Outcome of Burnout among Caregivers of Dementia Patients in AlHassa
Outcome of Burnout among Caregivers of Dementia Patients in AlHassa
Dr. Qasem Aljabr *, Khadijah Taher Alkathim, Laila Abdulhadi Alsalman, Bilqis Mohammed Buoways
*Correspondence to Dr. Qasem Aljabr, Saudi Arabia.
Copyright
© 2024 Dr. Qasem Aljabr. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 16 September 2024
Published: 01 October 2024
DOI: https://doi.org/10.5281/zenodo.13859991
Abstract
Background: Dementia affects the elderly by impairing memory, orientation, and decision-making. Caregivers, often family members, experience significant stress and burnout due to the intensive care required. While there is substantial literature on occupational burnout, limited studies focus on the stress faced by dementia caregivers in Saudi Arabia and the MENA region. This study aims to quantify caregiver burden and its impact on the quality of care for dementia patients in AlHassa, Saudi Arabia.
Methods: An observational cross-sectional study was conducted from January to June 2024 in AlHassa, Saudi Arabia. Convenience sampling targeted caregivers of dementia patients from Ministry of Health outpatient clinics. Data collection involved a validated questionnaire, including the revised Zarit Caregiver Burden Scale (ZBI-12) and patient A1C levels to assess care quality. A minimum sample size of 183 was determined based on a 50% prevalence rate. Statistical analysis was performed using SPSS version 23.0.
Results: The study included 181 participants, nearly evenly split by gender (49.7% males, 50.3% females). Most caregivers were married (80.7%), had university or secondary education (72.4%), and were primarily the patient's children (79%). Caregivers' age ranged from 18 to over 65, with 62.4% living with the patient. The mean ZBI-12 score was 15.39 (SD = 11.20), with 42.5% experiencing no to mild burden, 27.1% mild to moderate burden, and 30.4% high burden. Caregiver burden was significantly associated with living with the patient (p = 0.016) and the number of children (p = 0.002). Patients with dementia for over six years had caregivers with lower burden scores (p = 0.025). Other factors such as gender, marital status, education, and comorbidity showed no significant effects.
Conclusion: Caregiver burden in dementia patients in AlHassa is significant, with nearly a third experiencing high levels of stress. Key factors influencing burden include residence with the patient and childcare responsibilities, while longer disease duration is associated with lower caregiver burden, potentially due to adaptation over time. These findings highlight the need for targeted support interventions for caregivers to improve both their well-being and the quality of care for dementia patients.
Keywords: Caregiver Burden, dementia, Burnout, Saudi Arabia, Quality of Care
Outcome of Burnout among Caregivers of Dementia Patients in AlHassa
Introduction
Dementia is a neurodegenerative disease that disproportionately affects the elderly and causes impairment in areas such as memory, orientation, and decision-making [1-2]. Although there are other potential causes of dementia, Alzheimer's dementia is by far the most common. Factors such as age, genetics, sexual orientation, gender, cognitive reserve, ethnicity, health status, and way of life all have a part [1-2]. Occupational burnout is the primary subject of the literature. However, studies examining the stress that dementia carers in Saudi Arabia and other MENA nations face are few and far between [3].
Dementia severely limits patients' ability to care for themselves, necessitating a greater level of caregiver participation [4]. Caregivers' health and well-being, as well as the care of demented patients, are greatly improved when the burden of caring for these patients is reduced. This, in turn, aids in the early detection of health conditions, the clinical response, and the subsequent decisions about treatment [5-6]. Makes it possible to intervene before burnout even starts to set in, giving therapy a better chance of success.
Half a billion people throughout the world suffer from dementia, and the cost to treat it is at least one trillion dollars a year. There was a 144.95% increase in the number of dementia patients identified between 1990 and 2019. From 1990 to 2016, dementia jumped 12 spots to become the sixth most burdensome illness or injury in the US, based on the most current Global Burden of Disease categorization system [6-9]. Over 11 million Americans provide unpaid assistance to those suffering from dementia. The majority of those taking care of their parents are women, and over half of them are either married or in committed relationships. Dementia caregivers report much higher rates of emotional, financial, and physical difficulties compared to non-dementia caregivers. Caregivers of people with dementia report devoting 27 more hours per month (92 vs 65 hours) to care than caregivers of people without dementia [2].
Given the significant role that caregivers play in the care of older patients, particularly those with dementia, and the immense burden that this condition imposes, this research aimed to quantify the prevalence of caregiver burden and its impact on the quality of care for dementia patients [10]. Considering the dearth of research on this particular aspect on a global scale. Furthermore, no prior research has used a validated, standardized instrument to assess the burden on Saudi Arabian caregivers due to dementia. Another important part of dementia prevention efforts is giving care the information and resources they need, which include emotional, social, psychological, and technical resources [2, 11-12]. The purpose of this research was to examine the frequency of caregiver burden and how it affects the standard of care for people with dementia.
Methods
Research Design
An observational cross-sectional study design was employed to measure the prevalence of caregiver burden and its effects on the quality of care for dementia patients in Alhassa, located in the Eastern Province of the Kingdom of Saudi Arabia. The study was conducted from January to June 2024. Ethical approval was obtained from the Institutional Review Board (IRB) of King Fahad Hospital – Hofuf (KFHH), Saudi Arabia. Data was collected via a questionnaire administered to caregivers of dementia patients through virtual or outpatient clinics. Participants were fully informed about the study's aims, and informed consent was required before completing the questionnaire. Confidentiality of the information provided was ensured.
Sampling
Convenience sampling was used for this study. The target population included patients diagnosed with dementia disease and their caregivers from Ministry of Health outpatient clinics. Participants were interviewed either virtually or in outpatient clinics following official appointment registration. Informed consent was obtained from both patients (if eligible) and their caregivers. The inclusion criteria encompassed elderly male and female patients aged 65 and above diagnosed with dementia, with or without other chronic diseases, as well as adult caregivers aged 18 and above who lived with the patients and assisted with daily activities or medical care. Healthcare workers were excluded from this study [13].
Using the formula n=Zα/22⋅p⋅(1−p)e2n=e2Zα/22⋅p⋅(1−p) for calculating the adequate sample size in prevalence studies, a minimum sample size of 183 participants was determined, assuming a 50% prevalence rate, an absolute precision of 0.05, and a 95% confidence level [14-19]. There wer e 10 participants that were excluded after contacting caregivers as they passed away.
Questionnaire
Data was collected using a validated, standardized research tool. A personal questionnaire was used to gather socio-demographic data related to both the caregiver and the dementia patient. The primary tool, the revised Zarit Caregiver Burden Scale, was used to assess caregiver burden. This scale, which has been validated in various culturally and ethnically diverse populations, provides a comprehensive assessment of both objective and subjective burdens. The short version of the scale, containing 12 items, was utilized. Each item was rated on a 5-point scale, with responses ranging from 0 (Never) to 4 (Nearly Always). The scores ranged from 0 to 48, with higher scores indicating greater caregiver burden. The scores were categorized into four groups: 0-10 (no to mild burden), 10-20 (mild to moderate burden), and >20 (high burden).
Measurement of Quality of Care
The effect of caregiver burden on the quality of care for dementia patients was measured using the patient's A1C reading. A cutoff of 9 was used; an A1C reading above 9 indicated poor quality of care. The quality of care was reflected by measuring the effect of burnout on A1C and blood pressure measurements.
Statistical Analysis
All statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) version 23.0. Descriptive statistics were presented using the arithmetic mean and standard deviation. Spearman's rank correlation test and Pearson's chi-squared test were employed for inferential statistics. Confidence intervals (CIs) of 95% were used, and a P-value of < 0.05 (two-sided) was considered statistically significant.
Results
The study included 181 patients after after contacting 190 caregivers' and exclusion of 10 patients who passed away based on caregivers’ contact. The demographic characteristics of the surveyed population are diverse across multiple variables. Gender distribution is nearly even, with 90 males (49.7%) and 91 females (50.3%). In terms of marital status, the majority of respondents are married (146 individuals, 80.7%), with 27 single (14.9%) and 8 divorced (4.4%). Education levels vary, with 69 participants having university education (38.1%), 62 with secondary education (34.3%), 22 with intermediate education (12.2%), and 28 with primary education (15.5%). Regarding kinship degree, most respondents (143 individuals, 79%) are children, while 14 (7.7%) are spouses, and 24 (13.3%) fall into other categories. Age distribution shows that 98 participants (54.1%) are aged 46-65, 77 (42.5%) are between 18-45, and a small portion (6 individuals, 3.3%) are over 65. Residence data reveals that 113 respondents (62.4%) live with the patient, while 68 (37.6%) live separately. In terms of childcare responsibilities, 90 participants (49.7%) have three or more children, 39 (21.5%) have one or two children, and 52 (28.7%) have no children. The time spent per day on activities varies, with 31 participants (17.1%) indicating they spend all day, and other responses scattered across different time intervals. Table 1 summarizes the demographic characteristics of study participants.
|
Table 1: Demographic characteristics of study participants |
|||
|
Characteristic |
Categories |
Frequency |
Percent |
|
Gender |
Male |
90 |
49.7 |
|
Female |
91 |
50.3 |
|
|
Marital Status |
Single |
27 |
14.9 |
|
Married |
146 |
80.7 |
|
|
Divorced |
8 |
4.4 |
|
|
Education |
Primary |
28 |
15.5 |
|
Intermediate |
22 |
12.2 |
|
|
Secondary |
62 |
34.3 |
|
|
University |
69 |
38.1 |
|
|
Kinship Degree |
Spouse |
14 |
7.7 |
|
Child |
143 |
79.0 |
|
|
Other |
24 |
13.3 |
|
|
Age |
18-45 |
77 |
42.5 |
|
46-65 |
98 |
54.1 |
|
|
More than 65 |
6 |
3.3 |
|
|
Residence |
With patient |
113 |
62.4 |
|
Separately |
68 |
37.6 |
|
|
Child Care |
No |
52 |
28.7 |
|
1-2 |
39 |
21.5 |
|
|
3 and more |
90 |
49.7 |
|
The demographic characteristics of patients with dementia disease reveal several notable trends. In terms of age, the largest group of patients (96 individuals, 53.0%) are over 80 years old, followed by those aged 71-75 (34 individuals, 18.8%), 76-80 (30 individuals, 16.6%), and 65-70 (21 individuals, 11.6%). Gender distribution indicates a higher proportion of female patients, with 100 females (55.2%) compared to 81 males (44.8%). The duration of AD varies, with half of the patients (92 individuals, 50.8%) having had the disease for 0-3 years, 60 patients (33.1%) for 4-6 years, and 29 patients (16.0%) for more than 6 years. The majority of patients (156 individuals, 86.2%) have comorbidities, while only 25 patients (13.8%) do not have any additional health conditions. Table 2 presents demographic characteristics of dementia Disease. Detailed participants responses are presented in annex 1.
|
Table 2: Patients’ demographic characteristics |
|||
|
Characteristic |
Categories |
Frequency |
Percent |
|
Patient Age |
65-70 |
21 |
11.6 |
|
71-75 |
34 |
18.8 |
|
|
76-80 |
30 |
16.6 |
|
|
More than 80 |
96 |
53.0 |
|
|
Patient Gender |
Male |
81 |
44.8 |
|
Female |
100 |
55.2 |
|
|
AD Duration |
0-3 |
92 |
50.8 |
|
4-6 |
60 |
33.1 |
|
|
More than 6 |
29 |
16.0 |
|
|
Comorbidity |
No |
25 |
13.8 |
|
Yes |
156 |
86.2 |
|
The demographic characteristics reveal significant data regarding the population studied, specifically focusing on diabetes mellitus (DM), HbA1c levels (A1C), hypertension (HTN), and blood pressure (BP). Among the participants, 55.6% (100 individuals) have diabetes mellitus, while 44.4% (80 individuals) do not. The HbA1c levels, an indicator of blood sugar control over the past three months, show that 56.2% (118 individuals) have levels from less than 8% which indicates a controlled state of DM. However, 3.2% (42 individuals) have levels between 8-9%, and 3.9% (7 individuals) have levels higher than 10%, with only 0.6% (1 individual) having levels between 9-10%. Hypertension is prevalent among the participants, with 75.8% (135 individuals) diagnosed with HTN, while 24.2% (43 individuals) do not have hypertension. Blood pressure readings show that 97 participants had a blood pressure of less than 140/90 (53.6%). Notably, 19.3% (35 individuals) have BP levels higher than 140/90, and 1.7% (3 individuals) have extremely high BP levels over 180/120. Only 11.0% (20 individuals) maintain optimal BP levels of 120/80 or less. These characteristics provide a comprehensive overview of the health status of the population, highlighting significant areas of concern regarding chronic diseases and their management.
Participants had varying levels of burden, as assessed by the short form ZBI-12 (Zarit Burden Interview). The majority of respondents (77 individuals, 42.5%) fall into the 'No to Mild' burden category, scoring between 0-10. The 'Mild to Moderate' burden category, with scores ranging from 10-20, includes 49 individuals (27.1%). Finally, a significant portion (55 individuals, 30.4%) experience a 'High' burden, indicated by scores greater than 20 (Figure 1). The mean score value of ZBI-12 was 15.39 + 11.20 with median score of 14. Score ranged from zero to 45.
Figure 1: Burden severity among dementia patients
The analysis of the demographic characteristics reveals significant insights into the population under study. For the Patient Gender, both males (N=81) and females (N=100) have similar mean scale scores, with males scoring 14.89 and females 15.80. The t-test indicates no significant difference between genders (t=-0.543, p=0.588). Regarding comorbidity, individuals without comorbidity (N=25) have a lower mean scale scores of 11.60 compared to those with comorbidity (N=156), who have a mean score of 16.00. This difference approaches significance (t=-1.835, p=0.068), suggesting that comorbidity might impact the burden scale scores. For Patient Age, the mean scale scores vary slightly across different age groups, with ANOVA indicating no significant differences (F=0.805, p=0.782). Similarly, for dementia disease duration, the mean scale scores across different duration groups do not differ significantly (F=1.182, p=0.239). These findings provide a comprehensive understanding of how these demographic factors relate to the scale scores in this population. There was strong significant linear correlation between level of HbA1C and ZBI-12 score, in which increased level of HbA1C was correlated with increases ZBI-12 score (r= 0.758, P=0.005). This indicates that patients with higher HbA1C had high burden.
|
Table 3: Mean scores of ZBI-12 based on patients characteristics |
||||
|
Characteristic |
Category |
Mean |
t/F value |
P value |
|
Patient Gender |
Male |
14.89 |
-0.543 |
0.588 |
|
Female |
15.80 |
|||
|
Comorbidity |
No |
11.60 |
-1.835 |
0.068 |
|
Yes |
16.00 |
|||
|
Patient Age |
65-70 |
15 |
0.805 |
0.782 |
|
71-75 |
15 |
|||
|
76-80 |
15 |
|||
|
More than 80 |
16 |
|||
|
Dementia Duration |
0-3 |
14 |
1.182 |
0.239 |
|
4-6 |
16 |
|||
|
More than 6 |
20 |
|||
|
HbA1C |
Less than 8% |
12 |
1.041 |
0.115 |
|
8-9% |
15 |
|||
|
9-10% |
15 |
|||
|
More than 10% |
16 |
|||
The regression analysis highlights the significant predictors among the demographic and patient-related variables. The model fitting criteria show a Chi-Square value of 57.680 with a significance level of 0.035, indicating the overall model is statistically significant. Pseudo R-square values of Cox and Snell (0.273), Nagelkerke (0.309), and McFadden (0.148) suggest a moderate fit of the model to the data. Significant predictors include Residence (p=0.014) and Child Care (p=0.002), with specific categories within these variables showing strong associations with the dependent variable. For instance, residing with the patient increases the likelihood (Exp(B)=3.426, p=0.016) of falling into higher scale categories. Similarly, having 1-2 children is significantly associated with higher scales, but the presence of 3 or more children decreases this likelihood significantly (Exp(B)=0.135, p=0.003). The presence of dementia disease duration over 6 years also shows a significant negative association (Exp(B)=0.259, p=0.025) with higher scales. Other variables such as gender, marital status, education, age, and comorbidity did not show significant effects on the dependent variable. Table 4 presents the results of regression analysis.
|
Table 4: Regression Analysis |
||||||
|
Variable |
Category |
B |
Std. Error |
Sig. |
Exp(B) |
95% Confidence Interval for Exp(B) |
|
Residence |
With patient |
1.232 |
0.512 |
0.016 |
3.426 |
1.255 – 9.353 |
|
Child Care |
1-2 |
1.099 |
0.664 |
0.098 |
3.000 |
0.816 – 11.031 |
|
3 and more |
-2.004 |
0.675 |
0.003 |
0.135 |
0.036 – 0.506 |
|
|
AD Duration |
More than 6 years |
-1.351 |
0.602 |
0.025 |
0.259 |
0.080 – 0.843 |
|
Gender |
Male |
-0.280 |
0.493 |
0.570 |
0.756 |
0.288 – 1.985 |
|
Marital Status |
Single |
-2.353 |
1.417 |
0.097 |
0.095 |
0.006 – 1.526 |
|
Education |
Primary |
0.057 |
0.783 |
0.942 |
1.059 |
0.228 – 4.917 |
|
Kinship Degree |
spouse |
2.183 |
1.252 |
0.081 |
8.873 |
0.763 – 103.239 |
|
Age |
18-45 |
0.021 |
1.481 |
0.989 |
1.021 |
0.056 – 18.620 |
|
Patient Age |
65-70 |
0.206 |
0.708 |
0.771 |
1.229 |
0.307 – 4.920 |
|
Patient Gender |
Male |
-0.673 |
0.487 |
0.167 |
0.510 |
0.196 – 1.326 |
|
Comorbidity |
No |
-0.026 |
0.567 |
0.964 |
0.974 |
0.321 – 2.962 |
Discussion
Caregivers are fundamental to the overall healthcare system, particularly in managing dementia patients. Family members predominantly provide home care and assistance to relatives with dementia, thereby saving the healthcare system hundreds of billions of dollars [20]. Dementia remains a significant concern for public health systems, impacting not only patients but also the family members who provide informal care. This informal caregiving often leads to caregiver burnout due to the mental and physical strain experienced [21].
For caregivers of individuals with Alzheimer’s Disease (AD), primary stressors such as the patient's behavioral issues—including restlessness, emotional outbursts, and inappropriate behavior—are the most significant risk factors for caregiver burden, depression, and stress-related illnesses. The challenges faced by caregivers can vary depending on the type of dementia and the associated behavioral issues [20]. Increased caregiving efforts, without a corresponding increase in perceived rewards or motivations, exacerbate the burden on dementia caregivers. Unlike caregivers of non-demented patients, those caring for dementia patients rarely experience increased burden due to physical limitations [20, 22]. While previous literature often reports a higher burden among female caregivers due to emotional involvement and societal expectations, this study found no significant gender differences in burden, aligning with research suggesting that caregiver stress is more linked to the caregiving context rather than gender alone [20-22].
In terms of patient comorbidities, this study found that caregivers of patients with additional health conditions experienced a higher, though not statistically significant, burden. This finding supports existing literature, where comorbid conditions such as diabetes and hypertension are shown to complicate caregiving by increasing the physical and medical demands on caregivers [22]. Previous studies emphasize that managing comorbidities, alongside dementia, contributes significantly to caregiver strain, particularly in cases where health conditions worsen over time [24-25].
In our sample, 13.3% of caregivers had no prior relationship with the patient, while 79% were providing care for a parent. Consistent with prior research, the majority of caregivers were the patients' daughters, followed by spouse as the second most common caregivers [18]. Similar findings have been reported in Brazil, where daughters primarily assume the caregiving role for dementia patients [24, 25].
Caregiver stress can manifest as mental health issues, such as anxiety and depression. A study indicated that 49.80% of caregivers experienced anxiety, and 26.72% suffered from depression [26]. Numerous studies have linked caregiving for dementia patients with negative mental health outcomes [27–29]. In developed countries, anxiety rates range from 16% to 45%, while depression rates vary from 23% to 85% [30, 31]. In contrast, in developing nations, mental illness affects 40–75% of the population [32]. A study of 117 unpaid caregivers found that 23.1% were at high risk for depression, and 41.0% were likely to experience ongoing psychological distress [21].
Previous research has shown that increased burnout correlates with a poorer quality of life and more severe depressive symptoms. These findings suggest that interventions targeting depression and quality of life may be effective in reducing caregiver burnout [22]. A systematic review confirmed that burnout syndrome negatively affects caregivers' quality of life and is associated with patient depressive and anxious symptoms and abusive behavior by the caregiver [33].
Contrary to most prior research, our study found no statistically significant correlation between caregiving time and the Zarit Burden Interview (ZBI) score. Previous studies indicated that extended caregiving increases the risk of burnout in both areas [27], aligning with findings that the intensity of caregiving duties predicts caregiver burnout [28]. Over time, caregivers may find themselves cutting back on leisure time for both themselves and their loved ones. Therefore, high-quality caregiver support services are essential to maintain the quality of life for caregiving dyads by reducing the burden and providing caregivers with necessary respite. Although caregiving for a dementia patient can be physically exhausting, a comprehensive review suggested that integrative approaches could significantly alleviate caregiver strain [29]. Additionally, support from nursing and health experts in symptom management has proven effective in reducing caregiver burden.
Married caregivers exhibited the highest rate of anxiety (48.50%), a statistically significant finding (P<0.05) [26]. Moreover, anxiety prevalence was strongly correlated with a history of psychiatric illness and the use of medication for such conditions. The highest rates of anxiety were among those without a psychiatric history (73.96%) and those not taking medication (70.46%) [26]. Regarding depression, a significant association was found between the caregiver's relationship with the patient and the prevalence of depression, with the highest rate (41.22%) observed among those without a relationship to the patient. The lowest income caregivers had the highest prevalence of depression at 70.34%, with all p-values below 0.05. Recent research also identified significant links between emotional exhaustion (EE) and caregiver characteristics, with female caregivers exhibiting higher levels of emotional exhaustion than their male counterparts [26]. Caregivers who reported psychological and physical problems, such as depression, anxiety, insomnia, irritability, and fatigue, also had higher EE scores [26]. Those expressing a "desire to die" had significantly higher EE scores (p<0.05). Additionally, statistical analysis revealed that higher scores on the Beck Depression Inventory (BDI) and the Beck Anxiety Inventory (BAI) were associated with increased EE levels in caregivers [23].
Age was another key factor, with this study reporting no significant differences in caregiver burden across patient age groups. This contrasts with studies suggesting that older dementia patients, particularly those in more advanced stages, require more intensive care, potentially leading to greater caregiver burden. However, the lack of a significant relationship in this study may be due to the distribution of caregiving responsibilities across different family members or the availability of external support, which can mitigate the effects of patient age on caregiver stress. An important and novel finding was the significant association between the duration of dementia and increased burden after six years [26-30]. This supports literature that links long-term caregiving to increased physical and emotional exhaustion, as caregivers become more entrenched in their roles with fewer opportunities for respite. Similar studies have noted that caregiver burden intensifies as patients' cognitive and functional decline progresses over time, leading to higher demands on caregivers. The burden is particularly evident in the later stages of dementia, where patients require assistance with all activities of daily living. Living with the patient was also a significant predictor of higher burden in this study, a finding consistently supported by previous research. Studies have long established that caregivers living with dementia patients face greater emotional and physical stress due to the round-the-clock nature of care. In line with these findings, caregivers who reside with their patients often report less time for personal activities, social isolation, and increased depression and anxiety levels, all of which contribute to higher burden scores [30-33].
Interestingly, this study found that caregivers with three or more children experienced significantly lower levels of burden, a result not commonly reported in prior research. While some studies suggest that larger family sizes do not necessarily alleviate caregiving stress, this finding could imply that caregivers in larger families benefit from shared caregiving responsibilities or stronger emotional and logistical support. This contrasts with literature indicating that larger families sometimes experience more conflicts over caregiving roles, leading to higher stress levels for primary caregivers [33-36].
Research suggests that intervention effects on caregiver stress are often modest [26]. However, psychoeducational interventions have shown the most promise in enhancing caregiver knowledge, reducing caregiver burden and depression, and improving caregiver satisfaction and well-being. Reducing caregiver strain and secondary stressors, such as social isolation, is a valuable approach, though further testing of these interventions is warranted [26]. Recently, highly collaborative care models, particularly in primary care settings, have shown potential in alleviating behavioral symptoms in AD patients and reducing caregiver stress. These models, which have gained prominence in treating mood disorders in older adults, represent a growing area of research over the past 15 years, though questions remain regarding the scope, timing, and dosage of such interventions.
Conclusion
The regression analysis identifies key factors influencing the dependent variable, highlighting the significance of residence, child care, and dementia duration. Residing with the patient and having 1-2 children are positively associated with higher scale categories, suggesting increased caregiving responsibilities impact the outcomes. Conversely, having three or more children shows a significant negative association, possibly indicating a distribution of caregiving duties that reduces individual burden. Additionally, a longer duration of dementia negatively affects the scale categories, reflecting the progressive nature of the disease and its increasing impact over time. Other demographic variables like gender, marital status, education, age, and comorbidity did not show significant effects, indicating that the caregiving context and duration of the disease are more critical determinants of the dependent variable.
References
1. World Health Organization. Global action plan on the public health response to dementia 2017–2025. Geneva: World Health Organization; 2017. 44 p.
2. 2022 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia. 2022;18(4):700–89.
3. Alshammari B, Noble H, McAneney H, Alshammari F, O’Halloran P. Caregiver Burden in Informal Caregivers of Patients in Saudi Arabia Receiving Hemodialysis: A Mixed-Methods Study. Healthcare (Basel). 2023 Jan 28;11(3):366.
4. D’Onofrio G, Sancarlo D, Addante F, Ciccone F, Cascavilla L, Paris F, et al. Caregiver burden characterization in patients with Alzheimer’s disease or vascular dementia. Int J Geriatr Psychiatry. 2015 Sep;30(9):891–9.
5. Lindeza P, Rodrigues M, Costa J, Guerreiro M, Rosa MM. Impact of dementia on informal care: a systematic review of family caregivers’ perceptions. BMJ Support Palliat Care. 2020 Oct 14;bmjspcare-2020-002242.
6. Kamiya M, Sakurai T, Ogama N, Maki Y, Toba K. Factors associated with increased caregivers’ burden in several cognitive stages of Alzheimer’s disease: Caregivers’ burden in Alzheimer’s disease. Geriatrics & Gerontology International. 2014 Apr;14:45–55.
7. Gratão ACM, Brigola AG, Ottaviani AC, Luchesi BM, Souza ÉN, Rossetti ES, et al. Brief version of Zarit Burden Interview (ZBI) for burden assessment in older caregivers. Dement Neuropsychol. 2019;13(1):122–9.
8. Alves LC de S, Monteiro DQ, Bento SR, Hayashi VD, Pelegrini LN de C, Vale FAC. Burnout syndrome in informal caregivers of older adults with dementia: A systematic review. Dement Neuropsychol. 2019;13(4):415–21.
9. Alsebayel FM, Alangari AM, Almubarak FH, Alhamwy R, Alsebayel FM, Alangari A, et al. Prevalence of Dementia and Its Associated Risk Factors Among Geriatric Patients Visiting Primary Healthcare Centers in Riyadh, Saudi Arabia: A Cross-Sectional Study. Cureus. 2022 Apr 22;14(4).
10. Ahlruwaili AA, Chapra M, Kofi M. Prevalence of Burnout in Dementia Caregivers, Riyadh, Saudi Arabia. J Family Med Prim Care. 2022 Jul 13;11(7):2552-7.
11. Mosquera I, Vergara I, Larrañaga I, Machón M, del Río M, Calderón C. Measuring the impact of informal elderly caregiving: A systematic review of tools. Qual Life Res. 2016;25:1059–92.
12. Van Durme T, Macq J, Jeanmart C, Gobert M. Tools for measuring the impact of informal caregiving of the elderly: A literature review. Int J Nurs Stud. 2012;49:490–504.
13. Metcalfe C. Biostatistics: A Foundation for Analysis in the Health Sciences. 7th ed. Wayne W. Daniel, Wiley; 1999. No. of pages: xiv+755+appendices. Statistics in Medicine. 2001;20(2):324–6.
14. Seng BK, Luo N, Ng WY, Lim J, Chionh HL, Goh J, et al. Validity and Reliability of the Zarit Burden Interview in Assessing Caregiving Burden. Ann Acad Med Singap. 2010 Oct 15;39(10):758–63.
15. Li X, Feng X, Sun X, Hou N, Han F, Liu Y. Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990–2019. Front Aging Neurosci. 2020 Sep 29;12:598484.
16. Arai Y, Kudo K, Hosokawa T, Washio M, Miura H, Hisamichi S, et al. Reliability and validity of the Japanese version of the Zarit Caregiver Burden Interview. Psychiatry Clin Neurosci. 1997;51:281-7.
17. Taub A, Andreoli SB, Bertolucci PH. Dementia caregiver burden: reliability of the Brazilian version of the Zarit caregiver burden. Dement Neuropsychol. 2012;6(3):187-96.
18. Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. 1980;20:649-55.
19. Chattat R, Cortesi V, Izzicupo F, Del Re ML, Sgarbi C, Fabbo A, et al. The Italian version of the Zarit Burden interview: a validation study. Int Psychogeriatr. 2011 Jun;23(5):797–805.
20. Sörensen S, Conwell Y. Issues in dementia caregiving: effects on mental and physical health, intervention strategies, and research needs. Am J Geriatr Psychiatry. 2011;19:491-6.
21. Batum K, Çinar N, ?ahin ?, Çakmak M, Kar?ida? S. The connection between MCI and Alzheimer disease: neurocognitive clues. Turk J Med Sci. 2015;45:1137-40.
22. Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, et al. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005;366:2112-7.
23. Truzzi A, Valente L, Ulstein I, Engelhardt E, Laks J, et al. Burnout in familial caregivers of patients with dementia. Braz J Psychiatry. 2012;34:405-12.
24. Garrido R, Menezes PR. Impact on caregivers of elderly patients with dementia treated at a psychogeriatric service. Rev Saude Publica. 2004;28:835-41.
25. Cassis SVA, Karnakis T, Moraes TA, Curiati JAE, Quadrante ACR, et al. Correlation between burden non caregiver and clinical characteristics of patients with dementia. Rev Assoc Med Bras. 2007;53:497-501.
26. Ahlruwaili AA, Chapra M, Kofi M. Prevalence of Burnout in Dementia Caregivers, Riyadh, Saudi Arabia. J Family Med Prim Care Open Acc. 2022;6:192.
27. Campbell P, Wright J, Oyebode J, Job D, Crome P, et al. Determinants of burden in those who care for someone with dementia. Int J Geriatr Psychiatry. 2008;23:1078-85.
28. Cooper C, Katona C, Orrell M, Livingston G. Coping strategies and anxiety in caregivers of people with Alzheimer's disease: the LASER-AD study. J Affect Disord. 2006;90:15-20.
29. Gaugler JE, Roth DL, Haley WE, Mittleman MS. Can counseling and support reduce burden and depressive symptoms in caregivers of people with Alzheimer's disease during the transition to institutionalization? Results from the New York University caregiver intervention study. J Am Geriatr Soc. 2008;56:421-8.
30. Clare L, Wilson BA, Carter G, Breen K, Berrios GE, et al. Depression and anxiety in memory clinic attenders and their carers: implications for evaluating the effectiveness of cognitive rehabilitation interventions. Int J Geriatr Psychiatry. 2002;17:962-7.
31. Adkins VK. Treatment of depressive disorders of spousal caregivers of persons with Alzheimer's disease: a review. Am J Alzheimers Dis. 1999;14:289-93.
32. Prince M, 10/66 Dementia Research Group. Care arrangements for people with dementia in developing countries. Int J Geriatr Psychiatry. 2004;19:170-7.
33. Raz L, Knoefel J, Bhaskar K. The neuropathology and cerebrovascular mechanisms of dementia. J Cereb Blood Flow Metab. 2016;36:172-86.
34. Pudelewicz A, Talarska D, B?czyk G. Burden of caregivers of patients with Alzheimer's disease. Scandinavian journal of caring sciences. 2019 Jun;33(2):336-41.
35. Avargues-Navarro ML, Borda-Mas M, Campos-Puente AD, Pérez-San-Gregorio MÁ, Martín-Rodríguez A, Sánchez-Martín M. Caring for family members with Alzheimer’s and burnout syndrome: impairment of the health of housewives. Frontiers in Psychology. 2020 Apr 21;11:576.
36. Chan CY, Cheung G, Martinez-Ruiz A, Chau PY, Wang K, Yeoh EK, Wong EL. Caregiving burnout of community-dwelling people with dementia in Hong Kong and New Zealand: a cross-sectional study. BMC geriatrics. 2021 Dec;21:1-5.
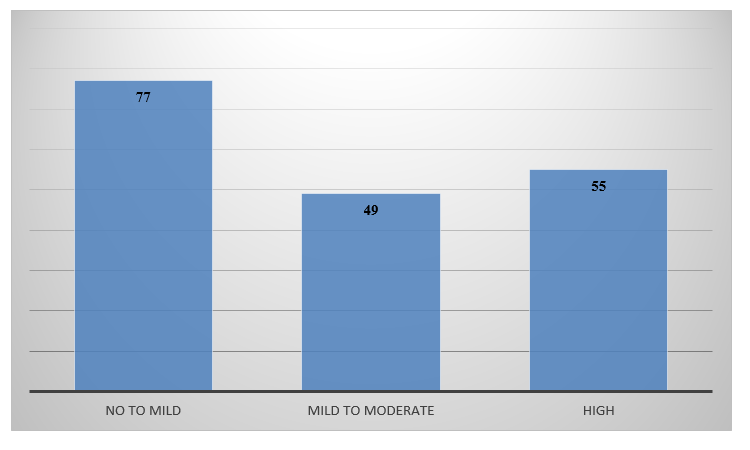
Figure 1
