA involves splitting the gluteus maximus muscle to expose the femur and acetabulum, avoiding disruption of hip abductors. However, PA has an increased dislocation rate. LA, on the other hand, has the lowest risk of dislocation but is associated with superior gluteal nerve injury, impaired abductor function, and heterotopic ossification. DAA offers earlier recovery, lower dislocation rates, and shorter hospital stays, but has disadvantages such as increased risk of periprosthetic fractures, an increased learning curve, and higher risk of injuring the Lateral Femoral Cutaneous Nerve. This article provides a critical review of outcomes and complications for each surgical approach.
Fig 1: Surgical approaches to Total Hip Arthroplasty.
Approaches in Total Hip Arthroplasty
The Direct Anterior Approach (DAA) is a soft tissue sparing surgical approach that enters the hip through an intermuscular plane between the tensor fasciae latae and gluteus medius laterally and medially through the sartorius muscle and rectus fascia. This approach is considered potentially advantageous when compared to other surgical approaches, as it preserves the stability of the hip joint. Patients have been documented to experience a rapid recovery based on function and activity using the DAA, making it potentially advantageous when compared with other approaches.
Postoperative narcotic use is considerably lower in DDA compared to other surgical approaches. The length of stay has been found to be shorter and more patients are being discharged home as opposed to transfer to post-op care facilities. Motor function recovery is faster and the time for ambulation without the use of assisted devices is also shorter. The average time to discontinue the use of walkers or canes was 21 days.
The DAA spares abductor muscles and the accuracy of the acetabular cup positioning has been shown to be better with less variation in cup angle when compared to the posterior approach. Although there is a tendency for the insertion of the acetabular cup in an anteverted fashion, revision rates for acetabular cup failure were lower in DAA compared to the posterior approach. Nerve injuries are also a risk with DAA, with the LFCN being among the most injured nerve with the DAA.
The most important predisposing factor for LFCN injury is the branching pattern. A study described four major branching patterns identified as trifurcate, primary femoral, late, and classical. The late branch was found to be at highest risk for injury due to its perpendicular orientation to the incision line. The best way to avoid nerve damage is to be cognizant of the various anatomical variations. The rate of injury of the LFCN associated with the DAA is variable between studies with reports ranging from 0.1% to 81%.
Early rates of THA failure have been reportedly increasing ranging from 24% to 50% within 5 years of the surgery due to femoral or acetabular prosthetic fracture, mal-alignment, or instability. Malalignment of the acetabular cup causes impingement, dislocation, and loosening of the acetabular component. Femoral stem alignment and acetabular anteversion may differ among approaches but has been shown to be more difficult to implant the femoral stem in a neutral position through the anterolateral approach.
The Posterior Approach (PA) is the most used surgical approach for THA, performed by positioning the patient in lateral decubitus position. Studies have shown that PA has been associated with greater dislocation rates than the LA, with studies showing a occurrence of almost 10% dislocation rate after THA using PA compared to the anterolateral approach.
Fig 2: Potential causes of failure and complications following Total Hip Replacement.
The lateral approach to total hip replacement (THA) has evolved over the years, with various modifications made over the decades. The most well-known LA was described by Hardinge and involved splitting the gluteus medius and minimus tendons longitudinally and continuing distally into the vastus lateralis tendon. The anterolateral approach gained popularity and was well developed by Sir Watson-Jones, which involved the interval between the tensor fasciae latae and the gluteus medius tendon. The Rottinger approach modified the LA by sparing detaching the abductor before exposing the joint capsule.
The minimally invasion approach has also been used with early recovery in outpatient total hip programs, with up to 99% of patients successfully discharged on the day of the THA using this approach. A randomized controlled trial compared 40 patients undergoing LA with patients using the DAA, finding that the DAA had better initial functional recovery up to 2 weeks post-operative. However, no difference was seen with respect to operative blood loss, procedure time, or length of stay in the hospital.
Post-surgical complications remain an issue for many patients, and advances in implant design, advanced protocols for controlling infections, and minimally invasive procedures have improved outcomes of THA. However, possible causes of THA failure include periprosthetic joint infection, dislocation, iliopsoas impingement, and implant malalignment. Dislocation is one of the most common issues after a primary THA, with risk factors such as obesity, spinal fusion, and capsular repair playing a critical role in dislocation.
Periprosthetic Joint Infection (PJI) can occur any time after the operation and is the most troublesome cause of failure after a hip replacement. Risk factors for PJI include high body mass index, surgical site infection, diabetes mellitus, chronic pulmonary disease, cardiovascular disease, and allogenic blood transfusion. Preoperative screening for risk factors is critical to reduce the incidence of infection in THA. Perioperative antibiotic prophylaxis has also been researched to prevent PJI, with data supporting the use of cephalosporins. Debridement and antibiotics for PJI in well-fixed implants is the first option for treatment. Critical factors for the success of this option involve early intervention, typically within seven days of onset, and replacing all modular components.
Nerve impingement is a severe post-op complication after THA, causing pain upon active hip flexion and resulting in nerve palsy. Risk factors for nerve damage include revision arthroplasty, female sex, dysplastic osteoarthritis, and limb elongation. Recovery of femoral nerve palsy has been shown to be more predictable than sciatic nerve injury.
Conclusion
Total hip arthroplasty involves various surgical approaches like DAA, LA, and PA, each with its own advantages and disadvantages. PA is the most common, but other methods struggle with infection rates, bone loss, and accessibility, making surgeons cautious when choosing a surgical approach.
References
1. Ackerman IN, Bohensky MA, Zomer E, et al. The projected burden of primary total knee and hip replacement for osteoarthritis in Australia to the year 2030. BMC Musculoskelet Disord 20 (2019): 90. [PMC free article] [PubMed] [Google Scholar]
2. Shan L, Shan B, Graham D, et al. Total hip replacement: a systematic review and meta-analysis on mid-term quality of life. Osteoarthritis Cartilage 22 (2014): 389–406. [PubMed] [Google Scholar]
3. Talia AJ, Coetzee C, Tirosh O, et al. Comparison of outcome measures and complication rates following three different approaches for primary total hip arthroplasty: a pragmatic randomised controlled trial. Trials 19 (2018): 13. [PMC free article] [PubMed] [Google Scholar]
4. Docter S, Philpott HT, Godkin L, et al. Comparison of intra and post-operative complication rates among surgical approaches in Total Hip Arthroplasty: A systematic review and meta-analysis. J Orthop 20 (2020): 310–325. [PMC free article] [PubMed] [Google Scholar]
5. Hartford JM, Bellino MJ. The Learning Curve for the Direct Anterior Approach for Total Hip Arthroplasty: A Single Surgeon’s First 500 Cases. HIP International 27 (2017): 483–488. [PubMed] [Google Scholar]
6. Su EP. Retraction: Post-operative neuropathy after total hip arthroplasty. Bone Joint J 99 (2017): 46–49. [PubMed] [Google Scholar]
7. Jia F, Guo B, Xu F, et al. A comparison of clinical, radiographic, and surgical outcomes of total hip arthroplasty between direct anterior and posterior approaches: a systematic review and meta-analysis. HIP International 29 (2019): 584–596. [PubMed] [Google Scholar]
8. Nistor DV, Caterev S, Bolboac? SD, et al. Transitioning to the direct anterior approach in total hip arthroplasty. Is it a true muscle sparing approach when performed by a low volume hip replacement surgeon? Int Orthop 41 (2017): 2245–2252. [PubMed] [Google Scholar]
9. Nistor DV, Bota NC, Caterev S, et al. Are physical therapy pain levels affected by surgical approach in total hip arthroplasty? A randomized controlled trial. Orthop Rev (Pavia) 12 (2020). [PMC free article] [PubMed] [Google Scholar]
10. Rodriguez JA, Deshmukh AJ, Rathod PA, et al. Does the direct anterior approach in THA offer faster rehabilitation and comparable safety to the posterior approach? Clin Orthop Relat Res 472 (2014): 455–463. [PMC free article] [PubMed] [Google Scholar]
11. Meermans G, Konan S, Das R, et al. The direct anterior approach in total hip arthroplasty. Bone Joint J 99-B (2017): 732–740. [PubMed] [Google Scholar]
12. Moerenhout K, Derome P, Laflamme GY, et al. Direct anterior versus posterior approach for total hip arthroplasty: a multicentre, prospective, randomized clinical trial. Canadian Journal of Surgery 63 (2020): E412–417. [PMC free article] [PubMed] [Google Scholar]
13. Bhaskar D, Rajpura A, Board T. Current Concepts in Acetabular Positioning in Total Hip Arthroplasty. Indian J Orthop 51 (2017): 386–396. [PMC free article] [PubMed] [Google Scholar]
14. Bartlett JD, Lawrence JE, Khanduja V. What Is the Risk Posed to the Lateral Femoral Cutaneous Nerve During the Use of the Anterior Portal of Supine Hip Arthroscopy and the Minimally Invasive Anterior Approach for Total Hip Arthroplasty? Arthroscopy: The Journal of Arthroscopic and Related Surgery 34 (2018): 1833–1840. [PubMed] [Google Scholar]
15. Coffey R, Gupta V. Meralgia Paresthetica. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023(2022). [PubMed] [Google Scholar]
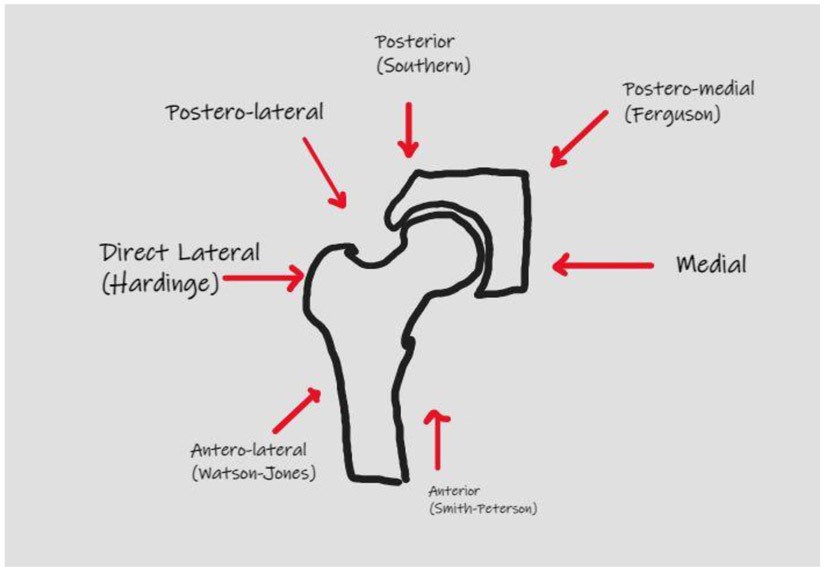
Figure 1
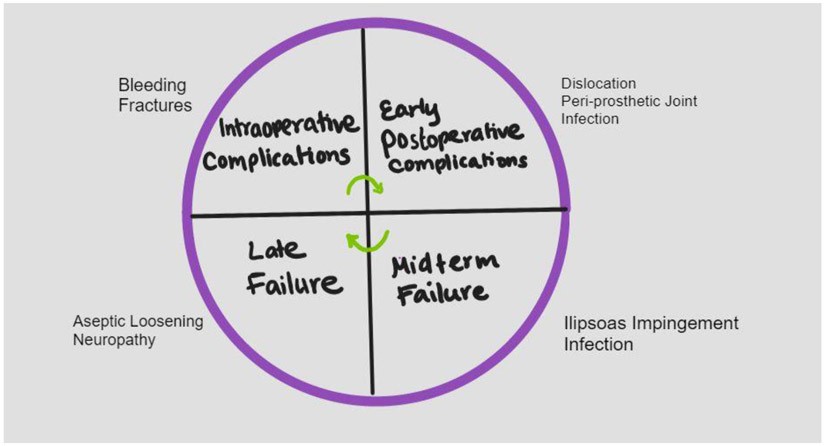
Figure 2
