A Brain Abscess in a Neonate: A Case report
A Brain Abscess in a Neonate: A Case report
Dr.Abdul Rahim H. Zwayed *1, Dr.Enas Hasan2, Dr.Amir Mustafa 3, Dr. Faisal K. Al Balushi 4, Dr. Mamdouh M.5, Dr. Hetal A. Bhai 6, Dr.Yasser A Raziek 7, Dr.Reem M. Ibrahim 8, Dr. Halima M.Al Amri 9, Moza Al Maamari 10, Dr.Ban F. Refaat 11, Dr.Yaqoob Al Saidi 12
1. M.B.Ch.B.,PhD. Department of Neurosurgery.
2, 12. Neurosurgeon.
3, 4, 5, 6. Anesthesia.
7, 8, 9. Radiology
10,11. Paediatrics.
Sohar Hospital, Sultanate of Oman.
*Correspondence to: Abdul Rahim H. Zwayed, M.B.Ch.B., PhD., Department of Neurosurgery. Sohar hospital –Sultanate of Oman.
Copyright
© 2024 Abdul Rahim H. Zwayed, This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 25 Sept 2024
Published: 24 Oct 2024
DOI: https://doi.org/10.5281/zenodo.14044720
A Brain Abscess in a Neonate: A Case report
Introduction
Brain abscesses occur at any age and most common cause is a complication of bacterial meningitis, but occur in a neonate of less than one moth of age with no clear history of meningitis is something unique.
Here we report a case of 28 days age presented with fever and convulsion and excessive cry, refusal to feed, and vomiting.
CT scan and Magnetic resonance imaging (MRI) with contrast studies revealed intra-parenchymal brain abscess in the left frontal region with ring enhancement and midline shift.
Craniotomy done as left frontal flap with evacuation of thick purulent material, then coverage of antibiotics for about 6 weeks according to culture and sensitivity
A complete resolution of the abscess occurs but the patient developed hydrocephalus where later on a ventriculo-peritoneal shunt done.
The patient was discharged after the documentation of radiological clearance in repeat MRI study.
No complications were recorded. An appropriate neuro-developmental outcome was observed on follow-up.
Keywords: Brain Abscess, neonate
The Case
This female near term baby was born by spontaneous vaginal delivery, with birth weight 2.3kg baby. Scan was normal, She was discharged after 24 hours and was normal till the age of 4 weeks where she was presented to the Emergency Paediatric Unit with history of 2 days fever documented at 38.5 as per father, associated with excessive cry, refusal to feed, seizures, and vomiting
Neurological examination revealed normal occipito-frontal circumference, wakefulness, reflexes and physiological hypotonia without a focal neurological deficit but bulging anterior fontanelle.
Examination of other systems was normal.
Laboratory investigations showed a positive sepsis screen:
Blood picture and biochemistry was as:
Total leukocyte count = 14.200 c/mm,
Absolute neutrophil count = 9.400/μl,
Serum C-reactive protein = 2.6 mg/dl.
Normal chest X-ray and an arterial blood gas.
Blood culture sent earlier was sterile.
The cerebrospinal fluid examination was normal with sterile culture and with no micro-organisms seen in the Gram-stained slide thus, indicating the absence of meningitis.
Due to the persistent clinical features of sepsis, antibiotics were started as intravenous Meropenem .
The persistence of fever and tense fontanelle shallow & irregular breathing pattern prompted us for cranial ultrasonograms which revealed hypo-echoic lesion in left frontal lobe.
CT /and Magnetic resonance imaging (MRI) brain with contrast was subsequently performed which showed hypo-dense lesion with peripheral enhancement suggestive of intra-parenchymal abscess in left frontal
Figure 1 ?. Head CT: showed a large left frontal hypodense cystic like lesion about 3.5x3.5 cm with density about (13 hu) causing compression of the left lateral ventricle anterior horn with midline shift to the right anteriorly about 3-4 mm with surrounding minimal oedematose changes in both frontal lobes
Figure 2: MRI brain images: There is left frontal intra axial complex cystic lesion 3.5x3.7x3.9 & thin smooth rim of peripheral enhancement ,internal thin enhancing septation fluid-fluid level and debris causing mass effect on adjacent frontal horn with mild midline shift 3mm to the right ,no direct connection seen with the left frontal horn
Figure 3 – The operation as left frontal craniotomy
An urgent operation done as left frontal craniotomy
Dural incision, brain was tense with gray to bluish discoloration
Small cortical incision at frontal lobe done, then evacuation of the abscess by aspiration totally (send for culture and sensitivity), washing the area with normal saline and diluted Gentamicin, haemostasis,, wounds closed in layers, drain left in situ for about 72 hours and removed where no more drainage appeared.
Aspirated fluid (purulent greenish material) culture and sensitivity showed: bacterial growth detected gram negative called:
(Citrobacter Sedlakii) which is as such:
|
Amoxicillin + Clavulan |
Resistant |
|
Ceftazidime |
Resistant |
|
Cefuroxime |
Resistant |
|
Ciprofloxacin |
Sensitive |
|
Gentamicin |
Resistant |
|
Imipenem |
Sensitive |
|
Meropenem |
Sensitive |
|
Piperacillin +Tazobactam |
Sensitive |
|
Trimethoprim +Sulfame |
Sensitive |
|
Ampicillin |
Resistant |
The patient was kept on intravenous anti biotics as Meropenem for about 6 weeks.
CT/MRI repeated (after completion the course of antibiotics) revealed no abscess but newly developed hydrocephalus.
Figure 4: MRI brain (post-operative craniotomy) in comparison with previous scans, there is complete resolution of the previously seen left frontal abscess collection with no residual or new collection, only mild post-operative gliosis, focal meningeal enhancement and haemosiderin rim seen.
There is dilatation of the lateral and third ventricles maximum diameter 26 mm of the right lateral ventricle at atrium with more dilatation of the left frontal horn.
Then again cerebrospinal fluid CSF study was done: which was clear and sterile so operation done as ventriculo peritoneal shunt (VPS).The patient stayed in the hospital after shunt operation for 7 days ,then discharged and advice for follow up in the neurosurgical outpatient clinic or consult on need to the emergency.
Follow up with no complication noted
Improvement in general condition was observed in the ensuing time. The baby had a normal neurological examination and developmental milestones at 9 months of age.
Discussion
Brain abscesses occur as an uncommon complication of bacterial meningitis in 1.3–4.0% neonates.[11]
Gram-negative micro-organisms commonly Citrobacter diversus, Proteus and Pseudomonas species have been implicated in the pathogenesis as they bear the propensity to invade nervous tissue and cause necrotizing vasculitis.[2]
Klebsiella pneumoniae was isolated in the cited case of brain abscess. Although, Klebsiella is the most common organism causing neonatal sepsis in developing countries [3], it has been reported in few cases of brain abscess in the world literature.[4,5] However, in one of the largest series of 30 neonates with brain abscess in a tertiary center, no case was attributed to Klebsiella species.[6] This could be due to its lesser tendency to cause necrotizing lesions as compared to Citrobacter and Proteus species.[1].
Volpe has emphasized that the bacteria cause meningitis and vasculitis initially, which may further, rarely complicate and result in the formation of a brain abscess.[15]
In this case, there was history of acute respiratory infection of the mother for 3 days prior to delivery which was probably followed by neonatal sepsis and haematogenous seeding of the brain parenchyma resulting in this abscess with no initial meningeal involvement.
Sundaram et al. have hypothesized that the direct hematogenous seeding of the parenchyma could be an equally important pathogenetic mechanism for an abscess to develop and a meningeal involvement may not be an essential prerequisite always.[14]
The colonization of brain parenchyma during sepsis can be explained by the physiological right-to-left shunt of the neonatal circulation.[8].
The usual clinical presentation of brain abscess in neonatal period consists of irritability, bulging fontanelle, and rapid rise in head circumference with wide separation of sutures, vomiting, seizures, and poor feeding.[13] This case was characterized by the absence of the usual clinical features as mentioned. The presence and persistence of fever, convulsion, refusal to feed and vomiting necessitated a cranial ultrasonography and MRI brain.(12)
The management of neonatal brain abscess is influenced not only by the anatomic location, size, stage, and nature of the abscesses but also by the age and neurological status of the patient.[3] Medical management usually started once patient has clear picture of infection and may save the patient from surgical complications especially in a neonate, who may present with significant surgery-related neurological deficits and hemorrhage.[1] The duration of the antibiotic course is usually 6–8 weeks and longer for immunocompromised patients.[10]
In this case, Meropenem penetrates the blood-brain barrier well when the meninges are inflamed and achieves an excellent minimum inhibitory concentration for almost all Gram-negative pathogens [5] but neonatal data about its penetrative ability in the absence of meningeal inflammation or within an abscess cavity are lacking.
On the other hand, surgical intervention provides samples for accurate diagnosis, reduces the mass of an abscess, improves the efficacy of the drugs used for treatment and in some conditions allows intrathecal, intra-ventricular or intra-cavitory administration of antibiotics.[2]
Abscess more than 2.5 cm of size requires neuro-surgical drainage.[7]
The long-term outcome of a neonatal brain abscess is not very encouraging. Various studies have highlighted the poor IQ scores and subsequent poor scholastic performance.[4] In this case, the patient exhibited appropriate developmental milestones on follow-up.
To conclude: brain abscesses may not be preceded by meningitis in all neonates. Apart from the typical features, a clinician should be aware of atypical features such as shallow and irregular breathing, inability to maintain oxygen saturation in room air, and absence of the usual clinical features. (6)
A strong clinical suspicion is required for the diagnosis especially in cases with atypical presentation.
Brain abscess in newborns is a very rare disease. It is a focal, intracerebral infection that begins as a localized area of cerebritis and develops into a collection of pus surrounded by a well-vascularized capsule. Early capsulation is seen in 10–13 days. (9)
Conclusion
Diagnosis of brain abscess is usually by clinical and radiology usually requires specific CT study, which is the modality of choice as MRI does not much differ in the diagnosis of brain abscess and cranial ultrasound that has been proved to be helpful in the diagnosis and surgical option is usually the best solution.
Reference
1. Basu S, Mukherjee KK, Poddar B. An unusual case of neonatal brain abscess following Klebsiella pneumoniae septicemia. Infection. 2001;29:283–5.
2. De Oliveira RS, Pinho VF, Madureira JF, . Brain abscess in a neonate: An unusual presentation. Childs Nerv Syst. 2007;23:139–42.
3. Francis BM, Gilbert GL. Survey of neonatal meningitis in Australia: 1987-1989. Med J Aust. 1992;156:240–3.
4. Feferbaum R, Diniz EM, Valente M., et al. Brain abscess by Citrobacter diversus in infancy: Case report. Arq Neuropsiquiatr. 2000;58:736–40.
5. Frazier JL, Ahn ES, Jallo GI. Management of brain abscesses in children. Neurosurg Focus. 2008;24:E8.
6. Gormley WB, del Busob R, Saravolat LD. Cranial and intracranial infections. In: Youman JR, editor. Neurological Surgery. 4th ed. Philadelphia: WB Saunders Publishers; 1996. pp. 3191–220.
7. Garfield J. Management of supratentorial intracranial abscess: A review of 200 cases. Br Med J. 1969; 2:7–11.
8. Gruber WC, Fisher RG. Miscellaneous bacterial infections. In: Feigin RD, editor. Textbook of Pediatric Infectious Diseases. 4th ed. Philadelphia: Saunders; 1994. pp. 1363–5.
9. Hakan T. Management of bacterial brain abscesses. Neurosurg Focus. 2008;24:E4.
10.Hinsdale G. Purulent encephalitis and cerebral abscess in the newborn due to infection through the umbilicus. Am J Med Sci. 1899; 118:280–3.
11.Lu CH, Chang WN, Lui CC. Strategies for the management of bacterial brain abscess. J Clin Neurosci. 2006; 13:979–85.
12. Nau R, Lassek C, Kinzig-Schippers M. Disposition and elimination of meropenem in cerebrospinal fluid of hydrocephalic patients with external ventriculostomy. Antimicrob Agents Chemother. 1998; 42:2012–6.
13. Renier D, Flandin C, Hirsch E. Brain abscesses in neonates. A study of 30 cases. J Neurosurg. 1988; 69:877–82.
14. Sundaram V, Agrawal S, Chacham S, Dutta S, Kumar P. Klebsiella pneumoniae brain abscess in neonates: A report of 2 cases. J Child Neurol. 2010;25:379–82.
15. Volpe JJ, editor. Neurology of the Newborn. 5th ed. Philadelphia, PA: Saunders, an Imprint of Elsevier Inc; 2008. Bacterial and fungal intracranial infections; pp. 916–56.
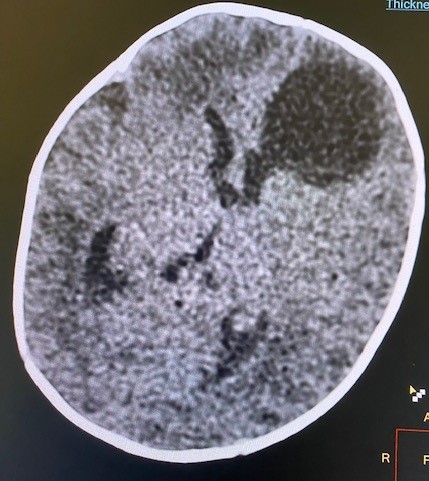
Figure 1
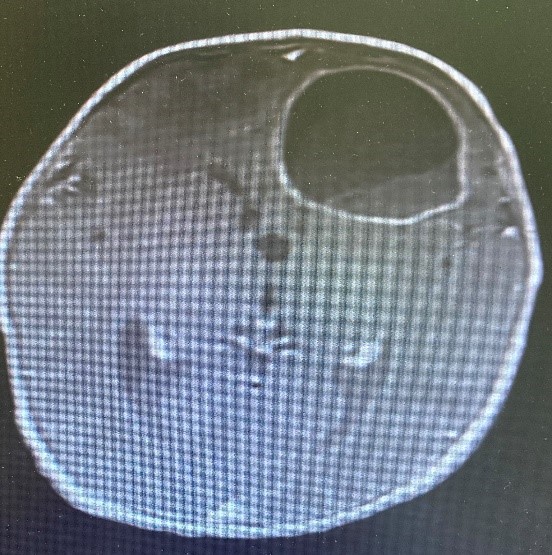
Figure 2

Figure 3
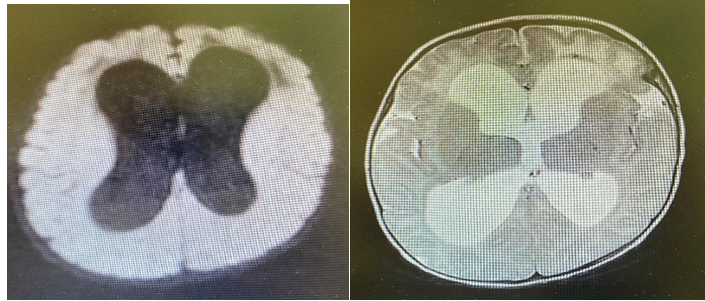
Figure 4
