Leptomeningeal Carcinomatosis in Metastatic Triple-Negative Breast Cancer: A Case Report of a 28-Year-Old Woman
Leptomeningeal Carcinomatosis in Metastatic Triple-Negative Breast Cancer: A Case Report of a 28-Year-Old Woman
Jose Portugal *
*Correspondence to: Jose Portugal. Medical Oncologist, Santiago Tavara Naval Medical Center.
Copyright.
© 2024 Jose Portugal. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 26 October 2024
Published: 01 November 2024
DOI: https://doi.org/10.5281/zenodo.14160015
Abstract
A 28-year-old female presented to the medical oncology department with complaints of progressive severe headache, multiple episodes of vomiting and generalized weakness. Her past medical history was notable for triple-negative breast cancer with liver and adrenal metastasis that was diagnosed approximately 5 months prior. She was undergoing treatment with chemotherapy (4 cycles of doxorubicin and cyclophosphamide-based chemotherapy followed by taxane-based chemotherapy) when after her 5th cycle (1st taxane), she developed a severe headache. Radiologic studies were performed in the department. MRI Brain was done which showed 1.5 x 1.5 mm and 2 x 2 mm focal blooming in the left insular cortex and left frontal lobe respectively which were suggestive of calcified granuloma. A lumbar puncture with a cerebrospinal fluid analysis revealed the presence of malignant cells. Together with clinical features and cerebrospinal fluid findings, leptomeningeal carcinomatosis was diagnosed. This case report presents an uncommon but well-known complication of breast cancer ~ Leptomeningeal carcinomatosis.
Leptomeningeal Carcinomatosis in Metastatic Triple-Negative Breast Cancer: A Case Report of a 28-Year-Old Woman
Introduction
One of the late complications of malignant tumors that metastasize to the cerebrospinal fluid and leptomeninges is Leptomeningeal carcinomatosis. Leptomeningeal carcinomatosis is an uncommon but well-known complication of breast cancer, where patients have a variable clinical presentation, as any level of the central nervous system (CNS) may be affected (1). Most common clinical presentations include migraines, altered mental sensorium, cerebellar signs, back pain, leg weakness etc (2). During the course of manifestation, CSF flow is impaired and the patient may present with symptoms of hydrocephalus, like positional headaches, nausea, vomiting, and somnolence (3). The incidence of Leptomeningeal carcinomatosis is challenging to determine (3). According to various studies, the approximate prevalence of the leptomeningeal disease is
approximately 19% (1). Approximately 8 % of all cancer patients present with leptomeningeal disease (3). Recent advances in neuroimaging, anti-cancer medications and other treatment modalities play a vital role in leptomeningeal diseases in cancer patients.
Figure 1. MRI Brain imaging showing 1.5 x 1.5 mm and 2 x 2 mm focal blooming in the left insular cortex and left frontal lobe respectively which were suggestive of calcified granuloma.No active metastatic lesion seen.
Figure 2. MRI Brain imaging showing 1.5 x 1.5 mm and 2 x 2 mm focal blooming in the left insular cortex and left frontal lobe respectively which were suggestive of calcified granuloma. No active metastatic lesion seen.
Case Presentation
A 28-year-old female nonsmoker presented to the medical oncology department with progressively worsening headache, multiple episodes of vomiting and generalized weakness. Five months prior, she was diagnosed with right-breast triple-negative Infiltrating ductal carcinoma grade II (TNBC) with liver and adrenal metastasis. She was started on chemotherapy with doxorubicin, cyclophosphamide followed by paclitaxel. However During the course of her treatment, after the first taxane(5th cycle of chemotherapy), she developed a severe headache and multiple episodes of vomiting. Magnetic resonance imaging (MRI) of the brain with contrast was obtained. MRI showed 1.5 x 1.5 mm and 2 x 2 mm focal blooming in the left insular cortex and left frontal lobe respectively which were suggestive of calcified granuloma. However, the patient’s clinical picture was concerning for the development of metastatic central nervous system (CNS) disease however MRI Brain did not correlate with the clinical picture. Given the patient’s clinical history and new
neurologic symptoms, concerns about leptomeningeal disease were raised. Lumbar puncture with CSF analysis was performed, which showed the presence of large atypical cells. Together with imaging and CSF analysis, Leptomeningeal carcinomatosis was diagnosed. Treatment was palliative with intrathecal
methotrexate (IT MTX) to improve her neurologic symptoms and prolong survival.
Discussion
Leptomeningeal carcinomatosis is an uncommon but classic late-stage complication of breast carcinoma that has become increasingly prevalent. The most common malignancy which metastasizes to leptomeninges includes Breast cancer, non-small-cell lung cancer and melanoma (3). Breast carcinoma consistently contributes the most to the total leptomeningeal carcinomatosis cases, despite only about 5% of breast cancer patients developing leptomeningeal involvement (1,3). Initial physical exam findings may be overlooked due to subtle presentation (3). Clinical suspicions must remain high in known metastatic breast cancer patients that develop neurological symptoms such as altered sensorium, headache, vomiting, hemiparesis etc (7). Various differentials must also be kept in mind while dealing with leptomeningeal carcinomatosis and should never be overlooked. These conditions include infectious meningitis, metabolic and toxic encephalopathies,
sarcoidosis, paraneoplastic syndromes, etc (1). Increased clinical awareness of Leptomeningeal carcinomatosis allows for earlier detection and treatment ultimately leading to a better and early treatment, thus providing a better quality of life to the patient (1).
Various Neuroimaging modalities have come up in due course of time, however, MRI stays a critical imaging modality in the initial workup process for leptomeningeal diseases. Since these metastatic malignancies can involve the entire craniospinal axis, brain with whole spine imaging is recommended (8).
T1 and T2-weighted sequences with contrast should be performed. Differentiating metastatic leptomeningeal enhancement from CNS vasculature or flow airfacts is often challenging if MRI is not done in enough enhanced planes (9). Computed Tomography is not recommended for evaluation and clinical decision-making in neurological malignancies. (8). CT scans have a significantly lower sensitivity as compared to MRI (8). The characteristic finding of leptomeningeal involvement on MRI is a meningeal enhancement (9). Radiologically, Leptomening malignancies and metastasis are differentiated based on location and number, as metastatic neoplasms to the leptomeninges are more commonly seen at the base of the brain, dorsal spinal cord, and cauda equina (1). The presence of malignant cells in CSF analysis is however the gold standard for the diagnosis of metastatic leptomeningeal disease (10). However, significant false-negative rates have also been reported (5). Therefore, serial CSF sampling can improve the sensitivity (5). According to various studies, approximately 53% of patients were diagnosed by MRI alone, 23% were diagnosed by CSF cytology and 24% by both MRI and CSF cytology (11). There it is concluded that neither MRI nor CSF cytology is a sensitive enough method when used alone (11). Thus, a combined clinical examination with either MRI findings or a CSF analysis is the basis to form a diagnosis of leptomeningeal carcinomatosis (5). Triple-negative Breast cancer is an aggressive variant of breast cancer and holds a very poor prognosis as compared to hormone-sensitive breast cancer (13). Because of its aggressive nature, Triple Negative Breast cancer has a very high chance of leptomeningeal spread (12). Moreover, Triple Negative Breast cancer is associated with a shorter interval between initial primary breast cancer diagnosis and the spread of the disease to leptomeninges (12). Once Leptomeningeal carcinomatosis has been diagnosed, treatment options remain limited and survival is often short (14). The standard treatment for leptomeningeal carcinomatosis is Intra thecal Methotrexate plus systemic chemotherapy with or without localized radiation therapy (3). With the advent of these treatment modalities, there has been an improvement in median survival to up to six months (3). Radiotherapy can also be useful for resolving impaired CSF flow in bulky leptomeningeal disease (15). However, no treatment modality has been shown to improve the overall survival (17).
Conclusions
Leptomeningeal carcinomatosis is a late-stage complication of Breast cancer, with a maximum incidence in Aggressive variants of breast cancer such as Triple-negative Breast cancer. Leptomeningeal carcinomatosis even though uncommon, is a well-known oncological entity that represents a terminal complication of breast cancer. Despite various recent neurological imagings, a combined clinical picture analysis and either MRI brain or CSF cytology has proven to be of standard significance. Other neurological conditions which mimic leptomeningeal carcinomatosis, such as infectious Meningitis should not be overlooked and appropriate analysis should be done. Further research is needed to determine better treatment options. Despite advancements in treatment options, leptomeningeal carcinomatosis leaves us with only a handful of options, one of them being intrathecal methotrexate. Other options include Radiotherapy, intrathecal chemotherapy and a combination of intrathecal methotrexate and chemotherapy, however, benefits in Overall Survival could not be established. Therefore to conclude, further research is needed for a better treatment plan in patients with leptomeningeal carcinomatosis
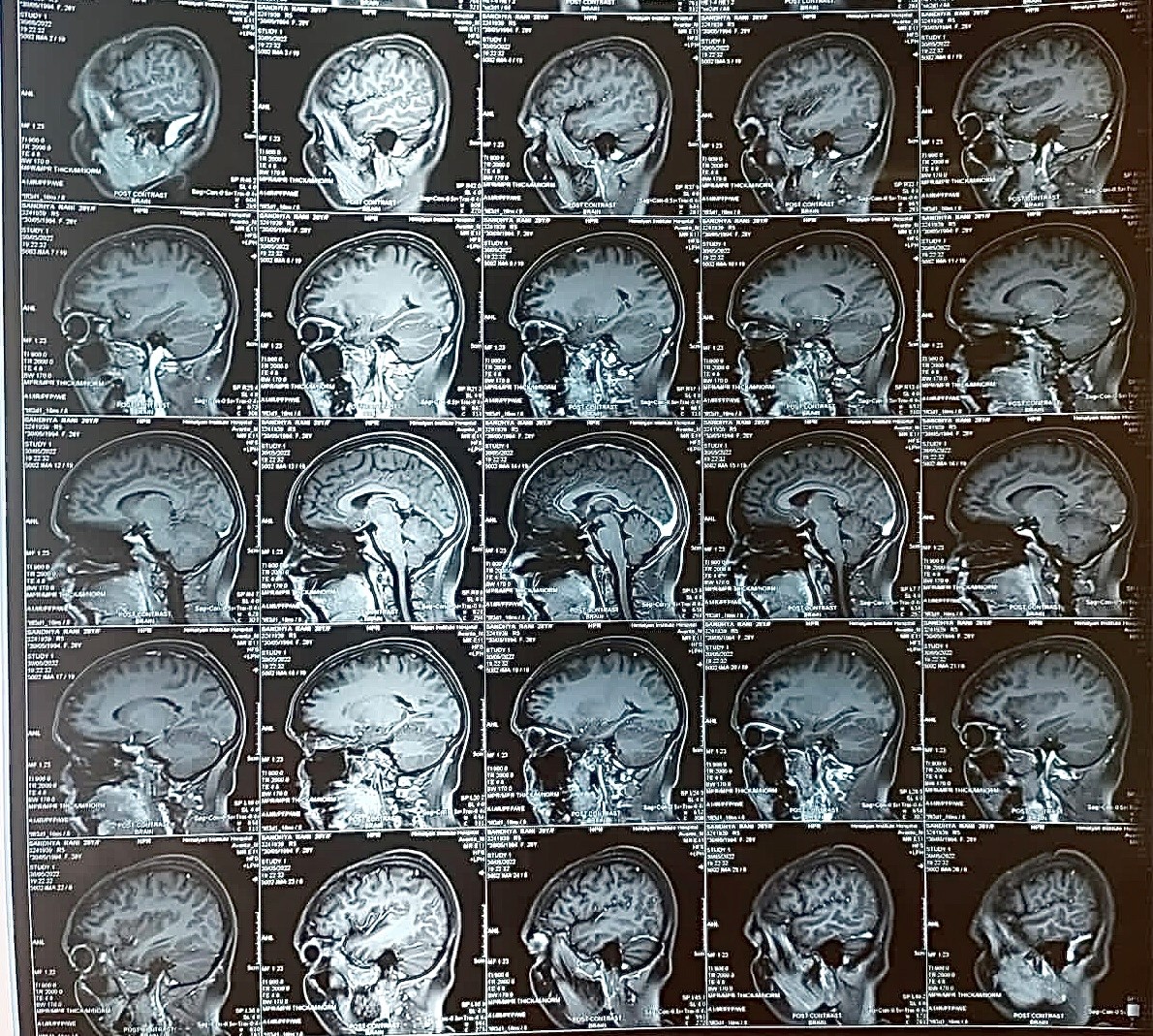
Figure 1
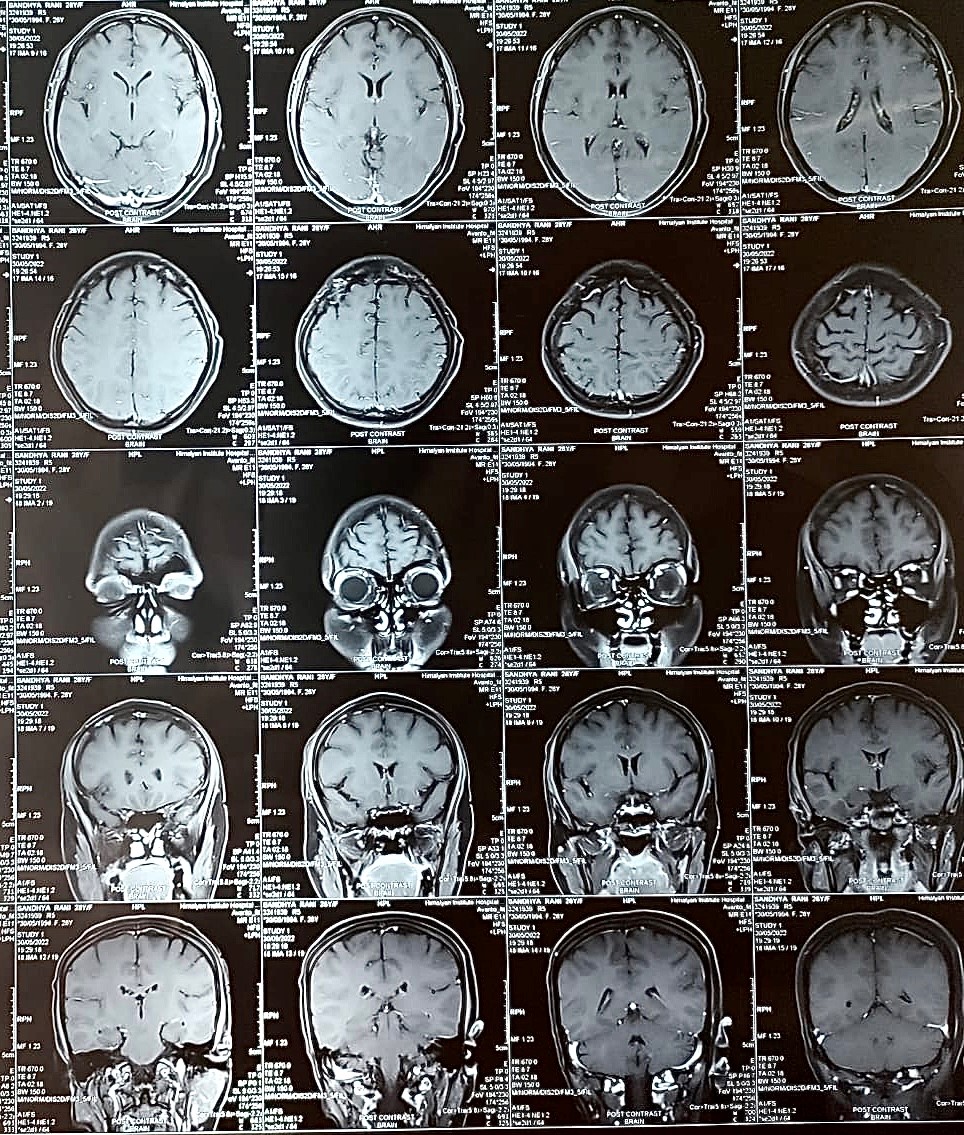
Figure 2
