Left Ovarian Vein Thrombosis Mimicking Pyelonephritis: A Case Report
Left Ovarian Vein Thrombosis Mimicking Pyelonephritis: A Case Report
Sara Osmana*, Walid Abd Alhameedb, Sami Elsharifc
a: Department of Obstetrics & Gynaecology, Muhayil General Hospital, Muhayil Aseer, KSA.
b: Department of Internal Medicine, Muhayil General Hospital, Muhayil Aseer, KSA.
c: Department of Obstetrics & Gynaecology, Muhayil General Hospital, Muhayil Aseer, KSA.
*Correspondence to: Sara Osman, Department of Obstetrics & Gynaecology, Muhayil General Hospital, Muhayil Aseer, KSA.
Copyright
© 2024 Sara Osman. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 09 October 2024
Published: 23 October 2024
DOI: https://doi.org/10.5281/zenodo.13979940
Abstract
Introduction
Ovarian vein thrombosis (OVT) is an uncommon condition, most frequently occur in the postpartum period. The presentation includes pelvic pain, fever, and abdominal mass. Although a rare diagnosis, OVT can potentially cause fatal complications; thus, early recognition and prompt treatment are important.
Case presentation
We present a case of a 29-year-old lady, Para 2, previously healthy, who presented 10 days after vaginal delivery with left-sided flank pain, fever, and burning micturition. The patient had a vaginal delivery at term complicated by extended episiotomy, which was sutured in operative theatre. Laboratory tests revealed elevated white blood cell (WBC) count (12000 cells/mm3) with neutrophilia and (20-25 WBC in high power field) in urine examination. The initial differential diagnosis was cystitis or pyelonephritis. Abdominal ultrasound showed an enlarged left kidney, no stones or hydronephrosis. Abdominal and pelvic contrast-enhanced computed tomography (CT) scan showed left OVT extending to the left renal vein and inferior vena cava. Urine culture was positive for Escherichia coli. Thus, she was started on anticoagulants, and antibiotics and discharged home after improvement. Follow-up revealed the resolution of the clot.
Conclusion
OVT is a rare condition, usually in the postpartum period. Its presentation can mimic other differential diagnoses, so a high index of suspicion is required for prompt diagnosis and management. Diagnosis can be obtained using a CT scan, magnetic resonance, or ultrasound (US) Doppler. Treatment includes a combination of anticoagulants and antibiotics. The prognosis is good nowadays.
Left Ovarian Vein Thrombosis Mimicking Pyelonephritis: A Case Report
Introduction
Ovarian vein thrombosis (OVT) is a rare condition most frequently seen in the immediate postpartum period. OVT has been reported in ~2% of births by Cesarean section (C-section) and in 0.05–0.18% of vaginal births (1). It can also arise in association with endometritis, pelvic inflammatory disease, malignancy, pelvic surgery, inflammatory bowel disease, and thrombophilia (2). However, it can be classified as idiopathic in 4 to 16% of cases (3). Although it is rare, OVT can cause fatal complications; therefore, recognition and early treatment are important.
Case Report
We present a case of a 29-year-old lady, Para 2, previously healthy, who presented 10 days after vaginal delivery with left-sided flank pain, low-grade fever, and burning micturition. The pain was not radiating with no aggravating or relieving factors. The patient had a vaginal delivery at term complicated by extended episiotomy, which was sutured in the operative theatre. Upon examination, she looked ill and in pain. She was febrile and hemodynamically stable. Abdominal examination revealed left lower tenderness, with no palpable masses nor organomegaly.
Laboratory exams revealed elevated white blood cell (WBC) count (12000 cells/mm3) with neutrophilia and (20-25 WBC in high power field) in urine examination. Other inflammatory markers like c-reactive protein (CRP) and erythrocyte sedimentation rate were also high. The initial differential diagnosis was cystitis or pyelonephritis. Abdominal ultrasound showed an enlarged left kidney, no hydronephrosis and no stones. A urine sample was sent for culture and sensitivity. The patient was admitted, and antibiotics and painkillers were initiated. An abdominal and pelvic computed tomography (CT) scan was arranged to be done the next day. CT scan with contrast showed left OVT (Figure 1, Figure 2) extending to the left renal vein (Figure 3) and inferior vena cava. Thus, she was started on anticoagulants. Urine culture was positive for Escherichia coli (ESPLs). She received low molecular weight heparin (LMWH) and shifted to warfarin. The patient was discharged home after 1 week on warfarin & oral antibiotics. A follow-up CT scan after 3 months, revealed the resolution of the clot.
Figure 1: Contrast-enhanced CT scan shows left ovarian vein with filling defect & ring enhancement indicating the thrombus (red arrow).
Figure 2: Coronal view, contrast-enhanced CT scan demonstrates distended thrombosed left ovarian vein (red arrow)
Figure 3: Coronal view, contrast-enhanced CT scan demonstrates distended thrombosed left renal vein (red arrow)
Discussion
Ovarian vein thrombosis (OVT) is a rare venous thrombosis. Compared to lower limb vein thrombosis, it is 60 times less frequent (4). Due to the anatomy of the ovarian veins, the right ovarian vein is more frequently involved (70–80% of cases); also, it was reported bilaterally (around 10% of cases). Nevertheless, in this patient, it was left-sided. The pathophysiology of OVT is also related to the Virchow triad: venous stasis, vascular injury, and hypercoagulability (5).
Mostly it is a postpartum complication (6). Postpartum OVT can occur within 4 weeks after delivery, but it peaks around 2 to 6 days after delivery, and in 90% of women arises within 10 days (5). OVT can also be associated with pelvic surgeries, cancer, inflammatory disorders, or thrombophilia (3). Although it is rare, OVT can have serious complications. If not diagnosed and managed can be complicated by sepsis, extension to the inferior vena cava or renal vessels, or rarely pulmonary embolism (PE). The usual presentation is fever, abdominal pain, and abdominal mass a few days after delivery (7). In this case, there was pain and fever, but no mass was felt upon examination. Also, burning micturition and features of infection in her urine examination directed the doctors toward the diagnosis of a complicated urinary tract infection. However, the tenderness was mainly lower abdominal not consistent with her complaint of flank pain, and raised a possibility of other pathology. The hypercoagulability state, as she was in the postpartum period and the infection, both of them possibly played a role in her OVT. It requires a high index of suspicion to diagnose OVT, as symptoms are nonspecific, and abdominal pain is a very common complaint in the emergency department (8). Differential diagnoses can involve pyelonephritis, tubo-ovarian abscess, broad ligament hematoma, ovarian torsion, and appendicitis (9). Therefore, imaging studies are usually required to reach the diagnosis of OVT (8). Sepsis is often first suspected, hence investigations including a full blood count, urea and creatinine, CRP, lactate, and cultures are performed. Although OVT can be associated with leucocytosis and high CRP, these are not specific to thrombosis (10).
OVT can be diagnosed by Doppler ultrasound, contrast-enhanced computerized tomography (CT) scan, and magnetic resonant angiography (MRI). MRI is 100 percent sensitive and specific. Ultrasound accuracy sometimes can be affected by the operator or overlying bowel gas. Still, it is very important in initial investigations and follow-up (11). Contrast-enhanced CT scan is primarily used to diagnose OVT (12). It has a high sensitivity and specificity and it is easily obtainable and is more cost-effective than (MRI) (11).
The suggested management of postpartum OVT is a short duration (3 months) of anticoagulation, with the addition of antibiotics especially if infection is suspected (7). OVT has a good prognosis and patient symptoms usually improve in a few days. Follow-up is needed to ensure thrombus resolution and recanalization of the ovarian vein. Oral anticoagulant efficacy has not been proven (13). In recurrent PE or contraindication to anticoagulant, thrombectomy or inferior vena cava filter may be used (7).
This patient started on intravenous antibiotics on admission. When the diagnosis of OVT was done, she was started on LMWH and within 1 week, transitioned to warfarin. Symptoms improved within 2 days. CT scan was repeated 3 months later and resolution of thrombus was confirmed. She had a referral to the hematology unit for thrombophilia screening. Recurrence in future pregnancy is low, but still, there is limited data in this area. Screening for thrombophilia is advised especially in idiopathic OVT (14).
Conclusion
Ovarian vein thrombosis is an uncommon condition. It should be in mind if any woman presents with fever and abdominal pain, especially in the postpartum period. CT scan is usually used for diagnosis, although other modalities may be used. Treatment consists of anticoagulation to treat thrombosis and antibiotics. Morbidity is rare nowadays and it is due to PE and sepsis. The outcome with treatment is most commonly complete resolution of thrombus and the risk of recurrence is rare.
References
1- El Mawla, Zeinab MDa; Damen, Bilal MDb.Postpartum ovarian vein thrombosis: a case report.Annals of Medicine & Surgery 85(6):p 3082-3085, June 2023. DOI:10.1097/MS9.0000000000000838
2- Aguilar S, Cunha V, Martins L, et al. Ovarian vein thrombosis: a case report. Int J Med Rev Case Rep 2018;2:1.
3- Nicoletta Riva , Jean Calleja-Agius. Ovarian Vein Thrombosis: A Narrative Review. Hamostaseologie 2021; 41(04): 257-266. DOI: 10.1055/a-1306-4327
4- Z. El Mawla, B. Damen. Postpartum ovarian vein thrombosis: a case report. Ann. Med. Surg., 85 (6) (May 2023), pp. 3082-3085, DOI:10.1097/MS9.0000000000000838
5- N Riva, J Calleja-Agius. Ovarian vein thrombosis: a narrative review. Hamostaseologie, 41 (04) (2021), pp. 257-266
6- N. Kodali, I. Veytsman, S. Martyr, K. Lu. Diagnosis and management of ovarian vein thrombosis in a healthy individual: a case report and a literature review. J Thromb Haemostasis, 15 (2017), pp. 242-245
7- Bannow BTS, Skeith L. Diagnosis and management of postpartum ovarian vein thrombosis. Hematology Am Soc Hematol Educ Program 2017; 2017: 168–171.
8- K. Harris, S. Mehta, E. Iskhakov, M. Chalhoub, T. Maniatis, F. Forte, H. Alkaied
Ovarian vein thrombosis in the nonpregnant woman: an overlooked diagnosis.Ther. Adv. Hematol., 3 (5) (2012), pp. 325-328, DOI:10.1177/2040620712450887
9- Khlifi A., Kebaili S., Hammami M., Berregaya L., Hidar S., Affes N., and Khairi H., Postpartum ovarian vein thrombophlebitis: report of a case and review of the literature, North American Journal of Medical Sciences. (2010) 389–391,https://doi.org/10.4297/najms.2010.2389.
10- Dougan C, Phillips R, Harley I, Benson G, Anbazhagan A. Postpartum ovarian vein thrombosis. Obstet Gynaecol. 2016;18(4):291–9.
11- AA Jenayah, S Saoudi, F Boudaya, I Bouriel, E Sfar, D Chelli. Ovarian vein thrombosis. Pan Afr Med J, 21 (2015), p. 251.
12- Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D, Bounameaux H, Huisman M, King CS, Morris TA, Sood N, et al: Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest.149:315–352. 2016.
13- N. Kodali, I. Veytsman, S. Martyr, K. Lu.Diagnosis and management of ovarian vein thrombosis in a healthy individual: a case report and a literature review. J. Thromb. Haemost., 15 (2) (Feb. 2017), pp. 242-245, 10.1111/jth.13584
14- Klima DA, Snyder TE. Postpartum ovarian vein thrombosis. Obstet Gynecol. 2008;111(2):431–5.
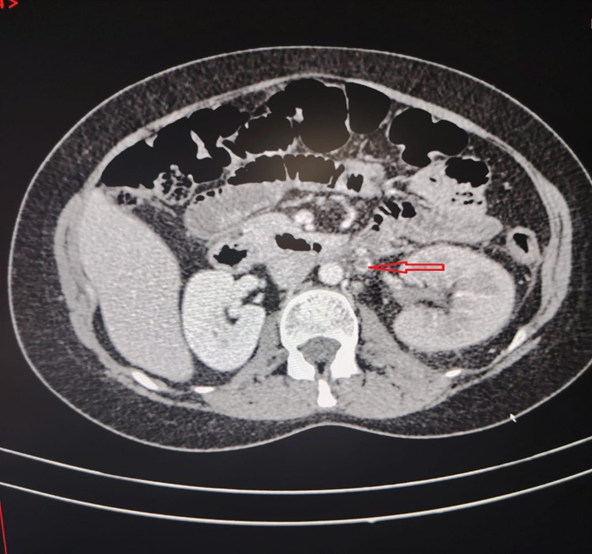
Figure 1
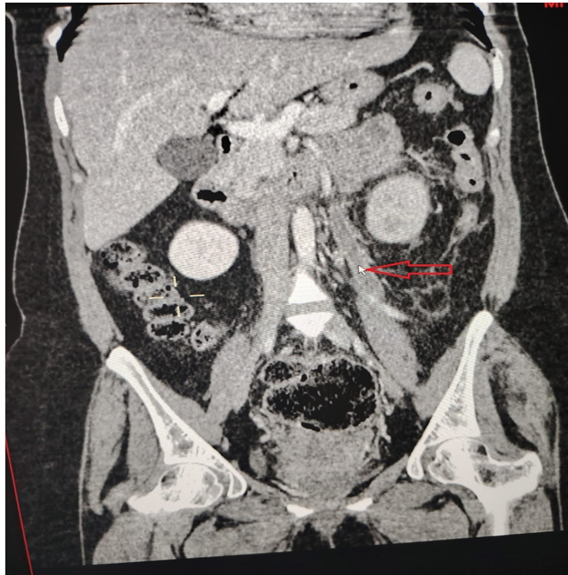
Figure 2
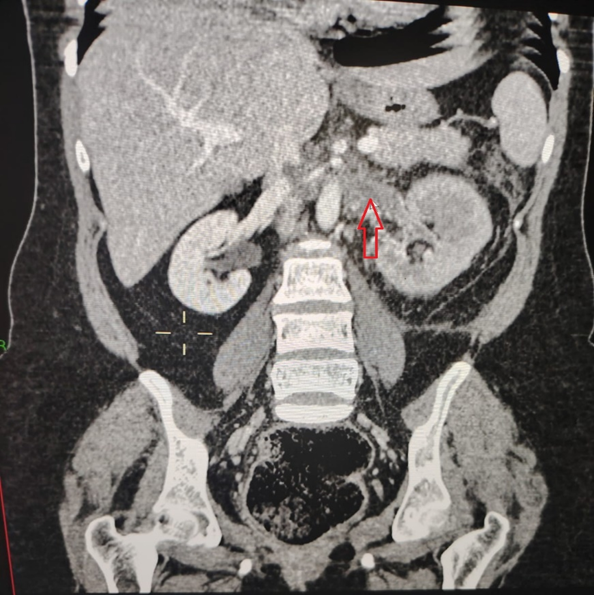
Figure 3
