Intrahepatic Gallbladder Presenting as a Gallbladder Herniation through the Liver
Intrahepatic Gallbladder Presenting as a Gallbladder Herniation through the Liver
Muhammad A Khan1*, Sarah Hamad2, Mario Potvin2.
1. Woodbury High School, 2655 Woodland Drive, Woodbury, MN, 55125.
2, 3. MD, Sanford Medical Center, 3001 Sanford Pkwy, Thief River Falls, MN, 56701.
*Correspondence to: Muhammad A Khan, Woodbury High School, 2655 Woodland Drive, Woodbury, MN, 55125.
Copyright
© 2024: Muhammad A Khan. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 09 Sept 2024
Published: 01 Oct 2024
Abstract
The intrahepatic gallbladder is a rare anatomical anomaly of the gallbladder that has important implications for surgery due to its proximity to the critical biliary and vascular structures, the possibility of associated biliary anomalies, and its potential to cause diagnostic confusion due to the inability to identify its peculiar location preoperatively. We report a rare case where the gallbladder protruded through the substance of the liver to the anterior surface of the liver, mimicking gallbladder hernia. The patient had biliary dyskinesia, and the unusual location of the gallbladder was not suspected preoperatively. The patient underwent a laparoscopic cholecystectomy and had an uneventful recovery. This case is being presented to highlight the extreme technical care to avoid accidental injury to the hepatic biliary and vascular structures.
Key Words: Ectopic Gallbladder; Intrahepatic Gallbladder; Gallbladder Hernia; Anatomic variation; Laparoscopic Cholecystectomy; Biliary Dyskinesia.
Intrahepatic Gallbladder Presenting as a Gallbladder Herniation through the Liver
Introduction
The gallbladder is located on the inferior surface of the liver, on the quadrate lobe between segments IV and V of the liver. Gallbladder congenital anomalies are infrequent. Ectopic gallbladders are extremely rare, with an incidence of 0.1%– 0.7%, and are found in a wide range of locations. Ectopic gallbladder has been classified into four types: intrahepatic, transverse, retroplaced, and left-sided, i.e., to the left of the falciform ligament. Rarely, ectopic gall bladder has been reported in the lesser omentum, falciform ligament, the retroduodenal area, the abdominal wall muscles, and within the thorax (1, 2).
Developmental anomalies during embryogenesis can lead to the formation of an intrahepatic gallbladder, often located in segments IV and V of the liver. This abnormal positioning can result in incomplete emptying of the gallbladder and stasis, leading to the formation of gallstones (3) and the need for complex surgical procedures due to the atypical anatomy (4). The intrahepatic gallbladder may cause problems with the clinical diagnosis of gallbladder disease, particularly gallbladders away from the peritoneum, which may not elucidate typical signs or symptoms of gallbladder disease, hence delaying the diagnosis. Sometimes, the unusual location of the gallbladder away from the liver can predispose to complications like herniation or torsion of the gallbladder (5). Furthermore, delayed diagnosis of cholecystitis in intrahepatic gallbladder cases can lead to abscess formation, causing diagnostic confusion and potentially necessitating formal liver resection to rule out malignancy (6).
Anatomically, the intrahepatic gallbladder may be difficult surgically due to the proximity of the gallbladder to the right anterior and right posterior portal pedicle. The intrahepatic gallbladder may be challenging to identify in imaging investigations. Understanding the anatomical location is critical to avoid accidental injury to adjacent structures, such as hepatic ducts and blood vessels. Traditional imaging modalities, such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI), may inadequately visualize the gallbladder when deeply embedded within the liver parenchyma (7). Advanced imaging techniques and intraoperative cholangiography may be essential to ascertain its location and prevent diagnostic inaccuracies accurately.
Case Report
A 19-year-old morbidly obese female with a history of major depressive disorder visited the clinic due to recurring right upper quadrant pain accompanied by nausea and vomiting over a few months. Despite several ER visits and imaging tests, including ultrasound and CT scan, a non-obstructive stone in the upper pole of the right kidney was the only significant finding. Although she received treatment with analgesics, her symptoms persisted. Further evaluation suggested a hepatobiliary origin for her pain despite normal imaging results for her gallbladder. A HIDA scan revealed a Gallbladder ejection fraction of 3%, leading to a diagnosis of gallbladder dyskinesia. To confirm the diagnosis and assess the potential benefits of surgery, she underwent an evaluation based on the Rome IV criteria for a functional biliary disorder, meeting all the criteria. As a result, she was recommended for a laparoscopic cholecystectomy. During the surgery, the anatomical structure of her gallbladder was found to be quite unusual, with the body being wholly intrahepatic and surrounded by liver tissue. The fundus projected over the surface of the liver mimicking a herniation of the gallbladder through the liver, as shown in Figure 1.
Figure 1. Gallbladder fundus herniating through the anterior surface of the liver.
Only the infundibulum of the gallbladder was found in its expected location. After getting the critical view of safety and transecting the artery and cystic duct, the gallbladder was grasped from the clipped end, and gentle traction was applied. The serosa over the gallbladder and live junction was teased open, and the plane was entered. By careful circumferential dissection and staying on the wall of the gallbladder, the gallbladder was dissected off the liver tissue and retrieved, as shown in Figures 2a, 2b, and 2c. 
Figure 2a,Figure 2b.Figure 2c.
Figure 2 a: Gallbladder being dissected from the substance of the liver; Figure 2b: Demonstration of critical view of safety; Figure 2c: Completed dissection after gallbladder removal.
We used ligasure during this part of the dissection. After ensuring meticulous hemostasis, the rent in the liver tissue was checked for bile leak. Next, the liver rent was packed with omentum to prevent the chances of internal herniation of the bowel. The patient was discharged home a few hours after surgery. On her postoperative visit, the patient was doing well.
Discussion
The intrahepatic gallbladder is a rare anomaly.
Embryologically, the gallbladder and biliary tree develop from an endodermal bud from the foregut during the third week of gestation. The bud bifurcates into hepatic and biliary diverticulum.It remains in the intrahepatic position until the second month, when it emerges from the liver to an extrahepatic position—the intrahepatic gallbladder results from positional arrest during the development (7).
After an extensive search of English literature, we retrieved two cases of gallbladder presenting as gallbladder hernia. Monib S et al. (3) reported a 57-year-old male with an intrahepatic gallbladder presenting like a hernia, which was managed with retrograde open cholecystectomy.
Chilana et al. (8) reported a similar case of intrahepatic gallbladder mimicking a hernia through the gallbladder in a 37-year-old female managed laparoscopically, and the liver edges were divided to prevent internal herniation.
In our case, the gallbladder projecting through the anterior surface of the liver and presenting as a herniation was an unsuspected intraoperative surprise as the anomaly was not anticipated on routine preoperative imaging investigations. The gallbladder infundibulum was the only part of the gallbladder seen at the cystic plate. The cystic duct was extremely short with conventional hepatic arterial anatomy. Cholecystectomy was done by staying right on the wall of the gallbladder to avoid accidental injury to the anterior portal pedicle and segmental ducts and vessels.
Conclusion
When faced with an intrahepatic gallbladder, careful consideration of the surgical approach is crucial. Laparoscopic cholecystectomy is generally the preferred technique for gallbladder removal, provided the gallbladder is readily accessible and not in proximity to significant hepatic structures. When the procedure presents heightened complexity, a transition to open surgery may be warranted to mitigate the risk of complications.
References
1. Chowbey PK, Wadhwa A, Sharma A, Khullar R, Soni V, Baijal M. Ectopic gallbladder: laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2004;14(1):26-8.
2. Chrungoo RK, Kachroo SL, Sharma AK, Khan AB, Nadim AS. Left-sided gall bladder: Report of two cases. J Minim Access Surg. 2007;3(3):108-10.
3. Monib S, Mahapatra P, Habashy HF. Intrahepatic Gallbladder. Eur J Case Rep Intern Med. 2019;6(6):001123.
4. Dhulkotia A, Kumar S, Kabra V, Shukla HS. Aberrant gallbladder situated beneath the left lobe of liver. HPB (Oxford). 2002;4(1):39-42.
5. Guerin JB, Venkatesh SK, Roberts LR. Ectopic Gallbladder. Clinical Gastroenterology and Hepatology. 2015;13(7):e69.
6. Guiteau JJ, Fisher M, Cotton RT, Goss JA. Intrahepatic Gallbladder. Journal of the American College of Surgeons. 2009;209(5):672.
7. Faure JP, Doucet C, Scepi M, Rigoard P, Carretier M, Richer JP. Abnormalities of the gallbladder, clinical effects. Surgical and Radiologic Anatomy. 2008;30(4):285-90.
8. Chilana AS, Singh PK, Bhattacharya K. Intrahepatic Gallbladder Mimicking as “Hernia of the Gallbladder.” Indian Journal of Surgery. 2023;85(5):1308.
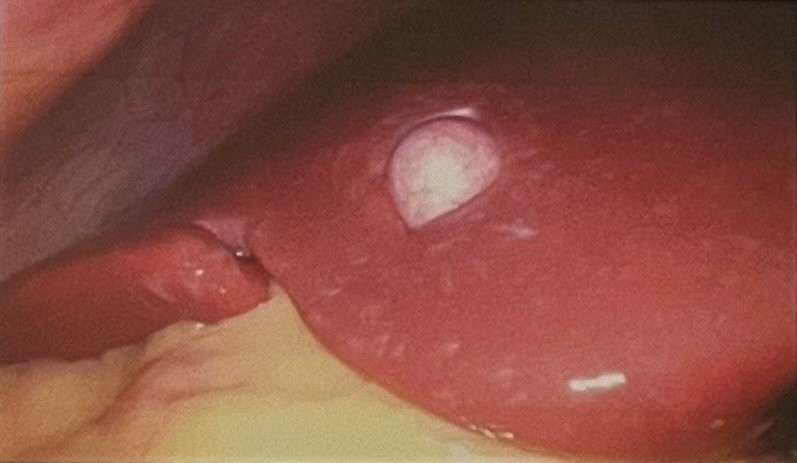
Figure 1
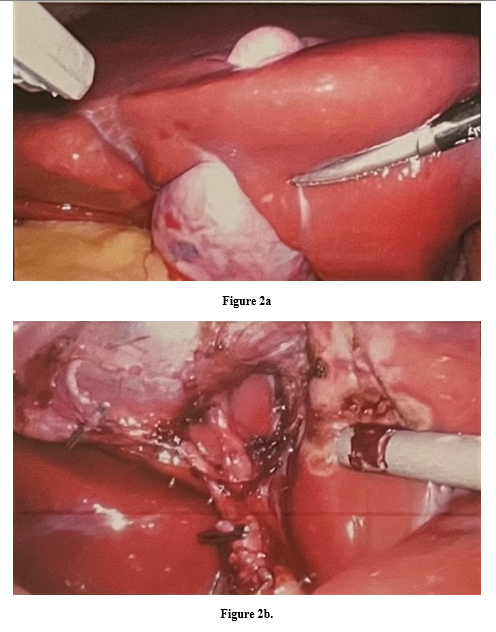
Figure 2
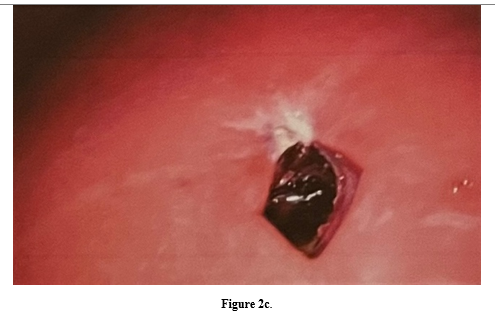
Figure 3
