Uterine Transplantation: Surgical Stages, Preservation Techniques, and Post-Transplant Care
Uterine Transplantation: Surgical Stages, Preservation Techniques, and Post-Transplant Care
Archana Singh1*, Varsha Ojha2
1) Archana Singh, Consultant IVF & Gynecologist, Indira IVF, Jodhpur, India.
2) Varsha Ojha, Specialist Gynecologist & Obstetrician, Prime Hospital, Dubai, UAE.
*Correspondence to: Archana Singh, Consultant IVF & Gynecologist, Indira IVF, Jodhpur, India.
Copyright
© 2024 Archana Singh. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 22 October 2024
Published: 01 November 2024
Uterine Transplantation: Surgical Stages, Preservation Techniques, and Post-Transplant Care
Introduction
A uterine transplantis a surgical procedure in which a healthy uterus is transplanted into a female patient whose uterus is either absent or diseased. This cutting-edge procedure offers hope for women who suffer from Absolute Uterine Factor Infertility (AUFI), a condition where the absence or abnormality of the uterus prevents normal embryonic implantation, rendering the woman infertile. Here's an in-depth look at uterine transplantation:
Absolute Uterine Factor Infertility (AUFI)
AUFI is a type of infertility where a woman is unable to conceive due to issues with the uterus, whether congenital (from birth) or acquired (later in life). This type of infertility is irreversibleby other medical interventions, and before the development of uterine transplants, women with AUFI had only two options for motherhood:
- Adoption
- Gestational surrogacy(which is restricted or banned in many countries)
Causes of AUFI
The uterus, a complex organ, plays a crucial role in embryo implantationand the support of pregnancy. Various conditions can lead to AUFI:
Congenital Causes:
- Mayer–Rokitansky–Küster–Hauser (MRKH) Syndrome: This is a congenital condition in which the uterus and the vagina are underdeveloped or absent. Women with MRKH are typically born without a functioning uterus but have normal ovaries and external genitalia.
Acquired Causes:
- Asherman’s Syndrome: This condition involves intrauterine adhesions (scar tissue within the uterus) which can lead to infertility and recurrent miscarriages.
- Pregnancy Interfering Myomas: Uterine fibroids (benign tumors) can interfere with pregnancy and sometimes lead to the need for a hysterectomy.
- Hysterectomies: Removal of the uterus due to medical conditions such as hemorrhage or trauma, except for malign tumors, can leave a woman infertile.
Uterine Transplant as a Treatment for AUFI
Uterine transplantation is considered a potential solution for women with AUFI. The process involves surgically placing a healthy uterus (from a donor) into the recipient. This transplanted uterus can then allow the woman to become pregnant and carry her own child.
Indications for Uterine Transplant
Women who are candidates for uterine transplantation typically meet the following criteria:
- Infertility due to uterine factors: This includes congenital absence of the uterus or removal of the uterus due to conditions like trauma or hemorrhage.
- Desire to have a baby: The patient must be motivated to undergo a transplant to achieve pregnancy.
- Medically impossible to have a baby otherwise: If the woman cannot conceive naturally due to the absence of a uterus, she may be a candidate.
- Age range: Ideal candidates are typically between 18-45 years of age, ensuring they are of reproductive age and can safely carry a pregnancy.
- Psychosocial stability: The emotional and psychological preparedness of the patient is essential, given the complex nature of the procedure and postoperative care.
- Healthy organs and systems: The recipient must have no significant health issues that could complicate surgery or postoperative recovery.
- Willingness to take immunosuppressive agents: After the transplant, the recipient must take immunosuppressive drugs to prevent the body from rejecting the transplanted organ. These drugs can have long-term side effects, so the patient must be fully informed.
The Process of Uterine Transplantation
1. Counseling: Extensive counseling is required before the procedure, including the risks involved, the need for lifelong follow-up, and the ethical considerations of organ transplantation.
2. Donor Uterus: The donor uterus can come from either a living donoror a deceased donor. The donor must meet stringent medical and ethical criteria to ensure the best possible outcome for the recipient.
3. Recipient Investigation: Thorough medical evaluations are performed to ensure the recipient is a suitable candidate for transplantation. This includes assessing the health of other organs, the reproductive system, and overall fitness for surgery.
4. In Vitro Fertilization (IVF): Before the transplant, the recipient undergoes an IVF cycleto create embryos. These embryos are frozen and later implanted into the transplanted uterus after it has healed.
5. Surgical Procedure: The uterus is transplanted into the recipient, connecting the blood vessels and ensuring proper blood flow. This is a complex surgery as the uterus is highly dependent on blood flowfor successful implantation and pregnancy.
6. Post-Transplant Care: The recipient must take immunosuppressive medicationsto prevent rejection of the transplanted uterus. Regular monitoring is crucial to ensure the uterus is functioning well.
7. Embryo Transfer: After ensuring the uterus is stable and functional, typically around 1.5 years after transplantation, the previously created embryos are transferred to the uterus to initiate pregnancy.
8. Pregnancy Monitoring: The pregnancy must be closely monitored to ensure the health of both the mother and the fetus. Any complications related to the transplant or immunosuppressive drugs need to be addressed immediately.
9. Hysterectomy: After the birth of one or two children, the transplanted uterus is usually removed via hysterectomy. This is done to avoid the long-term risks associated with taking immunosuppressive drugs.
Procedure
- Uterine transplantation starts with the uterus retrieval surgery on the donor. Working techniques for this exist for animals, including primates and more recently humans.
- The recovered uterus may need to be stored, for example for transportation to the location of the recipient. Studies on cold-ischemia/ perfusion indicate an ischemic tolerance of more than 24 hours.
- The recipient has to look at potentially three major surgeries. First of all, there is the transplantation surgery. If a pregnancy is established and carried to viability a cesarean section is performed. As the recipient is treated with immuno-suppressive therapy, eventually, after completion of childbearing, a hysterectomy needs to be done so that the immuno-suppressive therapy can be terminated.
SURGERY AND VASCULAR ANASTOMOSIS
- Procurement (technique similar to radical hysterectomy).
- Dissection of ureters.
- Isolation of arterial supply: isolation of the uterus with bilateral, long venous, and arterial vascular
- pedicles.
- Back table preparation.
- Vascular anastomosis: end-to-side bilateral vascular anastomoses.
- Connect the uterine veins to the external iliac veins (with 8-0 polypropylene sutures).
- Connect the anterior divisions of the internal iliac arteries to the external iliac arteries (with 7-0 polypropylene sutures).
- Ensure that good pulses existed distal to the arterial anastomosis sites and that the uterine tissue changed from pale to reddish, which is a sign of peripheral tissue perfusion.
- Blood flow : 40 mL per min.
Fig 1, Fig 2
FIXATION OF TRANSPLANTED UTERUS
- Vaginal rim anastomosis.
- Round ligaments.
- the extensive bladder peritoneum on the uterine graft on top of the recipient’s bladder to provide extra structural support.
- Avoid spontaneous labor
PREVENTION OF ISCHEMIA (COLD/WARM) – REPERFUSION INJURY
Cold ischemia at ex vivo preservation of graft leads to energy depletion, membrane polarity change, and major damage. Warm ischemia and reperfusion cause organelle destruction and inflammation. Metabolic stabilization occurs after 3 hours of ischemia.
Rejection in Uterine Transplantation
After transplantation, the risk of organ rejection is a significant concern. Each organ type has a different rejection risk, with the uterus presenting unique challenges:
- In uterine transplants, there is no specific blood marker that can indicate declining uterine function or rejection, making it difficult to detect until significant damage occurs.
- Subclinical (hidden) episodes of rejection can only be diagnosed through biopsies, as the uterus can be accessed easily via the vagina for cervical biopsies. These biopsies do not interfere with the uterine cavity, making it possible to monitor rejection even during pregnancy.
- In a specific case in Saudi Arabia, Doppler ultrasound, MRI, and blood tests (CD4/CD8 ratio) were used to monitor rejection. The patient showed early signs of acute rejection such as fatigue, fever, and vaginal discharge. After increasing immunosuppressive treatment and administering antithymocyte globulin, the rejection episode resolved.
Criteria for Uterine Transplantation
The recipient must:
- Be a genetic female with uterine absence and no medical contraindications.
- Have no other feasible options (such as surrogacy or adoption) due to legal or personal reasons.
- Be psychologically stable and informed of the risks involved.
The donor must:
- Be a healthy woman of reproductive age who has completed childbearing or consented to donate after death.
- Be free of coercion, have a good understanding of the process, and be mentally competent.
Donor Selection Criteria
Donors can be either living or deceased. The ideal donor must:
- Be younger than 45 years old and healthy.
- Be a multiparous woman (has had children).
- Be brain-dead but stable if deceased.
- Have no major health issues, normal blood tests, and matched blood and HLA types.
- Be negative for HPV, CMV, HIV, and viral hepatitis.
- Have no uterine abnormalities like myomas (fibroids) or vascular issues.
Immunosuppressive Protocol
To prevent rejection, the recipient undergoes two phases of immunosuppression:
1. Induction Phase:
- Anti-thymocyte globulin and prednisolone to reduce immune response.
2. Maintenance Phase:
- A combination of tacrolimus, mycophenolate mofetil, and azathioprine (switched to avoid teratogenic risks before embryo transfer).
The recipient is also at risk of life-threatening fungal infections, such as Candida and Aspergillus, which can affect multiple organs and have high mortality rates.
Post-Transplant Complications and Pregnancy
- Maintaining a healthy pregnancy is critical, requiring close monitoring to ensure:
- No malformations in the newborn.
- No deterioration of graft function in the mother.
Future Prospects of Uterine Transplantation
Advances in the field may include:
- Laparoscopic and robotic-assisted surgeries to reduce risks and shorten surgical times.
- Organ engineering technologies that could one day allow for the use of decellularized organs or synthetic matrices, potentially eliminating the need for immunosuppression.
- Continued development of psychological support protocols to ensure patients are emotionally and mentally prepared for the complexities of the procedure.
This innovative procedure offers new hope for women with Absolute Uterine Factor Infertility and represents a growing field with exciting future possibilities.
Conclusion
Uterine transplantation offers a revolutionary solution for women with Absolute Uterine Factor Infertility, providing them the opportunity to experience pregnancy and childbirth. However, it is a complex procedure that requires careful patient selection, meticulous surgical technique, long-term follow-up, and a deep consideration of the ethical implications. With proper care, women with AUFI may now have a chance to become mothers, a possibility that was once unattainable.
Reference
1. Barbor M. Cancer and Fertility Preservation Will New Laws Leave Patients Without Options - The ASCO Post. [ Nov; 2023 ]. https://ascopost.com/issues/october-10-2022/cancer-and-fertility-preservation-will-new-laws-leave-patients-without-options/ https://ascopost.com/issues/october-10-2022/cancer-and-fertility-preservation-will-new-laws-leave-patients-without-options/
2. Uterus transplantation as a therapy method in Mayer-Rokitansky-Küster-Hauser syndrome. Georgopapadakos N, Manoli A, Passia G, Skandalakis PN, Filippou D. Cureus. 2019;11:0. doi: 10.7759/cureus.6333. [DOI] [PMC free article] [PubMed] [Google Scholar]
3. The history behind successful uterine transplantation in humans. Castellón LA, Amador MI, González RE, Eduardo MS, Díaz-García C, Kvarnström N, Bränström M. JBRA Assist Reprod. 2017;21:126–134. doi: 10.5935/1518-0557.20170028. [DOI] [PMC free article] [PubMed] [Google Scholar]
4. Uterine transplant: This prospect for pregnancy is not worth the risks | Your Pregnancy Matters | UT Southwestern Medical Center. [ Nov; 2023 ]. http://utswmed.org/medblog/uterine-transplant-motherhood/ http://utswmed.org/medblog/uterine-transplant-motherhood/
5. Ethical aspects of uterus transplantation [Article in Czech] Chmel R, Nová?ková M, Pastor Z, Mat?cha J, ?ekal M, Fron?k J. https://pubmed.ncbi.nlm.nih.gov/28264580/ Cas Lek Cesk. 2017;156:36–42. [PubMed] [Google Scholar]
6. Ethical issues in uterine transplantation. Koplin JJ, Kendal E. Korean J Transplant. 2020;34:78–83. doi: 10.4285/kjt.2020.34.2.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
7. Ethical and policy issues raised by uterus transplants. O'Donovan L, Williams NJ, Wilkinson S. Br Med Bull. 2019;131:19–28. doi: 10.1093/bmb/ldz022. [DOI] [PMC free article] [PubMed] [Google Scholar]
8. Ethical considerations in uterus transplantation. Woessner JR, Blake VK, Arora KS. Medicoleg Bioeth. 2015;5:81–88. [Google Scholar]
9. Uterine Transplant Program. [ Nov; 2023 ]. https://www.hopkinsmedicine.org/gynecology-obstetrics/specialty-areas/uterine-transplant
https://www.hopkinsmedicine.org/gynecology-obstetrics/specialty-areas/uterine-transplant
10. Psychosocial outcomes of uterine transplant recipients and partners up to 3 years after transplantation: results from the Swedish trial. Järvholm S, Dahm-Kähler P, Kvarnström N, Brännström M. Fertil Steril. 2020;114:407–415. doi: 10.1016/j.fertnstert.2020.03.043. [DOI] [PubMed] [Google Scholar]

Figure 1
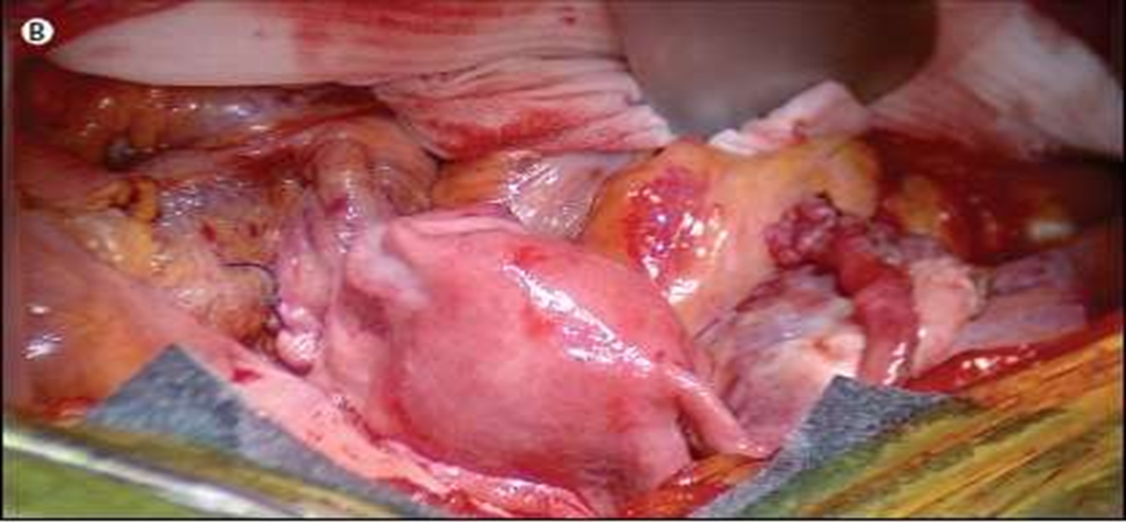
Figure 2
