4 Years Old Boy with Four Toes Nails Melanonychia and Recurrent Hemolytic Anemia due to G6PD
4 Years Old Boy with Four Toes Nails Melanonychia and Recurrent Hemolytic Anemia due to G6PD
Dr. Ahmed Moosa Yahya Assery*, Dr. Mohammad Abdullah Elomair *
*Correspondence to:
Dr. Ahmed Moosa Yahya Assery, Paediatrics ambulatory care consultant. King Abdulaziz Medical City, National Guard Medical Affairs, Family Medicine-Ambulatory care, NGCSC.RDH.KSA.
Dr. Mohammad Abdullah Elomair, Internal medicine ambulatory care consultant, King Abdulaziz Medical City, National Guard Medical Affairs, Family Medicine-Ambulatory care, medical field. RDH.KSA.
Copyright
© 2024: Dr. Ahmed Moosa Yahya Assery, Dr. Mohammad Abdullah Elomair. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 10 Sep 2024
Published: 15 Sep 2024
Abstract
We have here for you such attractive case for a boy who is 4 years old known to me via the regular FU due to the recurrent HL caused by the G6PD he is having and presented to me recently with MLN of four toes nails which is the darkness pigmentation of the toes nails that was so striking and diffuse in the affected toenails. Nothing mentioned in our medical environment offices of paediatrics blood t there is a known relations between the blood disorders in children and any skin hyperpigmentation except the Fanconi Anaemia. So, on this case report maybe we will be the first peoples who recorded the second haematological disorder that comes with cutaneous pigmentation (Hemocutaneous stigmata) if it is really and correct terminology.
4 Years Old Boy with Four Toes Nails Melanonychia and Recurrent Hemolytic Anemia due to G6PD
Keywords:
FU: Follow up.
HL: Hemolysis.
G6PD: Glucose-6-Phosphate Dehydrogenase Deficiency.
MLN: melanonychia.
KSA: Kingdom of Saudi Arabia.
RDH: Riyadh.
NGCSC: National guard Comprehensive Clinics.
AHA: Acute haemolytic anaemia
Introduction
G6PD: G6PD: is an inherited disorder caused by a genetic defect in the red blood cell (RBC) enzyme G6PD, which generates NADPH and protects RBCs from oxidative injury. G6PD deficiency is the most common enzymatic disorder of RBCs. The severity of haemolytic anaemia varies among individuals with G6PD deficiency, making diagnosis more challenging in some cases. Identification of G6PD deficiency and patient education regarding safe and unsafe medications and foods is critical to preventing future episodes of haemolysis.
This topic review discusses the clinical manifestations, diagnosis, and management of G6PD deficiency. Separate topic reviews discuss the genetic testing and pathogenesis of G6PD deficiency and an overall approach to the patient with unexplained haemolytic anemia.
G6PD deficiency is the most common enzymatic disorder of red blood cells (RBCs), affecting 400 to 500 million people worldwide. G6PD deficiency is global in its distribution (figure 1) It occurs most often in the
tropical and subtropical zones of the Eastern Hemisphere (e.g., Africa, Europe, Middle East, Asia), with prevalence of 20 percent or more in some regions. Examples of prevalence numbers include people from the following populations or countries:
Figure 1: The map shows the prevalence of G6PD deficiency variants throughout the world, with darker colours indicating higher prevalence. It was constructed from several sources; see the source document for details. Refer to UpToDate for additional information on the epidemiology, clinical presentation, and diagnostic evaluation for G6PD deficiency.
Kurdish Jews – 60 to 70 percent.
Sardinians – 4 to 35 percent, depending on the village.
Bahrain – 23 to 31 percent.
Nigeria – 22 percent.
Thailand – 17 percent.
African Americans – 11 to 12 percent.
Saudi Arabia – 8 percent.
Black people from Brazil – 8 percent.
Greece – 6 percent.
South China – approximately 6 percent.
Egypt – 4 percent.
India – 3 percent.
Japan and Korea – 0 to 1 percent.
This geographic distribution is highly correlated with regions in which malaria was once endemic, leading to the hypothesis that G6PD deficiency may have conferred a selective advantage against infection by Plasmodium falciparum, like observations with other gene variants affecting RBC properties. Clinically The clinical expression of G6PD deficiency encompasses a spectrum of disease severity. The severity of disease and the likelihood of developing neonatal jaundice or chronic haemolysis, and the magnitude of haemolysis when haemolytic episodes occur, depends on the degree of the enzyme deficiency, which in turn is determined by the characteristics of the G6PD variant.
?The majority of individuals are asymptomatic and do not have haemolysis in the steady state. They have neither anaemia, evidence of increased red blood cell (RBC) destruction, nor alteration in blood morphology, although a modest shortening of RBC survival can be demonstrated by isotopic techniques This includes almost all individuals with the most prevalent G6PD variants, G6PD A - and G6PD Mediterranean. However, episodes of acute haemolysis with haemolytic anaemia may be triggered by medications, certain foods (especially fava beans), and acute illnesses, especially infections.
?The rare individuals with severe disease (class A variants) usually have chronic haemolysis.) In many cases, women who have inherited one abnormal G6PD allele are unaffected carriers. However, as noted above, those with skewed lyonization may have clinical disease. Women who are homozygous or compound heterozygous for an abnormal G6PD gene will have a phenotype like men.
Table 1: factors causing HL in the G6PD). (6).`
AHA — Some individuals with G6PD deficiency have episodes of acute haemolysis in the setting of oxidant injury from medications, acute illnesses, and certain foods such as fava beans (table 1)(6). Once patients are diagnosed and can reduce oxidant stress exposures through medication avoidance, the frequency of haemolysis may decline dramatically. Episodes of acute haemolysis are more common in individuals with G6PD Mediterranean, which has a half-life measured in hours, than with G6PD A-, which has a half-life measured in days.
G6PD-deficiency-associated haemolytic anaemia can falsely lower the HbA1C level due to increased RBC turnover, as with other haemolytic anaemias, but G6PD deficiency does not alter the HbA1C by mechanisms other than haemolysis. (1).
Figure 2: Longitudinal melanonychia bands in an individual with darkly pigmented skin presenting as multiple lines on a Gray background
MLN: is common in individuals with darkly pigmented skin and typically affects multiple nails in individuals of African descent, melanonychia occurs in up to 77 percent of young adults and almost 100 percent over 50 years. In Japanese populations, it affects 10 to 20 percent of adults. On dermoscopy, this type of physiologic MLN presents as a Gray homogeneous band with or without thin regular lines (figure 2) .(2).
MLN is a very worrisome entity for most patients. It is characterized by brownish black discoloration of nail plate and is a common cause of nail plate pigmentation. The aetiology of MLN ranges from more common benign causes to less common invasive and in situ melanomas. MLN especially in a longitudinal band form can be due to both local and systemic causes. An understanding of the epidemiology, pathophysiology and clinical details is necessary for adequate patient care and counselling. It not only helps in the early recognition of melanoma but also prevents unnecessary invasive work up in cases with benign etiology. An early diagnosis of malignant lesion is the key to favourable outcome. Though there are no established guidelines or algorithms for evaluating melanonychia, a systematic stepwise approach has been suggested to arrive at a probable etiology. We, hereby, review the aetiology, clinical features, diagnostic modalities, and management protocol for melanonychia. (3).
Etiology of the MLN:
1. Melanocytic activation—Refers to increased melanin production from normal number of activated melanocytes in the nail matrix. It is also known as melanocyte stimulation,
2. Melanocyte proliferation—Means increased melanin pigment secondary to increased number of melanocytes in the nail matrix. The melanocytic hyperplasia or proliferation can be benign or malignant.
Nail matrix nevus and constitutional nail pigmentation are the most common causes. The percentage distribution of the aforesaid causes varies in different population. The most common cause in a study evaluating MLN of all morphologies was found to be subungual haemorrhage (29.1%), followed by nail matrix nevus (21.8%), trauma (14.5%), lentigo (11.6%), and race (8.0%). While in a study evaluating only longitudinal MLN, racial MLN was seen in 68.6%, trauma in 8.5%, fungal in 7.1%, and mixed ethology in 4.5% of cases. Benign melanocytic hyperplasia and nail apparatus malignancy contributed to 5.7% cases each. (3).
Figure 3: One of the laboratory blood tests of the case showing low G6PD, Normal range for his age is 4.0-13.0 U g Hb
Our Case Presentation
As we mentioned early about what we are presuming a new medical terminology “Hemocutaneous stigmata, here we are trying to see any connections between the blood disorder our patient is having -G6PD, (figure 3) and the toenail manifestation he is having-MLN, (figure 4-5). After the broad search in the midline search see what we got:
Figure 4-5: Our case report toenails melanonychia in both feet as showed here the right foot with two nails and the left one with only one nail.
1_ In Dermo-Sifiliográficas Vol. 111. Issue 9.Pages 771 -772 (November 2020) published by L. Cristián Fischera,, M. Matías Sanhuezab under the title of “ The First Case of Skin Hyperpigmentation and Melanonychia Due to Hydroxychloroquine in Chile where the correlation between the MLN with any haematological disorder was not direct really , otherwise the correlation was here in this interesting case was between the MLN and the famous drug used for the haemato-infectious disorder which is the Malaria in that article concluded that
Few cases of skin hyperpigmentation induced by hydroxychloroquine have been reported in such literature and nail involvement is the rarest adverse effect .It manifests as patches of variable colour (greyish-blue, coffee-yellow, or dark purple), which can appear on the oral mucosa (hard palate and gums) and skin, mainly on the face, torso, back, nails, anterior surface of the arms, hands, legs, and feet. (4).
2_in the famous website of the very-well health in the issued in 2023 September by By Susan J. Huang, MD and Medically reviewed by Danielle McNeil, D.P.M
Under the title Brown Line on Nails: Vitamin Deficiencies and Other Medical Causes, this great article mentioned that the prevalence of melanonychia is about 1% of people of any age, but it’s extremely rare in children. More than 50 years of research suggests that just 16 cases of melanonychia have been documented in children and they were diagnosed as melanoma cancer, that was published by: Ansari MS, Mahmoudi H, Sadeghinia A, Azizzadeh-Roodpishi S, Ghanadan A, Daneshpazhooh M. Dermoscopic Evaluation of Longitudinal Melanonychia in Children: A Prospective Study. Indian J Dermatol. 2021 Jul-Aug;66(4):445. doi: 10.4103/ijd.IJD_722_20.
There are differences in how melanonychia looks in adults compared to how it looks in children. The commonest causes of the paediatrics MLN are:
Traumatic or infectious causes:
- Injury (e.g., nail-biting, stubbed toes, wearing shoes that do not fit, slamming your finger in a door)
- Infections
Medical condition-related causes:
- Lichen planus
- Lupus
- Psoriasis
- Amyloidosis
- Hyperthyroidism
- Addison’s disease
- Skin cancer
- HIV/AIDS
- Cushing’s syndrome
Health-related causes:
- Sun sensitivity (photosensitivity)
- Iron overload
- Nutrient deficiencies
- Pregnancy
- Growth hormone problems
- Warts
Treatment-related causes:
- Phototherapy
- X-rays
- Radiation
- Chemotherapy
- Medications to treat malaria. (5).
That is the maximum form the midline search correlating indirectly between the MLN and G6PD in pediatrics since of the scarcity of the resources that mean maybe we are the first people open the gate of such correlation via such interesting cases.
Conclusion
From this case report of this G6PD boy with recurrent HL who presented recently with MLN we will ask ourselves are we dealing with a new cause of the toenail MLN which is the G6PD or not? Let wait the coming publishments.
Conflicts of Interest: The authors declare no conflicts of interest.
References
1.https://www.uptodate.com/contents/diagnosis-and-management-of-glucose-6-phosphate-dehydrogenase-g6pd-deficiency?search=g6pd%20deficiency&source=search_result&selectedTitle=1%7E138&usage_type=default&display_rank=1.
2-https://www.uptodate.com/contents/dermoscopy-of-nail-pigmentations?search=melanonychia&source=search_result&selectedTitle=2%7E16&usage_type=default&display_rank=2#H61932105.
3- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7001389/
4-https://www.actasdermo.org/en-the-first-case-skin-hyperpigmentation-articulo-S1578219020302900
5-https://www.verywellhealth.com/what-is-longitudinal-melanonychia-1069479
6-https://emorymedicine.wordpress.com/2024/04/11/midtown-morning-report-what-is-the-association-of-bactrim-induced-hemolysis-in-the-setting-of-g6pd-deficiency/
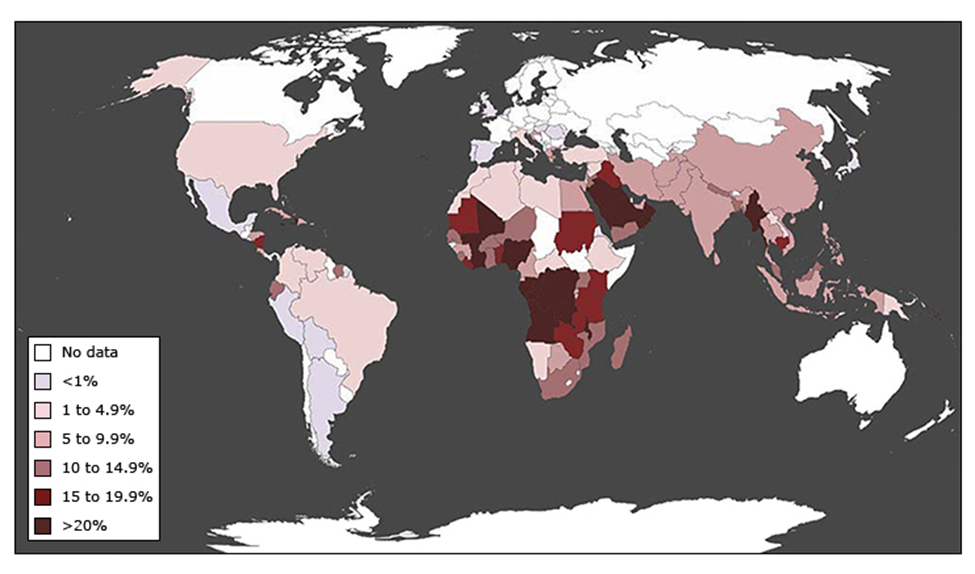
Figure 1
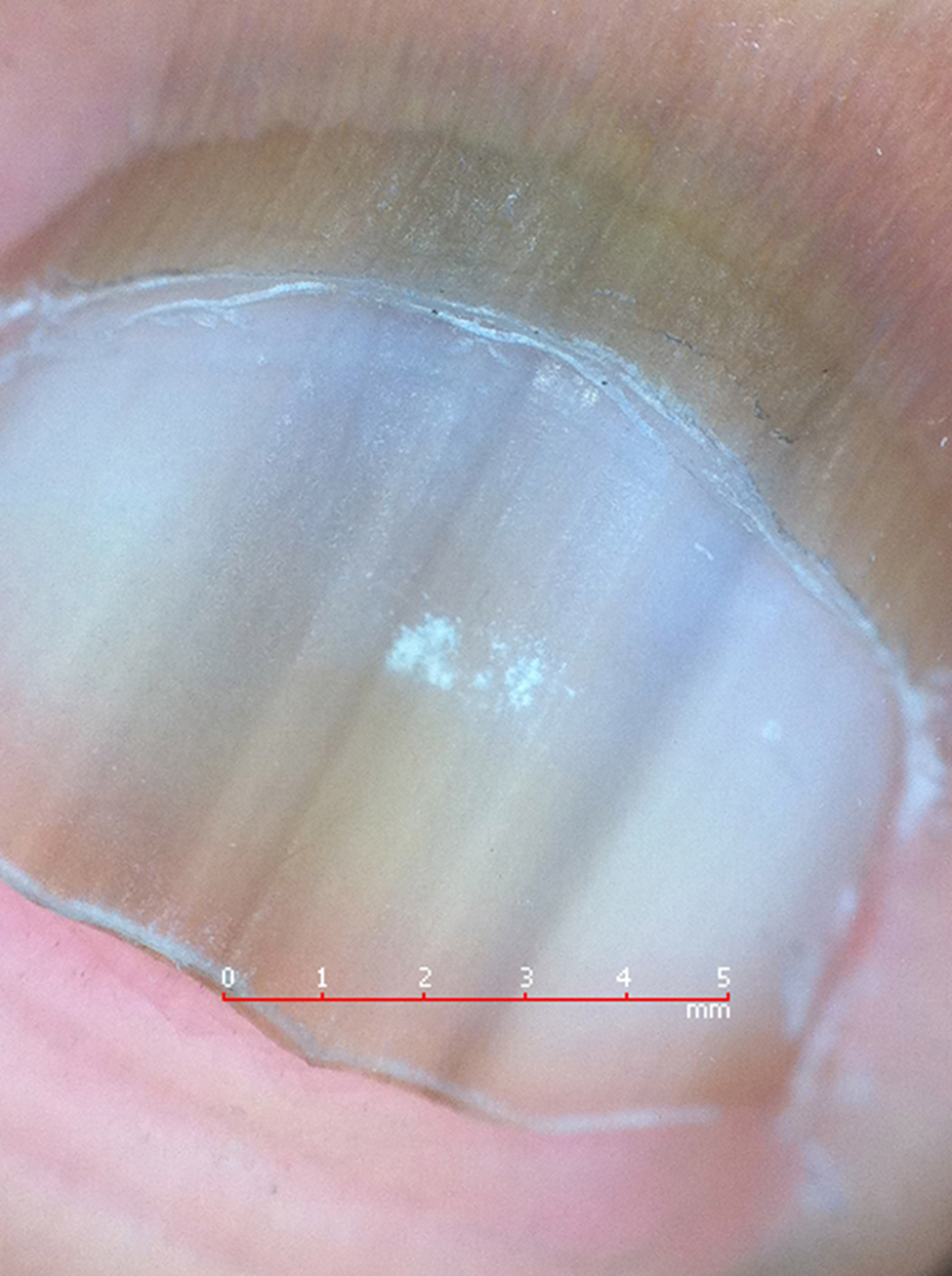
Figure 2
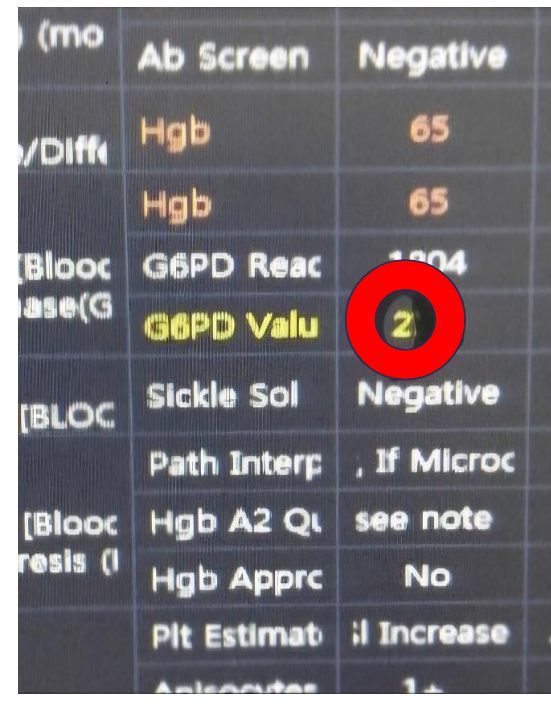
Figure 3

Figure 4

Figure 5
