Determination of Prognosis and Survival of Patients with Spinal Cord Compression Syndrome (SCCS) in an Argentine University Institution
Determination of Prognosis and Survival of Patients with Spinal Cord Compression Syndrome (SCCS) in an Argentine University Institution
Mesples B 1*, Martínez JJ 1, Jové F 1, Toranzos C 1, Ortega- Chahla E 2 , Mazzon , A 2. Zaloff Dakoff, J. 2
1 Oncology Clinic.
2 Neuro-Oncology Functional Unit, Angel H. Roffo Oncology Institute, University of Buenos Aires, Argentina.
*Correspondence to: Mesples B, Oncology Clinic.
Copyright.
© 2024 Mesples B. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 21 October 2024
Published: 01 November 2024
DOI: https://doi.org/10.5281/zenodo.14160011
Abstract
Spinal cord compression syndrome (SCCS) is an oncological emergency that requires a rapid therapeutic response. The Bauer Score (BS) determines the patient's survival in order to determine the treatment. The SINS and ESCCS scores allow us to recognize the risk of instability and the degree of neurological involvement.
An institutional retrospective observational analysis was carried out on 54 medical records of patients admitted to the Oncology Clinic Ward of the Institution from January 2017 to June 2022, applying the prognostic scores and treatment instituted.
55% were male with a mean age of 56 years (18 - 79). The main cause was breast cancer (15%).
50% of the patients were receiving oncological treatment. The dominant site was dorsal (52%) followed by lumbosacral (29%). 53% suffered multiple involvement, with pain (70%) being the most frequent symptom. The average hospital stay was 15 days. All patients who suffered CM presented deterioration of the ECOG. Applying the BS, 48% presented score 2. 28% and 22% presented scores of 0-1 and 3-4. All received corticosteroids as the main treatment. Survival was 87 days. Scores greater than or equal to 2 resulted in a survival of 150 days. 26 patients (48%) died during hospitalization or immediately in the following weeks.
Mortality between 40-60% of the sample analyzed. The majority presented injuries with a high risk of neurological complications.
We conclude that the correct use of these scores demonstrates the short- and medium-term prognosis of patients and the importance of better articulating the different protagonists that make up the multidisciplinary team to address this syndrome.
Keywords: Spinal cord compression syndrome (SCCS), Bauer Score (BS), SINS Score, Epidural Spinal Cord Compression Scale (ESCCS)
Determination of Prognosis and Survival of Patients with Spinal Cord Compression Syndrome (SCCS) in an Argentine University Institution
Introduction
Spinal cord compression syndrome (SCCS) is an entity with a poor prognosis in the natural evolution of solid and oncohematological tumors. Due to the potential irreversible neurological damage, it is considered an oncological emergency, the prognosis of which will depend largely on the type of primary tumor, the number and location of the lesion(s), the time of evolution until medical consultation and the functional status of the patient.
SCCS occurs in up to 5% of patients considered “terminal.” Its incidence varies, being more frequent in lung, breast and prostate cancer. In up to 35% of these patients, it may correspond to the first systemic manifestation of this disease.
For all these reasons, this syndrome requires rapid identification and response by the healthcare providers, as well as a multidisciplinary approach to achieve greater benefit for the patient. 1
Clinical presentation
The most commonly affected site is the thoracic spine, followed by the lumbar and cervical spines. Pain is present in 80-95% of cases, is usually constant, and worsens at night, with Valsalva maneuvers, or when lying down.
Along with the pain, we can also find neurological symptoms that will be related to the height of the dominant lesion(s). Motor symptoms usually predominate at the beginning, and as the disease progresses over time, sensory symptoms appear followed by autonomic deficit and thus a worse prognosis. 1
Diagnosis
The complementary reference method is magnetic resonance imaging (MRI) of the spine with intravenous contrast, with a sensitivity of 93% and a specificity of 97%. This should be of the entire spine since between 20-35% of patients have multiple non-contiguous compression lesions and the pain does not always correlate with the image. 4
Other alternative methods include computed tomography (CT), which provides less detailed description of the lesions, or computed myelography, both of which are useful (when MRI is contraindicated).
Positron emission tomography (PET-CT) has poorer anatomical resolution and its negative predictive value is low for detecting the presence of spinal cord compression, so its use is not recommended in this entity. 1
Patient prognosis
The correct determination of the Functional Performance Status of the patient (ECOG/ Karnofsky ) with SCCS is of vital importance since it allows us to predict the patient's survival, determine their quality of life and thus adapt the treatment to avoid therapeutic obstinacy. 7
Fig 1
Currently, we have several prognostic scores for patients with spinal cord compression. The first one to consider is Bauer's, which allows us to determine the patient's survival rate based on the primary tumor, the number of bone metastases, and the existence of visceral involvement.
Depending on the presence (or not) of these positive prognostic factors, one can determine the surgical approach or strategy.
Fig 2
A score of 3-4 points corresponds to a median survival of 28 months with neurosurgical treatment, and our goal should be local control in the medium term. A score of 2 points corresponds to a median survival of 18 months, so the neurosurgical approach continues to be of utmost importance, the goal being oriented towards short-term symptomatic palliation. Finally, with a score of 0-1, the median survival corresponds to approximately 5 months. Here, the therapeutic effort should be mainly non-specific palliative, contraindicating major surgeries based on the risk/benefit ratio of this scenario for the patient.
With this system, simple and easy to implement, we can determine the prognosis and evolution of the patient according to their underlying disease and the benefit that our intervention will have, taking into consideration that doing more is not always the best for the patient.
Fig 3
On the other hand, there are scores that allow determining the degree of instability of the spine and the degree of spinal cord compression. These are the Fisher and Bilsky scores , respectively. 8
The first of these, called the Spinal Instability Neoplastic Score (SINS) by Fisher and collaborators, allows us to determine the degree of instability of the spine according to the dominant lesion(s). 7
When all these variables are summed, we obtain a score between 0 and 6, which suggests that the spinal cord compression is stable and the risk of neurological complications is low; a score of 7 to 12 represents an intermediate risk, and a score of 13 to 18 indicates a high risk of spinal instability.
Bilsky 's working group , also called Epidural Spinal Cord Compression Scale (ESCCS) helps us to characterize the degree of spinal cord involvement, considering those lesions as high risk (2 - 3) when the spinal cord is affected, on the contrary, if only bone lesions are evident, the lesion is of low risk of permanent neurological compromise. 8
Applied correctly, these systems allow us to speed up the surgical approach to avoid irreversible damage. 1
Treatment
After rapid identification and diagnosis, the initial management of these patients should be urgent and consists of treatment with intravenous corticosteroids with dexamethasone (depending on the location and series, the doses are variable) but the administration of a bolus of 16 mg followed by 8 mg every 12 hours IV, is effective in reducing inflammation and prevents the adverse effects of higher doses of corticosteroids. 5,6,9 In addition to this, supportive treatment aimed at symptomatic management of the patient should be performed, including analgesics of different mechanisms of action and intensity, when pain is present, as well as adjuvants ( pregabalin , amitriptyline) or bone modifying agents, can be very useful. 1
In the case of dysautonomic involvement, we must not forget the use of laxatives to avoid constipation caused by opioids or by spinal cord compression itself, as well as bladder catheterization to avoid acute urinary retention. 1
Regarding the surgical approach, it is known that surgery followed by radiotherapy has more benefits than these two modalities used separately in terms of results such as post-surgical walking time , lower dose of analgesics, shorter hospital stay and longer survival. 2
These previously mentioned scores, along with the biological characteristics of the oncological disease, give rise to the mnemonic rule NOMS (“ N eurologic – Oncologic – Mechanical – Systemic ”) that allows us to integrate these modalities in order to choose the best therapeutic strategy 3 . For this, the neurological and mechanical components refer to the Bilsky and Fisher scores respectively , mentioned above.
The oncological component refers to the radiosensitivity of the primary tumor and its metastasis. It is known that lymphoma, multiple myeloma and germ cell tumors (seminomas) have high radiosensitivity, while tumors such as melanoma, sarcoma and kidney cancer present a certain degree of resistance to this type of therapy. 3
The systemic component consists of two elements. The first is the state of the oncological disease at the time of diagnosis of spinal cord compression. Does it occur in a context of uncontrolled systemic progression and/or after multiple lines of treatment? The second is the comorbidities of our patient. Can he/she undergo decompressive surgery? What is the surgical risk?
Fig 4
By adding these different variables, in a multidisciplinary manner, we can define the best treatment option for our patients. It is vitally important to be able to recognize those who will benefit from intensive treatment so as not to delay its early initiation and thus its recovery .
In most cases, spinal cord compression syndrome marks the entry into the specific oncological terminal phase and is a “catastrophic” condition for the patient that not only causes the loss of autonomy, but also psychologically affects both the patient and the family group surrounding him.
In a clinical situation with a poor prognosis, combined with difficulties in accessing the best medical treatment, prognostic scores greatly assist the medical team in taking action and in managing information for the patient.
Materials and Methods
For this work, a retrospective observational institutional analysis was carried out on 54 patients hospitalized for spinal cord compression in the Oncology Clinic ward from January 2017 to June 2022, through the database of the Clinical Oncology Residency service of the Ángel H. Roffo Oncology Institute located in the Autonomous City of Buenos Aires, Argentina.
Among them, the incidence in male patients was 55.5% (30) , while in female patients it was 44.4% (24) . The majority (regardless of gender) had an age range of 18 - 79 years, with a median of 56.5. ( Table 1 )
Regarding the analysis of the primary tumor, the main tumors reported were breast (15%), melanoma (9%), kidney (9%), prostate (7%) and lung (7%). If we analyze the incidence of spinal cord compression in terms of the stage of the disease at the time of diagnosis, we can see that the majority corresponds to locally advanced or de novo metastatic tumors (33% and 43% respectively).
In accordance with the poor prognosis of this entity, the majority had an initial ECOG score of ECOG 3/4 (37% and 22% respectively). 50% of the patients were receiving systemic oncologic treatment at the time of spinal cord compression.
The dominant vertebral lesion (the one that caused the symptoms that motivated the hospitalization to the general ward) was at the dorsal or thoracic level (52%) followed by the lumbosacral (29%). 53% of these patients suffered multiple involvement at the time of diagnosis (i.e. 4 or more lesions along the spine). Among these, the most frequent symptom was pain (70%), also presenting neurological symptoms in 48% ( sensory , in its paresis or paraparesis variants of 92% (24) - motor , i.e. weakness or plegia 73% (19) and autonomic , constipation and/or urinary incontinence 34% (9). Only one patient was diagnosed through images.
Analyzing the time from the onset of symptoms until admission to the Oncology Clinic ward, the average time was 15.27 days (with a range that remained between 0 and 142 days). According to what is known about the underlying pathophysiology of neuronal damage caused by ischemia secondary to spinal cord compression, the time of evolution is crucial in the prognosis and subsequent sequelae; it is interesting to note that 22 patients (40.7%) were admitted within 72 hours or less (time considered critical for action). However, in all patients who suffered from SCCS, deterioration in performance status was observed, regardless of how quickly the therapy was installed.
The form of presentation depends fundamentally on the height of the dominant lesion in the spine. Analyzing the deterioration of the ECOG according to this parameter, it seems that it was not a determining factor when influencing the prognosis of our patients; that is, it does not matter if the lesion is cervical, thoracic or lumbosacral, the worsening of the performance status occurs in the same way.
|
Table 1. Characteristics of the patients analyzed - %(n) |
|
|
Sex Male Female |
55.5% (30) 44.4% (24) |
|
Age Under 35 years old Between 35 - 65 years old Over 65 years old |
56.5 (18 - 79) 24% (13) 55.5% (30) 32% (11) |
|
Time elapsed from the onset of symptoms to hospitalization |
15.27 days (0 - 142) |
|
Primary tumor Breast Prostate Sarcomas (unspecified) Kidney Melanoma Lung Cervix-uterus Parotid Germinal Lymphoma Colon Bladder Oral cavity Oropharynx |
15% (8) 13% (7) 11% (6) 9% (5) 9% (5) 7% (4) 5% (3) 3% (2) 3% (2) 3% (2) 3% (2) 1% 1% 1% |
|
Stage I II III IV |
11% (6) 13% (7) 33% (18) 43% (23) |
|
Initial ECOG 0 - 1 2 3 4 |
15% (8) 22% (12) 37% (20) 22% (12) |
|
Vertebral involvement Cervical Dorsal Lumbosacral |
7.5% (4) 52% (28) 29% (16) |
|
Multiple injuries yes (more than 4) No |
53% (29) 46% (25) |
|
Predominant symptom Pain Neurological Both image |
70% (38) 22% (12) 48% (26) 1.85% (1) |
|
In active oncological treatment at the time of SCCS Yes No |
50% (27) 50% (27) |
|
Type of treatment (27) Chemotherapy Targeted therapy Immunotherapy Hormonal Combined |
33.3% (9) 15% (4) 7.4% (2) 22.2% (6) 22.2% (6)
|
Results
In the observational analysis of the collected data, applying the Bauer Score (estimated survival and treatment intensification calculation), 48.15% of patients benefited from a palliative approach in the short term, meaning that, if treated appropriately, an estimated survival of 18 months is expected (score 2). In contrast, 27.7% and 22.2% presented scores of 0-1 and 3-4 respectively. These numbers are not negligible for patients in whom the treatment is exclusively palliative, since survival does not reach 6 months.
It is interesting to note that in the group of patients with the best prognosis (3-4; estimated survival of 28 months), none were treated surgically. However, regardless of the Bauer score, all received corticosteroids as the main treatment, followed by corticosteroids plus radiotherapy.
Can we infer the aggressiveness of the disease clinically? It is not such a simple question to answer, but we can observe that spinal cord compression occurred in a high percentage (between 45 - 60%; 46.7%, 48.15% and 22.2% in groups 0-1, 2 and 3-4, respectively) of patients who were exposed to systemic treatment (either chemotherapy, targeted therapy, hormonal therapy, immunotherapy or combinations of these). Fundamentally, in the 3 groups, it was hormonal therapy (in accordance with the incidence of SCCS according to the primary tumor; breast and prostate) and the combination of different treatment modalities. (Table 2)
|
Table 2. Bauer score |
|||
|
Score |
0 -1 |
2 |
3 - 4 |
|
% (n) |
27.7% (15) |
48.15% (26) |
22.2% (12) |
|
Treatment performed SCCS |
Only Corticosteroids 46.7% (7) Corticosteroids and radiotherapy 46.7% (7) Corticosteroids and surgery 6.7% (1) |
Only Corticosteroids 42% (11) Corticosteroids and radiotherapy 34.6% (9) Corticosteroids and surgery 15.4% (4) Corticosteroids and chemotherapy 7.7% (2) |
Only Corticosteroids 66.7% (8) Corticosteroids and radiotherapy 33.3% (4) Corticosteroids and surgery 0% (0)
|
|
Systemic treatment performed at the time of SCCS |
YES - 46.7% (7) Hormonal therapy (1) Targeted therapy (1) Chemotherapy (2) Combination (3)
NO - 53.3% (8) |
YES - 46.15% (12) Hormonal therapy (4) Targeted therapy (2) Chemotherapy (4) Combination (2)
NO -53.8 % ( 14) |
YES - 58.3% (7) Hormonal therapy (1) Targeted therapy/IT (2) Chemotherapy (1) Combination (3)
NO - 41.6% (5) |
|
Survival |
0 - 407 days Average: 75.67 days 40% (6) died at the time during hospitalization or near hospital discharge.
|
0 - 751 days Average: 220.5 days 46% (12) died at the time during hospitalization or near hospital discharge
|
0 - 438 days Average: 181.8 days 58.3% (7) died at the time during hospitalization or close to hospital discharge
|
In the entire population analyzed, the median survival was 86.6 days. Of these, 26 patients (48%) died during hospitalization or in the immediate days/weeks following. Analyzing according to the different scores of the Bauer Score, we observed a mortality rate between 40 - 60% of the analyzed sample (40%, 46% and 58.3% in groups 0-1, 2 and 3-4, respectively). (Table 2)
Scores between 0-1 (15 patients) had a mean survival of 75.67 days; however, those with a better score, such as Score 2, had a longer survival with a mean of 220.5 days. Scores of 3-4 had a mean of 181.8 days (more than double that of those with a worse prognosis). (Table 2)
These results reflect the results known worldwide, although we can observe that in our sample, those with an intermediate score (Score 2) had a higher survival rate; probably because these patients have a higher n (26), when we carefully analyze the information obtained from the other two subgroups of patients, we can see that despite having a similar n (15 vs 12 patients for those with risk 0-1 and 3-4, respectively), survival is much better for the latter.
However, if we analyse the sample from those patients with a high risk of neurological and potentially irreversible complications (unstable spine and high-grade injuries) only a small number of patients (less than 30%) presented low-risk injuries. (Tables 3 and 4)
|
Table 3. Spinal Instability Neoplastic Score (SINS) |
||||
|
Score |
0 - 6 (stable) |
7 - 12 (potentially unstable) |
13 - 18 (unstable) |
Unknown |
|
% (n) |
16.7% (9) |
55.5% (30) |
13% (7) |
15% (8) |
|
Treatment performed SCCS |
Only Corticosteroids 44.4% (4) Corticosteroids and radiotherapy 22.2% (2) Corticosteroids and surgery 22.2 % ( 2) |
Only Corticosteroids 46.6% (14) Corticosteroids and radiotherapy 43.3% (13) Corticosteroids and surgery 6.67% (2) Corticosteroids and chemotherapy 3.3% (1) |
Only Corticosteroids 71.4% (5) Corticosteroids and radiotherapy 14.3% (1) Corticosteroids and chemotherapy 14.3% (1) Corticosteroids and surgery 0% (0)
|
|
That is to say, when SCCS was diagnosed, the vast majority of the time it was in patients with borderline ECOG and lesions with a high risk of neurological complications.
|
Table 4. Epidural Spinal Cord Compression Scale |
|||
|
RISK |
HIGH |
LOW |
Unknown |
|
% (n) |
62% (33) |
26% (14) |
13% (7) |
|
Treatment performed SCCS |
Only Corticosteroids 42.4% (14) Corticosteroids and radiotherapy 24.3% (8) Corticosteroids and surgery 6% (2) Corticosteroids and chemotherapy 3% (1) |
Only Corticosteroids 35.7% (5) Corticosteroids and radiotherapy 21.4% (3) Corticosteroids and surgery 14.3% (2) Corticosteroids and chemotherapy 0% (0) |
Only Corticosteroids 42.8% (3) Corticosteroids and radiotherapy 51.1% (4)
|
Discussion
There are many factors that influence the disease to become metastatic ( genetic ; the function of neoplastic cells to induce the proteins and substances necessary to create the niche where the lesion will subsequently persist, extracellular matrix ; since the exchange between these malignant cells and the cellular/tumor microenvironment generates the selection of the most suitable clones for this growth and development; environmental factors ; such as repetitive exposure to the same noxa, for example, tobacco in patients with lung cancer who continue to smoke, among others).
There are many mechanisms, therefore, that make this syndrome, which is nothing more than the metastatic presentation of the disease in the vertebral bodies of the individual, inherently indicate a poor prognosis (this without mentioning the risk of permanent paralysis or plegia as a secondary condition) for our patients
In line with this inferred “aggressiveness,” which may at times seem obvious (a stage IV tumor is more serious than a stage I or II tumor), we were able to obtain data that support this observation.
It should be noted that, due to the heterogeneity of our sample and the number of patients analyzed, we were unable to determine at the time of this analysis whether histology and/or histological grade influence the evolution of this entity. The ability to extrapolate this to what happens with oncological disease in general, and to interpret it as well, must be done carefully, without forgetting the intrinsic characteristics of each tumor in particular.
The same applies to staging; What has more influence, the size of the primary tumor (T), the nodal component (N) or the de novo metastatic presentation (M)? Unfortunately, we were not able to answer that question either, however, in the analyzed database, we can see that the majority of patients who presented with SCCS did so with de novo Stage IV onset, 43% (23 patients).
In our sample, we can observe that it affected the majority of patients who were receiving active systemic treatment, that is, they were under the effects of the best standard treatment according to the oncological guidelines of the time and in a multiple manner (that is, many cell clones acquired the capacity to affect the bone marrow).
We can also observe this aggressiveness in an empirical clinical way, since all patients showed a deterioration in functional performance status, regardless of the affected vertebral height. Is it correct then to ask ourselves what is the use of the rapid establishment of neurological treatment if all patients will eventually present the deterioration that will lead them to exclusive palliative care?
Oncological disease forces the scientific community to work in a multidisciplinary manner, and SCM is just another example where this is demonstrated.
There are more and more treatments available, both in the surgical field, as well as in clinical oncology and radiotherapy to deal with the disease, both for localized and advanced disease, and this often forces us to ask ourselves "how far we can go" without falling into therapeutic obstinacy. If spinal cord compression inherently marks a stage of poor prognosis and often the admission to the end of life, shouldn't we focus more on palliative aspects rather than on the ways and speed of treating it?
It is not an easy question to answer. The constant advancement of medicine in the different actors involved in the treatment of this syndrome forces us to constantly look for ways to improve all possible strategies to provide our patients with the best possible care.
Thus , the complexity of spinal cord compression lies in finding the “right time” to act in the most correct way with those patients who have an adequate survival rate (i.e. an assured benefit), even in a situation of poor prognosis with a disease, as we have already seen, aggressive; to receive intensive treatment that is not free of complications or subsequent risks (i.e. surgery).
The correct implementation of these scores not only demonstrates the short- and medium-term prognosis of patients regarding the future of their disease, but also the importance of better articulating the different protagonists.
Our work has weaknesses; the first is the number of cases. Although it is not easy to find 54 patients with spinal cord compression, the Angel H. Roffo Oncology Institute is a national referral cancer center, which makes it more difficult to obtain this number of patients, unlike an acute care hospital, where oncological pathology and its complications are often not the most frequent reason for consultation. That said, the sample is not enough to be able to analyze the effect of T or N on the stage of the disease. As occurs in the different tumor models, we believe that it does have an influence, but at the moment we do not have enough statistical power to demonstrate it.
Second, not all specialists use these scores in daily practice and the patients analyzed since 2017 and 2018 were not considered in the same way by the medical team at that time.
Third, the observational and retrospective nature of the study has less statistical weight than it would have if it were prospective. Unfortunately, we do not have enough time to implement this dynamic. Perhaps for later years it may be interesting to complement it with this information, since, as we saw previously, it influences the oncological strategy.
Fourth, access to health systems is a problem worldwide, and Argentina is not exempt from this. Many of the patients analyzed do not have or did not have medical coverage and this unfortunately affects everything from the choice of diagnostic method (it is easier to perform a CT scan than an MRI at the expense of the latter providing greater resolution), to systemic treatment (often due to lack of delivery of oncological medication, suboptimal treatments are instituted) or local treatment (lack of surgical materials for those patients who need it or access to radiotherapy).
This analysis confirms the global data on SCCS that we already knew, namely that the main tumors that cause it are breast, prostate, kidney and lung; dorsal or thoracic involvement being the most frequent, presenting in most cases with pain as the first clinical manifestation. But it also allows us to characterize the clinical-oncological situation in greater detail, confirming the severity of the situation not only from the potential neurological damage but also in the impact on the quality of life and survival of the affected patients.
This forces the medical community not only to be more alert to the form of clinical presentation in order to act quickly, but also to know how to choose more correctly and with the smallest possible margin of error, those patients who, even in an instance of poor prognosis, benefit from an aggressive and multimodal treatment in a multidisciplinary setting.
References:
1- Assessment and Management of Patients with Metastatic Spinal Cord Compression: A Multidisciplinary Review
Andrew J. Lawton, Kathleen A. Lee, Andrea L. Cheville, Marco L. Ferrone, Dirk Rades , Tracy A. Balboni , and Janet L. Abrahm . J Clin Oncol 36. © 2018
2- Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomized trial
Roy A Patchell , Phillip A Tibbs, William F Regine, Richard Payne, Stephen Saris, Richard J Kryscio , Mohammed Mohiuddin, Byron Young. Lancet 2005; 366:643–48
3- The NOMS Framework: Approach to the Treatment of Spinal Metastatic Tumors Ilya Laufer, David G. Rubin, Eric Lis, Brett W. Cox, Michael D. Stubblefield, Yoshiya Yamada, Mark Bilsky . The Oncologist
4- Sensitivity and specificity of MRI in detecting malignant spinal cord compression and in distinguishing malignant from benign compression fractures of vertebrae Li KC, Poon PY; Magn Reson Imaging 6:547-556, 1988
5- A pilot randomized comparison of dexamethasone 96mg vs 16 mg per day for malignant spinal-cord compression treated by radiotherapy: TROG 01.05 Superdex study
Graham PH, Capp A, Delaney G; Clin Oncol (R Coll Radiol ) 18:70-76, 2006
6- Metastatic spinal cord compression and steroid treatment: A systematic review Kumar A, Weber MH, Gokaslan Z; Clin Spine Surg 30:156-163, 2017
7- A novel classification system for spinal instability in neoplastic disease: An evidence-based approach and expert consensus from the Spine Oncology Stud Group. Fisher CG, DiPaola CP, Ryken TC; Spine 35:E 1221-E1229, 2010
8- Reliability analysis of the Epidural Spinal Cord Compression Scale Bilsky MH, Laufer I, Fourney DR; J Neurosurg Spine 13:324-328, 2010
9- Corticosteroid Treatment for Metastatic Spinal Cord Compression: A Review Gordon D. Skeoch, BA1, Matthew K. Tobin, BS1, Sajeel Khan, MD1, Andreas A. Linninger , PhD1, and Ankit I. Mehta, MD1
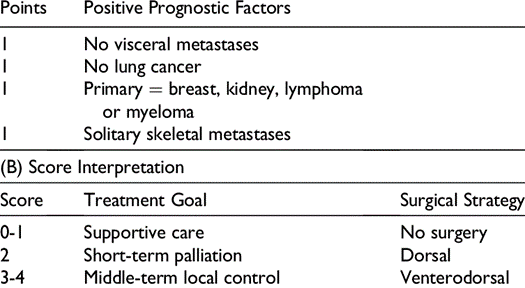
Figure 1
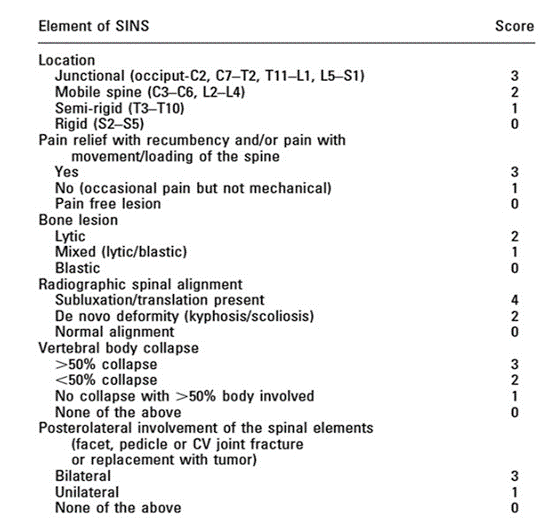
Figure 2
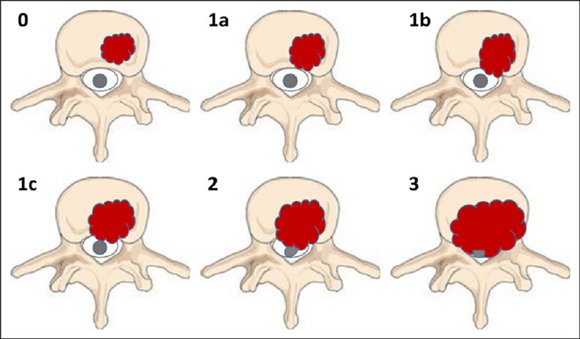
Figure 3
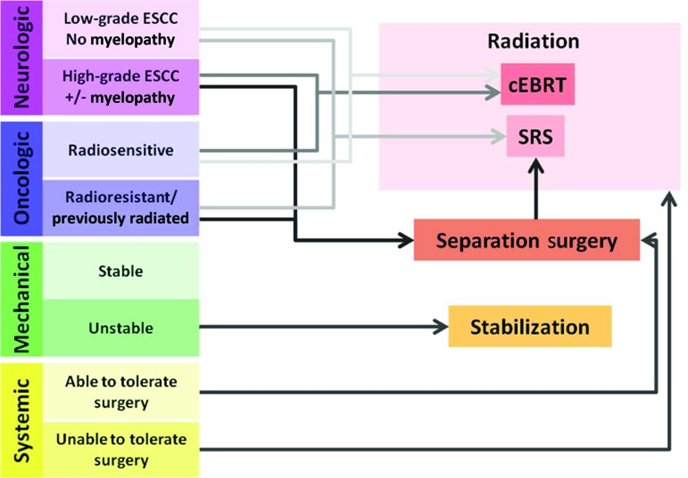
Figure 4
