PRP-Based Ovarian Rejuvenation: Extraction and Blood Separation Techniques
PRP-Based Ovarian Rejuvenation: Extraction and Blood Separation Techniques
Archana Singh1*, Varsha Ojha2
1) Archana Singh, Consultant IVF & Gynecologist, Indira IVF, Jodhpur, India.
2) Varsha Ojha, Specialist Gynecologist & Obstetrician, Prime Hospital, Dubai, UAE.
*Correspondence to: Archana Singh, Consultant IVF & Gynecologist, Indira IVF, Jodhpur, India.
Copyright
© 2024 Archana Singh. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 22 October 2024
Published: 01 November 2024
PRP-Based Ovarian Rejuvenation: Extraction and Blood Separation Techniques
Introduction
The process of ovarian rejuvenation and the use of Platelet-Rich Plasma (PRP) therapy to stimulate egg production in women with diminished ovarian reserve or ovarian dysfunction.
Ovarian Rejuvenation: Reawakening Dormant Follicles
This procedure is designed to help women who struggle with infertility due to ovarian aging or dysfunction by reactivating dormant follicles within the ovary. Dormant follicles are immature eggs that have not yet developed, and by stimulating them, this treatment aims to enable the ovaries to produce more eggs than they naturally would under normal circumstances. This allows women, even those with reduced fertility, to potentially conceive using their own genetic material.
Process of Egg Stimulation
Ovarian rejuvenation involves artificially stimulating the ovaries to **enhance egg production**. This can significantly increase a woman’s chances of conceiving, particularly for those who may have thought they were no longer able to produce eggs. PRP therapy is a key part of this process, as it uses the body’s own healing mechanisms to promote the development of eggs in the ovaries.
Indications for Ovarian Rejuvenation
This procedure is beneficial for women in a variety of reproductive scenarios, including:
- Menopausal or perimenopausal women under the age of 50 who may still have residual follicles in their ovaries but have ceased ovulating naturally.
- Infertile women over the age of 35 who have a low egg reserve (fewer remaining eggs) and low Anti-Mullerian Hormone (AMH) levels, which indicate reduced ovarian function.
- Women under the age of 35 who also have a low egg reserve and low AMH levels, suggesting premature ovarian aging.
- Women with premature ovarian failure (POF), a condition where the ovaries stop functioning normally before the age of 40.
- Primary ovarian insufficiency (POI), a condition similar to POF but often less severe, where ovarian function fluctuates, leading to inconsistent egg production.
- Women who have lost ovarian function due to chemotherapy or other medical treatments that damage ovarian tissue, leading to infertility.
Platelet-Rich Plasma (PRP) Therapy
PRP therapy is based on the body's natural healing process. When tissue is injured, the body’s immediate response is to deliver platelets to the site of injury. These platelets promote healing by releasing growth factors that attract stem cells to the area and stimulate regeneration. In the context of ovarian rejuvenation, PRP is used to:
- Activate dormant follicles in the ovaries.
- Encourage the growth and maturation of these follicles, which can lead to the production of viable eggs.
How PRP is Prepared
PRP is derived from the patient’s own blood (referred to as autologous PRP), which is drawn and then centrifuged to separate the red blood cells (RBCs) from the plasma. The plasma that remains is highly concentrated with growth factors—about 5 to 10 times more than what is found in whole blood. This concentrated "cocktail of growth factors" is then injected back into the ovaries to promote healing, regeneration, and egg development.
Benefits of Ovarian Rejuvenation with PRP
For women who have limited fertility options due to poor ovarian function, ovarian rejuvenation with PRP offers a new avenue of hope. By using the body's own regenerative capabilities, this treatment aims to help women conceive, even in cases where traditional fertility treatments may have failed.
The PRP process is minimally invasive and can be repeated if necessary, making it a safe and promising option for many women experiencing infertility due to ovarian issues. The ultimate goal of this therapy is to enable women to conceive using their own eggs, which can be life-changing for those who may have previously thought they could not have biological children.
Fig 1 : PRP Therapy
Materials and Methods
A study involving eight peri-menopausal women undergoing platelet-rich plasma (PRP) treatment found that ovarian function was monitored before and after the treatment. FSH, LH, E2, and AMH levels were determined before and after the treatment. The presence of developing follicles was confirmed through ultrasound scans. PRP was prepared using the RegenACR®-C Kit and injected into the ovaries using a transvaginal ultrasound-guided injection. All patients underwent natural cycle IVF without ovarian stimulation or GnRH antagonist supplementation. When a follicle was observed, ovulation triggering was achieved with 5000 IU of hCG and follicle aspiration was performed 32 hours later.
Results
The study confirmed successful ovarian rejuvenation 1-3 months after ovarian PRP treatment. Oocyte retrievals were successful in all cases, resulting in 2.50±0.71 follicles of 15.20±2.05 mm diameter, 1.50±0.71 oocytes, and 1.50±0.71 MII oocytes. All mature oocytes were inseminated by ICSI, and the resultant embryos were cryopreserved at 2pn stage until transfer. The study suggests that PRP infusion may enrich dysfunctional, peri-menopausal ovarian tissue with essential factors for angiogenesis and normal vascular function leading to tissue regeneration. Many peri-menopausal women may maintain a restricted amount of inactive primordial follicles, which could be activated by PRP growth factors or subsequent ovarian tissue regeneration and maturate into preantral and antral follicles. Platelet-derived growth factors (PDGFs) have been shown to enhance blood vessel formation and growth, and their receptors in granulosa cells suggest a potential association with primordial follicle activation. The recent detection of ovarian stem cells in human ovarian surface epithelium and their ability to differentiate into oocytes provide new data for the origin of PRP-derived follicles.
Conclusions
The study demonstrates the successful restoration of temporary ovarian activity in peri-menopausal women after autologous ovarian platelet-rich plasma treatment. The results suggest that PRP therapy could be a first-line treatment for ovarian regeneration and folliculogenesis reactivation in perimenopausal women. This treatment may extend fertility potential, making oocyte donation IVF cycles an ultimate option. PRP therapy stimulates the natural production of eggs in women with diminished ovarian reserve, premature ovarian failure, or other conditions affecting ovarian function, providing new hope for those who may have lost hope due to age or medical conditions.
Reference
1. Qureshi et al. PLoS One 2009;4:e7627. 4. Borrione et al. Am J Phys Med Rehabil. 2010;89: 854–61. 7. Bakacak et al. Gynecol Obstet Invest. 2016;81:225-31.
2. Stiles CD. Cell. 1983;33:653–655. 5. Callejo et al. J Ovarian Research. 2013;6:33. 8. White et al. Nat Med 2012;18:413–421.
3. Pietrzak and Eppley. J Craniofac Surg. 2005;16:1043-54. 6. Chang et al. Int J Clin Exp Med. 2015;8:1286-1290. 9. Virant-Klun et al. Differentiation 2008;76:843–856.
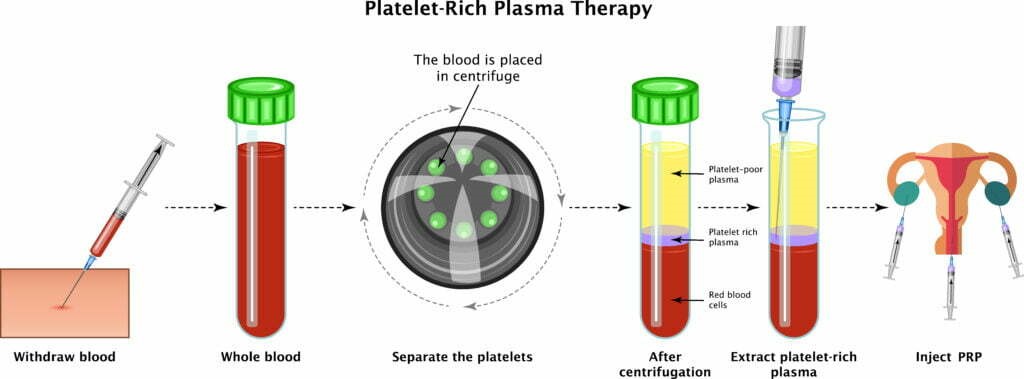
Figure 1
