A Rare Case of a Symptomatic Iatrogenic Arterio-venous Malformation after a Laparoscopic Repair of Uterine Cesarean Scar Isthmocele.
A Rare Case of a Symptomatic Iatrogenic Arterio-venous Malformation after a Laparoscopic Repair of Uterine Cesarean Scar Isthmocele.
Kinda Dargam1, Gayatri Kotni2, George Botros3
*Correspondence to: George Botros, United Arab Emirates.
Copyright
© 2024: George Botros. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 30 Sept 2024
Published: 08 Oct 2024
Abstarct
Uterine Arterio Venous Malformation (AVM) is a rare vascular lesion defined by aberrant arteriovenous connections between the branches of uterine artery and the Myometrial venous plexus.
Uterine AVM can cause massive haemorrhage which is refractory to usual management, hence potentially life threatening (1). Obstetricians & Gynaecologists need to be aware that AVM can arise following uterine surgery and prompt referral to tertiary referral centres with intervention radiology facilities sometimes is recommended.
In this case, AVM happened after a uterine Cesarean Scar Isthmocele repair surgery. The patient presented with heavy bleeding as a result of the iatrogenic AVM. By the time she presented at our hospital, she already experienced significant blood loss and became severely anemic. Diagnosis of AVM was established and she was successfully managed with Bilateral uterine artery embolization.
Key words: Arterio Venous Malformations , Uterine artery embolization, Thromboelastography, Haemostatic resuscitation, Uterine pseudo-aneurysms, Hemorrhagic shock, isthmocele, niche repair.
A Rare Case of a Symptomatic Iatrogenic Arterio-venous Malformation after a Laparoscopic Repair of Uterine Cesarean Scar Isthmocele.
Introduction
Uterine AVM can be congenital or acquired. Most commonly it presents with abnormal uterine bleeding and can be a serious cause of secondary postpartum haemorrhage (2). Usually, it may be confused with retained products of conception, Gestational trophoblastic disease (GTD), , haemangiomas, varicosities and malignancies of the uterus e.g. sarcomas.
Acquired uterine AVMs are frequently missed due to difficulty in diagnosis. they are characterized by abnormal communication between uterine arteries and myometrial venous plexus, deep within myometrium and endometrium. They are largely associated with uterine surgery, D&C, Gestational trophoblastic disease (GTD), endometrial cancer, and infection.
Earlier AVMs are investigated using trans-abdominal or transvaginal Ultrasound, commonly present as a heterogenous, ill-defined mass, with multiple, hypoechoic cystic or serpiginous structures of variable size. Colour Doppler US will reveal intense flow (4).
CT being a quick and non-invasive intervention obviates the need for conventional angiography in patients with normal renal function. CT also helps to delineate the feeding uterine arteries prior to any intervention.
MRI, when available can better characterize the pelvic organs compared to CT (3,6).
The most popular method for treating AVMs is trans arterial endovascular therapy, particularly in cases when there are several arteriovenous shunts (5).
Surgical treatment, by means of hysterectomy may be performed following failed embolization or if fertility is no longer desired.
Caesarean scar defect (Isthmocele) is thinning and indentation of the myometrium at the hysterotomy site during cesarean section that results from inadequate healing of the myometrium at this site. It has been defined by various terms like uterine niche, Isthmocele and uteroperitoneal fistula. Cesarean Scar complications are more prevalent as caesarean sections increase, most likely because of pre-existing scar issues that impair the healing of newly made incision.
Potential complications include Caesarean scar pregnancy, pelvic pain, post menstrual spotting, dysmenorrhea, dyspareunia, uterine rupture, and subsequent infertility problems. Management varies according to type, severity of symptoms and desire for future fertility. Conservative, hormone treatment and surgical repair of the defect among the management options for Isthmocele. (7,8).
Case Presentation
This case study describes the clinical course of a woman with acquired AVMs who presented to our hospital with excessive vaginal bleeding.
A 33 years old with previous 2 caesarean sections underwent laparoscopic uterine cesarean niche excision and repair in another facility. The discharge summary included intraoperative findings of a deep narrow niche of size 10x8x8.5 mm that has been excised and repaired via minimally invasive laparoscopic route. Patient made uneventful post operative recovery and was discharged second day post-operatively.
She had her period 2 days after the surgical repair and was average menstrual vaginal bleeding for 7 days.
Two days after, she started having sudden heavy vaginal bleeding foe which she went to a Private facility, after admission bleeding was controlled by Tranexamic acid. As per patient the ultrasound pelvis which was done at that facility no abnormality was detected.
She presented to the emergency department of our hospital around 1 week after that episode with vaginal bleeding. Upon arrival, her general condition was stable, her vitals were normal and she was having mild bleeding. Ultrasound was done in the emergency department, which showed mixed echogenic area at the Caesarean scar measuring 18x14 mm. Cervix was open with mixed echogenic mass ? large blood clot measuring 59x60x92mm. . Soon after the scan she started active heavy vaginal bleeding and went into hemorrhagic shock. She was tachycardic and hypotensive. Emergency resuscitative measures were initiated immediately. As a matter of urgency, she was transferred to the operation theatre (OT) for emergency exploration of the uterus under General anaesthesia.
Initial assessment showed Hgb 8.1g/L , WBC 17X109/L , bhcg negative , Elevated LFTs, CRP 4, Fibrinogen 2.8 g/L, and deranged coagulation. Soon her Hgb dropped to 4.3 g/L and then to 3.4g/L .
She was given 2 units of O-negative blood , 2 gms of fibrinogen and 2 gms of tranexamic acid. ROTEM ( Thromboelastography) has been used to guide in haemostatic resuscitation.
Ultrasound done in the operating theatre showed a small clot in front of the previous niche repair site and the uterine cavity was empty without any clots. There was small amount of blood in the pouch of Douglas and no collection at hepato-renal angles. About 200ml of organized clots were removed from the vagina. Cervix and vagina were normal on speculum examination, and the bleeding had stopped. Although exploratory laparotomy has been discussed and planned, at this point, there was no radiological evidence to support the procedure. Moreover, correcting anaemia and coagulopathy before proceeding to any surgical intervention was the main priority as the bleeding had settled. Blood loss in operating theatre was 250 ml and total blood loss altogether was around 3000-4000ml at this point.
She was put under close supervision in the High dependency unit. Her haemoglobin improved to 8.7 gms. No active bleeding was observed during her hospital stay.
A CT scan with contrast to rule out active bleeding/AVM was performed the following day. The CT scan showed 2.3 x1.8 cm hypodensity at the junction of the upper two-thirds and lower one-third of the anterior uterine wall at the left lateral border of the uterine Isthmocele repair . it was described as a focal contrast-filled structure seen in the left adnexa having enhancement similar to that of arteries on arterial and venous phases without significant change in the size on venous phase – this seemed to be an AV abnormality.
She was commenced on Norethisterone, GnRh analogues and underwent bilateral uterine artery embolization successfully and discharged home the next day with follow-up appointment.
She was reviewed again 2 weeks after the procedure and found t be in good condition with no further bleeding. Repeat MRI 4 months post procedure showed complete resolution of the AVM defect with good healing of the repaired cesarean scar defect. There was no significant fluid collection compared to the previous Ultrasound findings. She was started on Progesterone only contraceptive tablets.
Figure 1: Transvaginal image of the repaired uterine scar area
Figure 2a: Hematoma seen at site of the repaired scar area
Figure 2b: Hematoma seen at site of the repaired scar area
Figure 3: Doppler images of the AVM area
Figure 4: CT image of the AVM site
Discussion
This is a rare case of formation of pseudo uterine artery aneurism (AVM) resulted from the excision and repair of the cesarean scar niche area. This can result from the partial injury to the uterine artery or its descending cervical branch. That particular injury could occur if excision of the scar extended laterally towards the uterine vessels and included in the repaired defect. That particular complication during niche repair, as far as we aware has not been reported in the literature.
References
1. Agarwal N, Chopra S, Aggarwal N, Gorsi U. Congenital Uterine Arteriovenous Malformation Presenting as Postcoital bleeding: A Rare Presentation of a Rare Clinical Condition. J Clin Imaging Sci 2017; 7:11.
2. Fleming H, Ostör AG, Pickel H, Fortune DW. Arteriovenous malformations of the uterus. Obstet Gynecol 1989; 73:209.
3.Nasu K, Fujisawa K, Yoshimatsu J, Miyakawa I. Uterine arteriovenous malformation: ultrasonographic, magnetic resonance and radiological findings. Gynecol Obstet Invest 2002; 53:191.
4.Timor-Tritsch IE, Haynes MC, Monteagudo A, et al. Ultrasound diagnosis and management of acquired uterine enhanced myometrial vascularity/arteriovenous malformations. Am J Obstet Gynecol 2016; 214:731.e1.
5. Badawy SZ, Etman A, Singh M, et al. Uterine artery embolization: the role in obstetrics and gynecology. Clin Imaging 2001; 25:288.
6. Huang MW, Muradali D, Thurston WA, et al. Uterine arteriovenous malformations: gray-scale and Doppler US features with MR imaging correlation. Radiology 1998; 206:115.
7. Berghella, V., MD (2024, April 19). Cesarean birth: Postoperative care, complications, and long-term sequelae. UpToDate. Retrieved May 31, 2024, from https://www- uptodate-com.eu1.proxy.openathens.net/contents/cesarean-birth-postoperative- care-complications-and-long term sequale
8. Salmeri, N., Papale, M., & Montresor, C. (2022). Uterine arteriovenous malformation (UAVM) as a rare cause of postpartum hemorrhage (PPH): A literature review. Springer. https://doi.org/10.1007/s00404-022-06498-0
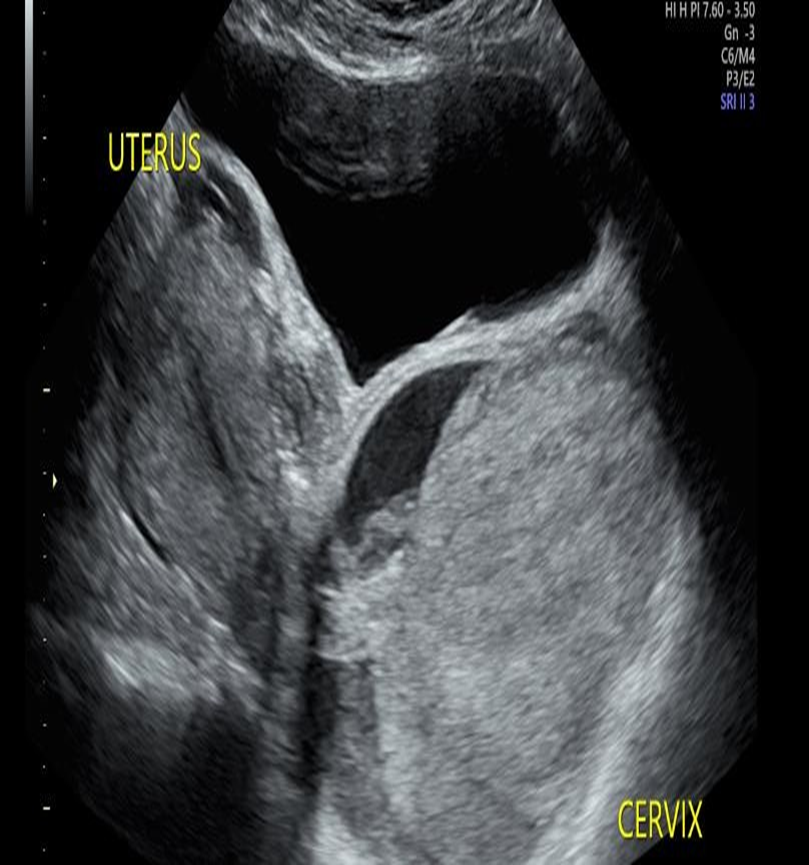
Figure 1
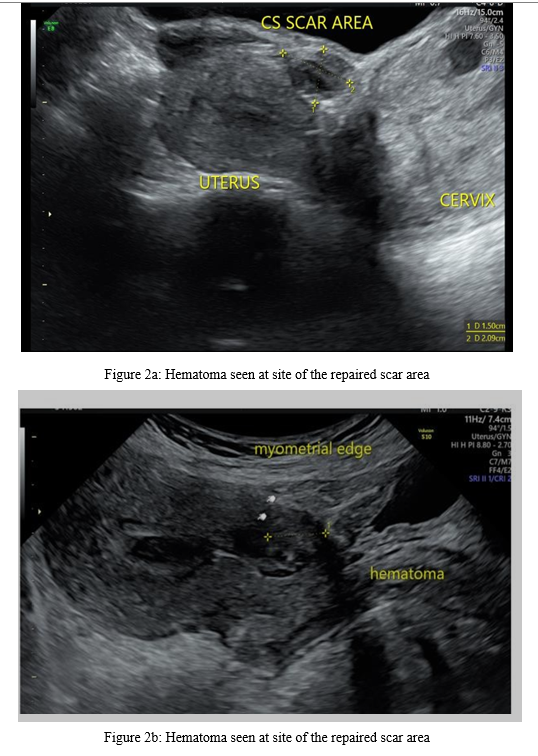
Figure 2

Figure 3
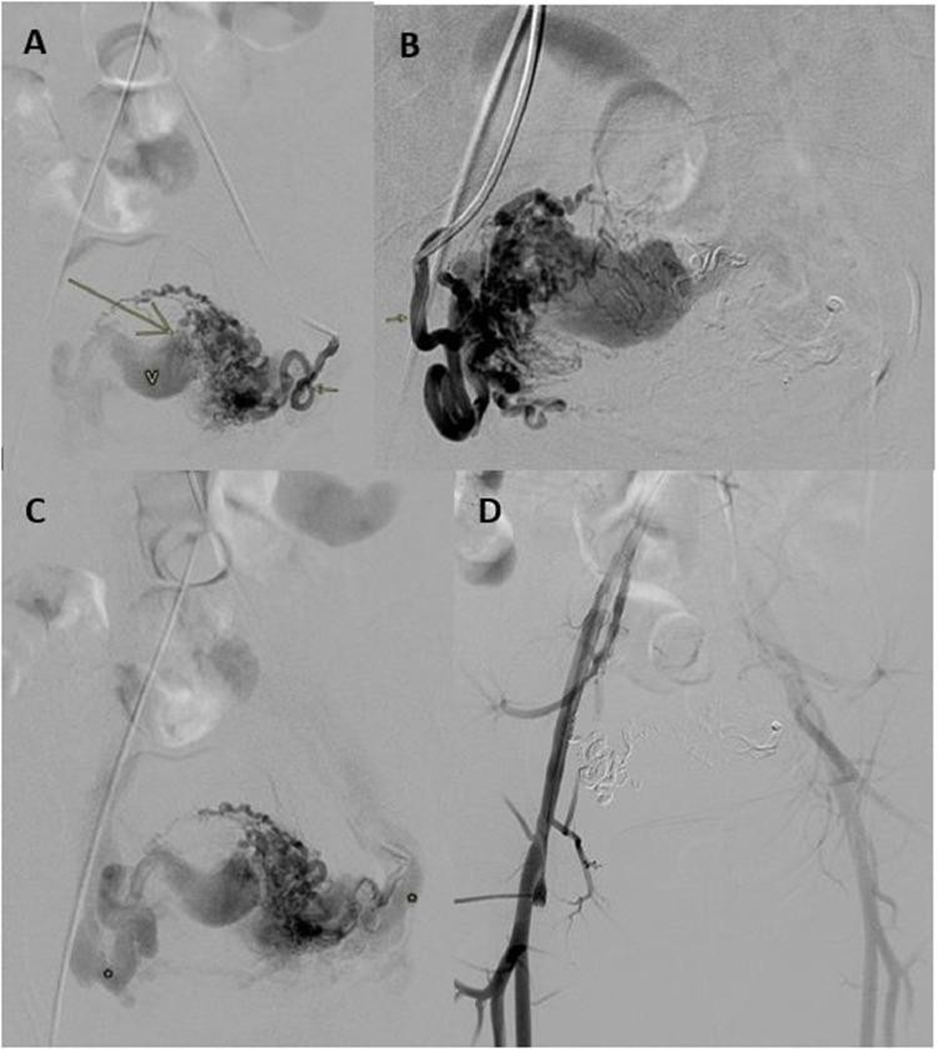
Figure 4
