Thyroid Function Assessment in Neonates Born to Mothers with Thyroid Dysfunction during Pregnancy
Thyroid Function Assessment in Neonates Born to Mothers with Thyroid Dysfunction during Pregnancy
Dr. Keerthana P Bhandary *1, Dr. Edwin Dias 2 , MD, DCH, DNB , Dr. Apsara M Nambiar3
1. Junior resident, Department of Paediatrics, Srinivas Institute of Medical Sciences and Research Centre, Mangalore
2.Professor and HOD, Department of Paediatrics, SIMS&RC , Mangalore , Director of Research and Publication , SIMS&RC , Mangalore , Research Professor , Srinivas University
3. Intern, Srinivas Institute of Medical sciences and Research Centre, Mangalore.
Correspondence to: Dr. Keerthana P Bhandary, Junior resident, Department of Paediatrics, Srinivas Institute of Medical Sciences and Research Centre, Mangalore.
Copyright
© 2024: Dr. Keerthana P Bhandary. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 30 Aug 2024
Published: 24 Oct 2024
Abstract
INTRODUCTION: Maternal thyroid disease is considered as risk factor for abnormal thyroid function at birth. The potential adverse impact of maternal hypothyroidism and hyperthyroidism, even when subclinical, on neurodevelopmental outcome in the new born is noted. Hence this study is taken up to determine the influence of maternal thyroid dysfunction in the new-borns. The potential harmful effects on the neonate had led to the clinical practice of thyroid function assessment in infants born to mothers with thyroid disease during pregnancy1. Grave's disease activity in women of childbearing age should be well controlled prior to conception4. Cardiac insufficiency is a major morbidity in neonatal hyperthyroidism. It is important to assess the hemodynamics in neonates born to mothers with Graves' disease (GD). This study prospectively evaluated the hemodynamic changes in neonates born to mothers with GD6. In the instances of transient neonatal hypothyroidsim due to a maternal TBIAb, the IgG has been of unusually high potency in the TBI assays (4,5,14)7.
OBJECTIVES: To assess thyroid dysfunction in neonates born to mothers with elevated TSH values and low fT4.
MATERIALS AND METHODS: Data was collected retrospectively from medical records All mothers diagnosed with thyroid disorders were included in the study. 50 mother-neonate pair of were investigated for TSH and fT4 between 48 and 72 hours of life( to avoid TSH surge) in a tertiary care centre between March 2022 and January 2023.
RESULTS: Among 50 new-borns, the prevalence of thyroid disorders in mothers with low fT4 and infants with low fT4 is 4 (8 %). 3(6%) were diagnosed to have congenital hypothyroidism , and 2(4%) were diagnosed to be hyperthyroid. Subclinical hypothyroidism (elevated TSH and normal ft4 ) was 9 (18%) which was the most common thyroid disorder observed. Most commonly observed foetal birth weight in this study were between 3-3.5kgs 20(40 %). Out of all thyroid disorders associated with pregnancy, subclinical hypothyroidism is the most frequently noted.
CONCLUSION: Subclinical hypothyroidism was noted in 18% of the study group. Women with thyroid dysfunction must be monitored throughout pregnancy, and also their new born infants should be closely followed in 1st month of postnatal life for thyroid disorder.
Thyroid Function Assessment in Neonates Born to Mothers with Thyroid Dysfunction during Pregnancy
Introduction
Maternal thyroid diseases are considered a risk factor for abnormal thyroid function at birth as well as long term morbidity in the offspring. [1] Thyroid hormones are important for energy metabolism, metabolism of nutrients, thermogenesis and stimulation of growth and development.
Maternal hyperthyroidism and hypothyroidism both affect foetal and neonatal thyroid. [1] Maternal hyperthyroidism during pregnancy is associated with an increased risk of low birth weight and neonatal hyperthyroidism causes goitre, poor weight gain and thrombocytopenia. [2] Maternal high-normal fT4 levels, in early pregnancy is associated with lower birth weight and increased risk for SGA newborns. Deficiency of thyroid hormones lead to mental retardation, jaundice, and lethargy. Congenital hypothyroidism is the most frequent cause of preventable mental retardation causing impaired psychomotor and intellectual development of the child , and all efforts to sustain prevention must be adhered to.
The most common cause of hypothyroidism during gestation is autoimmune thyroiditis, characterised by presence of specific thyroid autoantibodies, whereas hyperthyroidism is causes by Graves disease. A number of infants born to mothers with GD had abnormal TFTs requiring specific management, and some of them had abnormal growth and development. Careful evaluation of TFTs and long-term follow-up are mandatory for those children3. Antithyroid drugs such as propylthiouracil and methimazole in the pregnant mother are additional causes of transient hypothyroidism in the newborn. Maternal subclinical hypothyroidism has shown to cause adverse obstetric outcomes and neuro-intellectual impairment in child. These observations have led to recommendation on maintaining TSH values in pregnant woman below 2.5mU/L.
In most Western countries, newborn thyroid function screening is standard and its main purpose is to identify and initiate early supplemental thyroxine therapy in infants with congenital hypothyroidism. The potential effects of maternal thyroid disease on offspring have led to practice of recommending serum TFT in newborns at 2-3 days after birth owing to the TSH surges which soon occurs after birth giving high false positive results.
Therefore this study was carried out in Srinivas Hospital, in infants of age 2-3 days born to mothers with diagnosis of thyroid diseases. In this study, we retrospectively evaluated the TFT results and the complications in neonates born to mothers with thyroid dysfunction.
Aim and Objectives
AIM: To assess thyroid dysfunction in neonates born to mothers with thyroid dysfunction between 48-72 hours of life using TSH and fT4
OBJECTIVES: To study early neonatal complications like pathological jaundice, sepsis, congenital anomaly, diarrhoea and neonatal hypothyroidism
To study the correlation between birth weight and thyroid disorders.
Materials and Methods
This retrospective study was carried out from March 2022 to January 2023 at the Department of Paediatrics, Srinivas Hospital, Mukka, Mangalore. The study was conducted on all neonates born to mothers with thyroid dysfunction, satisfying both the inclusion and exclusion criteria. 50 mother-neonate pairs were selected for the study.
The diagnosis of maternal thyroid dysfunction based on TSH and fT4 levels were made.
INCLUSION CRITERIA:
• Hypothyroid mother
• Hyperthyroid mother
• Neonates born to hypothyroid and hyperthyroid mother
• TSH and fT4 measured between 48-72 hours of life
EXCLUSION CRITERIA:
• Mothers with no thyroid dysfunction
• TSH and fT4 measured below 48 hours and beyond 72 hours of life
After obtaining informed written consent from parents, neonates were tested for TSH and fT4 between 48-72 hours of life by venous blood testing.
Infant demographic and clinical data including gestational age, birth weight, sex , delivery route were recorded.
• Hypothyroidism: TSH >20uI/ml and fT4 <2ng/dl
• Hyperthyroidism: TSH <20uI/ml and fT4 >2ng/dl
• Subclinical Hypothyroidism: TSH is >20uIU/L and fT4 is 2-5ng/dl
Results and Analysis
• 50 babies under the inclusion criteria were screened.
• Among 50 newborns, the prevalence of thyroid disorders in mothers with elevated TSH and low fT4 and infants with low fT4 is 4(8%)-CONGENITAL HYPOTHYROIDISM
• Prevalence of thyroid disorders in mothers with low TSH and elevated fT4 with infants with elevated fT4 is 2 (4%)- HYPERTHYROIDISM
• Subclinical hypothyroidism (elevated TSH and normal fT4) was 9 (18%) which was the most common thyroid disorder observed.
• In the present study , the incidence of neonatal complication found in Subclinical hypothyroid was Pathological jaundice (29%), sepsis (43%), diarrhoea(29%) and no other complications found.
• Among overt hypothyroid mother, out of 3 cases, only 1 had pathological jaundice and other had diarrhoea.
• Most of the neonates born weighed between 3-3.5kg (20), and were born to hypothyroid mothers.
• Neonates born to hyperthyroid mother weighed between 2-2.5kg (2).
• Babies born to hypothyroid mothers were mostly AGA and LGA, but babies born to hyperthyroid mothers were termed as SGA.
Figure 1
Figure 2
Figure 3
Discussion
• In the present study, out of 50 mother-neonate pairs, only 12% were diagnosed to have congenital hypothyroidism and 6% were diagnosed to be hyperthyroid. Subclinical hypothyroidism (elevated TSH and normal fT4) was 18% which was the most common thyroid disorder observed.
• Similar study conducted by Luton et al showed 10% cases of congenital hypothyroidism and 6% cases of hyperthyroidism.
• Similar study conducted by Anderson et al, showed low birth weight in hyperthyroid mothers and higher birth weight in hypothyroid mothers.
• Mean maternal anti-TPO titers were significantly higher in infants with positive titers compared to infants with negative titers2.
Conclusion
• Thyroid hormones are required for various metabolic functions as well as myelination of brain, deficiency of thyroid hormones during critical period of development results in severe irreversible mental retardation.
• Congenital hypothyroidism is an important preventable cause of mental retardation. Patients with subclinical hypothyroidism remain asymptomatic but have bad neonatal outcome,
• In this context, screening for congenital hypothyroidism is the best and the least expensive solution for prevention.
•Duration of maternal Graves disease or thyrotoxicosis, either mild chemical or overt, in pregnancy is significantly associated with SGA neonates. Neonatal thyroid dysfunction is associated with the maternal thyroid condition, especially the serum TSH-receptor antibody level5.
References
1. Ben-Zeev ZS, Peniakov M, Felszer C, Weiner SA, Lahad A, Almashanu S, Tenenbaum Rakover Y. Usefulness of thyroid function assessment in infants born to mothers with thyroid dysfunction during pregnancy. Eur Thyroid J. 2022 Jun 23;11(4):e220055. doi: 10.1530/ETJ-22-0055. PMID: 35613337; PMCID: PMC9254317.
2. Ozdemir H, Akman I, Coskun S, Demirel U, Turan S, Bereket A, Bilgen H, Ozek E. Maternal thyroid dysfunction and neonatal thyroid problems. Int J Endocrinol. 2013;2013:987843. doi: 10.1155/2013/987843. Epub 2013 Apr 30. PMID: 23737782; PMCID: PMC3657451.
3. Sakornyutthadej N, Mahachoklertwattana P, Poomthavorn P. Thyroid function and long-term outcomes of children born to mothers with Graves' disease: A 20-year review. J Paediatr Child Health. 2023 Mar;59(3):526-532. doi: 10.1111/jpc.16343. Epub 2023 Feb 1. PMID: 36722797.
4. Uenaka M, Tanimura K, Tairaku S, Morioka I, Ebina Y, Yamada H. Risk factors for neonatal thyroid dysfunction in pregnancies complicated by Graves' disease. Eur J Obstet Gynecol Reprod Biol. 2014 Jun;177:89-93. doi: 10.1016/j.ejogrb.2014.03.007. Epub 2014 Mar 21. PMID: 24726178.
5. Mitsuda N, Tamaki H, Amino N, Hosono T, Miyai K, Tanizawa O. Risk factors for developmental disorders in infants born to women with Graves disease. Obstet Gynecol. 1992 Sep;80(3 Pt 1):359-64. PMID: 1379702.
6. Ishikawa T, Uchiyama H, Iwashima S, Baba T, Ohishi A, Iijima S, Itoh H. Hemodynamic changes in neonates born to mothers with Graves' disease. Endocrine. 2021 Apr;72(1):171-178. doi: 10.1007/s12020-020-02443-w. Epub 2020 Aug 12. PMID: 32785898.
7. 1.McKENZIE JM, ZAKARIJA M. Fetal and Neonatal Hyperthyroidism and Hypothyroidism due to Maternal TSH Receptor Antibodies. Thyroid. 1992 Jan;2(2):155–9.
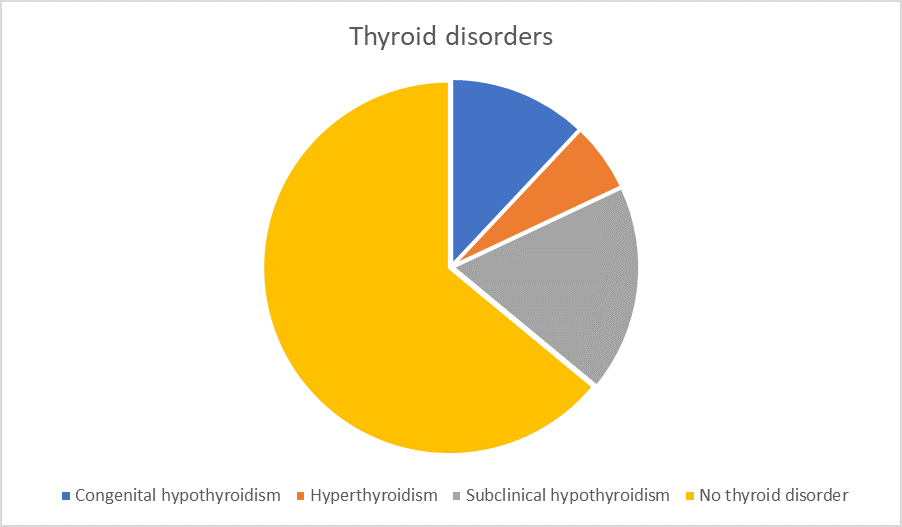
Figure 1
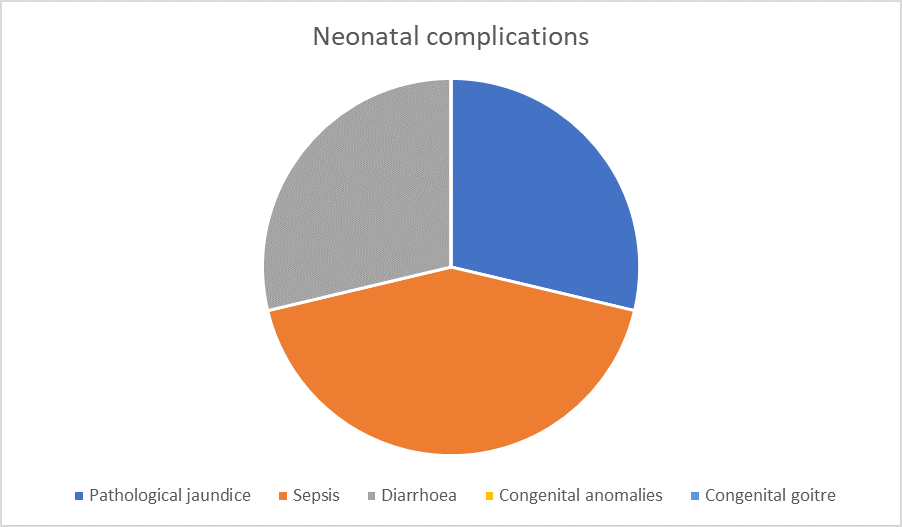
Figure 2
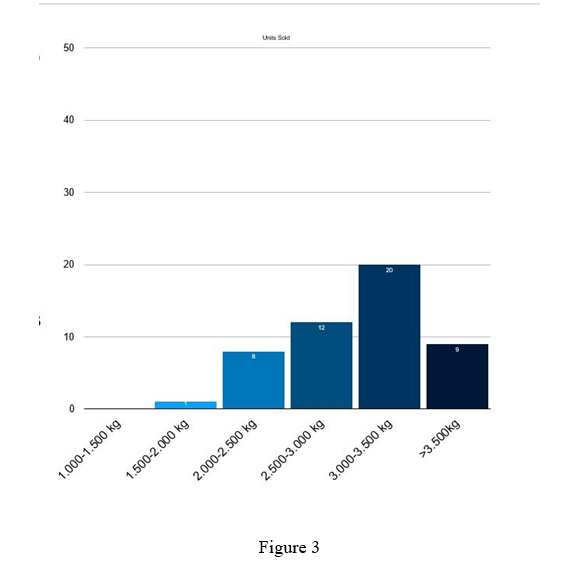
Figure 3
