Different Presentations of Scar Rupture in Labour - A Case Report
Different Presentations of Scar Rupture in Labour - A Case Report
Dr.Surbhi Sharma *, Dr. Manoj Chandrasiri1
1.Dr Manoj Chandrasiri Consultant Obstetrician and Gynaecologist, Wrexham Moelar hospital, Wrexham ,UK
*Correspondence to Dr.Surbhi Sharma registrar, MD, MRCOG.
Copyright
© 2024 Dr. Surbhi Sharma. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 15 October 2024
Published: 24 October 2024
DOI: https://doi.org/10.5281/zenodo.14044614
Abstract
Background: Uterine rupture is a rare event. Most cases of rupture happen in scarred uterus while in labour and can cause catastrophic outcome for mother and baby.
Case report : A case of a woman, 38 weeks gestation who had a previous caesarean delivery keen to have vaginal birth this time, had regular antenatal care and then had induction of labour. During labour she did not have typical symptoms or signs of scar rupture except cardiotocographic changes (CTG) needing emergency caesarean delivery. The second case is of a lady at 36 weeks gestation presenting with abdominal pain with 2 previous caesarean sections and no typical symptoms or signs of it except continuous abdominal pain and needing a caesarean delivery and finding of scar rupture intraoperatively.
Conclusion: Uterine rupture can occur in any woman scared or unscarred uterus, however heightened clinical awareness is essential for women with a history of uterine scarring, particularly during labour where it may sometimes be asymptomatic. With increasing cesarean section rates and many woman opting for vaginal birth after caesarean section (VBAC). Hence careful selection of cases for trial of scar and counseling should take place in antenatal period and then planning for induction of labour and augmentation in labour.
KEYWORDS : Uterine rupture ,VBAC,CTG.
Different Presentations of Scar Rupture in Labour - A Case Report
Introduction
Uterine rupture is a rare event, occurring in just 2 per 10 000 pregnancies (UKOSS)1. However, when it does occur it frequently results in life threatening maternal and/or fetal compromise. A study showed 87% of uterine ruptures occurred in women who had a uterine scar, with just 13% occurring in women with an unscarred uterus (2).
Case Reports
Case 1)
A 29-year-old lady was booked into second pregnancy at 16 weeks for consultant led care. She was G3p1+1, had a previous caesarean section at 37 wks for failed induction of labour, about 20 months ago. She was offered serial ultrasound scans in view of previous baby being on 5th centile. She also attended birth choices clinic to discuss her birth choices. She was keen for vaginal birth after caesarean section (VBAC) and had regular antenatal care. She developed gestational diabetics (GDM) at 28 weeks gestation and was commenced on metformin.
She opted for a VBAC and had appropriate counselling including a discussion of benefits, risks and the likelihood of a successful VBAC. She was also given option of having elective caesarean section.
She had serial growth scans and diabetic team reviews and was offered induction of labour (IOL) at 38 weeks gestation for above risk factors and recurrent reduce movements.
She was induced with a balloon catheter followed by artificial rupture of membranes (ARM) on labour ward and she was 2 cm on per vaginal examination. She was commenced on continuous cardiotocography (CTG) . She made progress until 4 cm and decided to go for epidural for pain relief. After further 6 hours, as there was no progress in labour and she was still 4 cm on vaginal assessment and having irregular contractions, she was assessed by doctor and offered oxytocin drip for augmentation of labour. Later on, there was sudden onset fetal bradycardia which continued 5 minutes with no signs of recovery. The vaginal examination revealed that she was 8 cm dilated with a high presenting part and decision for category 1 caesarean was made. Maternal observations remained normal throughout labour.
During the caesarean section upon entering the peritoneal cavity, there was hemoperitoneum and the baby was seen extruded in the abdominal cavity. Baby was pale, floppy on delivery. APGAR score at birth was 4 at 1 min and 8 at 5 min. There was a rupture along the left lateral uterine wall extending laterally to pelvic side walls and inferiorly. It was repaired but due to close proximity to the ureter, urologist was called for help and was aided in ureterolysis before the surgeon could repair the uterine tear, which was also preceded by a cystoscopy.
She had a total blood loss of 1.5 liters. She received inpatient care for 5 days needing two blood transfusions as her haemoglobin was 78 g/l post operatively and subsequently discharged with hemoglobin of 89g and on ferrous sulphate.
Both the woman and newborn were discharged home in good condition on postoperative day 5. She was debriefed and advised about future pregnancy to have elective caesarean section at 37 wks -38 wks of gestation.
Case Report 2
A 29 yr old woman booked into her fourth pregnancy, G4p3 ,1st pregnancy was a term vaginal delivery followed by emergency caesarean section 9 years ago followed by another elective LSCS 4 years ago.
She was booked under consultant led care due to history of mental health issues and also previous two caesarean sections. She presented with sharp lower abdomen pain at 36 weeks of gestation and despite analgesics like paracetamol and codeine phosphate the pain did not improve. No signs of uterine activity on clinical examination or on CTG. Urine dipstick was normal and all her observations were normal. There was no scar tenderness and on speculum examination cervical os was closed and actin partus was negative. Later she was reviewed again due to increasing pain and was offered stronger pain relief after thorough assessment.
She was subsequently transferred to labour ward for one to one care with continuous CTG monitoring due to ongoing concerns. In view of constant abdominal pain, decision was taken for a category 1 emergency LSCS. The intraoperative findings of a uterine rupture was confirmed with amniotic fluid in peritoneal cavity seen and the fetal head was also seen through uterine rupture. There was a small extension of uterine rupture to the inferior segment. It was repaired and baby was born in good condition. Total blood loss was 450ml and patient had an uneventful recovery..
Discussion
Characteristic signs and symptoms of uterine rupture include abdominal pain of a tearing quality, abnormal fetal heart rate, vaginal bleeding, sudden loss of contractions, and loss of the presenting part.
These signs are not always present, and the presentation of a uterine rupture is often non-specific (3,4.5). The fetal heart rate provides an insight into both the health of the fetus and the health of the woman. Fetal bradycardia is the most common abnormality associated with uterine rupture though no fetal heart rate tracing is pathognomonic for uterine rupture.
Absence of fetal heart sounds is obviously an ominous sign and requires an ultrasound to confirm absent cardiac activity. Uterine rupture is difficult to diagnose. Diagnostic imaging methods such as CT and MRI and ultrasound are of limited use due to delay in establishing the diagnosis.
The incidence of serious fetal and maternal morbidity depends upon the location and magnitude of the rupture and the speed of surgical intervention. Lateral ruptures are associated with worse outcomes than midline ruptures due to increase vascularity (3,4,5). Rupture of unscarred uterus is associated with more blood loss, a higher incidence of hysterectomy, and a higher rate of composite maternal morbidity (death, hysterectomy, blood transfusion, or urologic injury) than rupture of scarred uteri. A longer time to surgical intervention is associated with excess maternal blood loss, a higher risk of coagulopathy, and longer fetal exposure to hypoxia hence, fetal mortality of 2%(scarred uterus) ,which is fivefold higher in unscarred uterine rupture .The incidence of composite fetal neurologic injury (intraventricular hemorrhage, seizure, death, or brain ischemia) is also higher for ruptures involving an unscarred uteri, compared to scarred uteri.
In the first case, there were no symptoms of scar pain or constant pain or abnormal contour of uterus as all masked by a good working epidural nor we saw any signs of hemodynamic instability in the woman or vaginal bleeding which could suspect a uterine rupture. We could only detect CTG (figure 1) changes which was of bradycardia .It involve quick decision and category 1 LSCS was called for to prevent hypoxic damage to baby .In theatre, multi-disciplinary team(MDT)approach was taken on detection of tear closer to lateral wall of uterus and involvement of senior obstetrician and urologist. In the second case, as there were no acute signs of scar rupture evident on clinical examination of abdomen or CTG (figure 2 and 3) ,decision for delivery was difficult as we had to weigh the risk of prematurity. Throughout the assessment she had normal observations and CTG trace .
Hence, clinical judgment in cases is to be taken on case-to-case basis as there are no fixed pattern of presentation for atypical scar ruptures. We have to remain vigilant for signs and symptoms of it in any woman with a uterine scar in antenatal or intrapartum period and also in post natal period as some case reports of detection of scar rupture are reported after successful VBAC
.
Figure 1, Figure 2., Figure 3
Conclusion
Spontaneous rupture can occur in women without any alarming symptom and classical signs of rupture are not always present.
Hence, a high index of suspicion is the key to early diagnosis of uterine rupture in case of previous scar when they present with vague symptoms at any gestation. Prompt recognition of potential uterine rupture and immediate laparotomy lowers the rate of perinatal death. The diagnosis of uterine rupture is often confirmed when hemoperitoneum and fetal parts are identified during laparotomy.
Fetal bradycardia is the most common abnormality associated with uterine rupture. No fetal heart rate tracing pattern is pathognomonic for uterine rupture (7,8,9). The absence of fetal heart sounds is obviously an ominous sign and requires an ultrasound to confirm absent fetal cardiac activity. One has to be cautious when using IOL agents e.g., prostaglandins or oxytocin for augmentation in labor. Hence high suspicion of scar rupture and prompt management helps to avoid poor outcome for baby and mum.
References
1.Gynecol Obstet. 2005 Sep;272(3):229-31. [PubMed] https://www.npeu.ox.ac.uk/ukoss/completed-surveillance/ur
2. https://www.barnsleyhospital.nhs.uk/sites/default/files/2023-07/uterine-rupture.pdf
3.Gibbins KJ, Weber T, Holmgren CM, Porter TF, Varner MW, Manuck TA. Maternal and fetal morbidity associated with uterine rupture of the unscarred uterus. Am J Obstet Gynecol. 2015 Sep;213(3):382.e1-6. [PubMed]
4. Guiliano M, Closset E, Therby D, LeGoueff F, Deruelle P, Subtil D. Signs, symptoms and complications of complete and partial uterine ruptures during pregnancy and delivery. Eur J Obstet Gynecol Reprod Biol. 2014 Aug;179:130-4. [PubMed]
5 ACOG Practice Bulletin No. 205: Vaginal Birth After Cesarean Delivery. Obstet Gynecol. 2019 Feb;133(2):e110-e127. [PubMed]
6 Ozdemir I, Yucel N, Yucel O. Rupture of the pregnant uterus: a 9-year review. Arch
7. Miller DA, Goodwin TM, Gherman RB, Paul RH. Intrapartum rupture of the unscarred uterus. Obstet Gynecol 1997;89:671–3.
8. Revicky V, Muralidhar A, Mukhopadhyay S, Mahmood T. A case series of uterine rupture: lessons to be learned for future clinical practice. J Obstet Gynaecol India 2012;62:665–73.
9. Ripley DL. Uterine emergencies. Obstet Gynecol Clin North Am 1999;26(3):419–34. 6. Zwart JJ, Richters JM, Ory F, de Vries JIP, Bloemenkamp KWM, van Roosmalen J. Uterine rupture in the Netherlands: a nationwide population-based cohort study. BJOG 2009;116(8):1069–80.
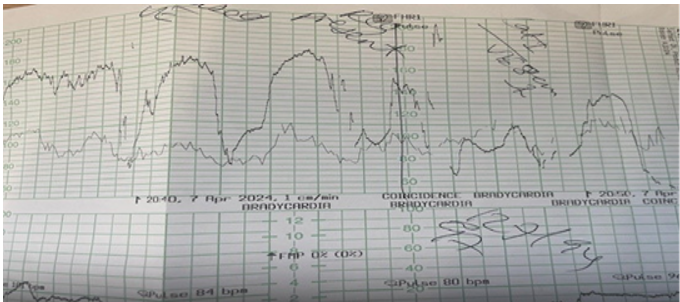
Figure 1
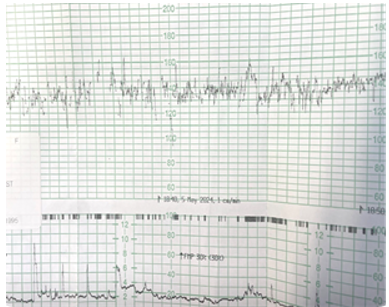
Figure 2
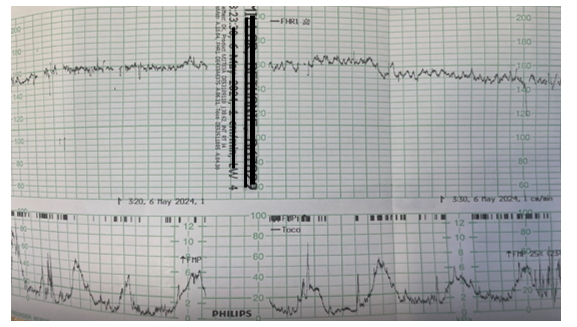
Figure 3
