Treatment of Proximal Phalanx Fractures with Long-Term Objective Results
Treatment of Proximal Phalanx Fractures with Long-Term Objective Results
Dr Kassem El Houcheimi *, Dr. Sanjay Kumar Sureen*, Dr. Vinod Kumar Singhal1
Dr. Vinod Kumar Singhal, consultant General Surgeon, Prime Hospital, Dubai.
*Correspondence to:
Dr Kassem El Houcheimi, FACS, MBA, Orthopedic surgeon, Clemenceau Medical Center Dubai.
Dr. Sanjay Kumar Sureen, Specialist Orthopaedic Surgeon, Prime Hospital, Dubai.
Copyright
© 2024 Dr Kassem El Houcheimi, Dr. Sanjay Kumar Sureen. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 03 Oct 2024
Published: 01 Nov 2024
DOI: https://doi.org/10.5281/zenodo.14160400
Abstract
This study presents the preferred methods for treating proximal phalanx fractures and their long-term outcomes. Between October 2001 and March 2010, 23 patients with 32 proximal phalanx fractures were treated in the Plastic Reconstructive and Aesthetic Surgery Department of Düzce Medical Faculty. Stable fractures were treated with splints, while unstable fractures were stabilized with 1.0 mm percutaneous intramedullary Kirschner wires. At follow-ups, patients were evaluated for radiologic efficiency, range of motion, total active movements, and grip power of the digit. Results showed perfect TAM scores for 20 fingers, good scores for 7 fingers, and moderate or poor scores for 5 fingers. A major complication was non-union in one finger. The study concluded that Kirschner wire fixation is a reliable and simple method for treating unstable proximal phalangeal fractures, with excellent long-term results in suitable cases.
Treatment of Proximal Phalanx Fractures with Long-Term Objective Results
Introduction
The most common fractures in the skeleton occur in the small tubular bones of the hands and feet, with phalangeal fractures being the most common. Distal phalanx fractures are the most common among phalangeal fractures, followed by proximal phalanx (PP) fractures. PP fractures are twice as common as those of the middle phalanx. A prospective study was conducted between October 2001-March 2010, involving 69 patients with 88 hand fractures.
To diagnose PP fractures effectively, the mechanism and force of the trauma should be queried in the initial examination. The study found that PP fractures can be divided into four categories: condyle, neck, shaft, and base. Other parameters important for PP fractures include displacement, stability, involvement of joints, type of fracture, and associated soft tissue injury.
Stable and nondisplaced PP fractures can be effectively managed by protective splinting and early controlled mobilization. However, each patient and fracture type has its own characteristics, so each fracture should be assessed individually. Unstable and nondisplaced PP fractures should be managed with fixation, as angulated fractures are considered unstable and require open reduction and fixation. Nondisplaced intraarticular PP fractures are highly unstable and susceptible to displacement, and early mobilization may cause their displacement.
Bicondylar fractures are almost always multiple fractures and require open reduction, while pilon fractures are multiple fractures in proximal interphalangeal (PIP) joints. If open reduction and fixation are not possible, traction-closed reduction or dynamic external fixation devices can be options. Restoration of movement is usually unpredictable in such cases, so restoration of the primary structure should be preferential. Dynamic external fixation devices are hinged and span the PIP joint to allow early protected ROM while maintaining joint reduction.
There is a consensus about treating displaced PP fractures with open reduction and internal fixation. Present lacerations secondary to injury can be used for access to the fracture line, and ligamentous and soft tissue attachments should be preserved. Fracture lines are fixed with one or multiple Kirschner wires (K-wire) or screws, and the PIP joints are held in nearly full extension to prevent collateral ligament and volar plate contracture.
Materials and Methods
This study analyzed the treatment choices and results of a group of patients with broken fingers, ranging in age from 5 to 78 years. The most common cause of these fractures was work-related accidents (56%), followed by home accidents (21%). Six patients (26%) suffered from right hand injury, while 17 patients (74%) suffered from left hand injury. The first and second fingers were the most commonly injured, with 32 fractures observed. Ten (31%) of the 32 fractures were intraarticular, and 22 (69%) were extraarticular. One patient had a fracture line extending between the PIP and metacarpophalangeal (MCP) joints. Eleven patients had associated metacarpal or middle or distal phalangeal fractures. The most common soft tissue injury associated with PP fractures was extensor tendon injury (34%). Other soft tissue injuries associated with PP fractures included flexor tendon, digital artery and digital nerve injuries, and skin defects that required reconstruction with a flap or a graft.
The study found that the extent of comminution of PP fractures did not preclude the use of K-wires in any of the patients. Twenty-seven of the 32 fractures were unstable and treated with open reduction, K-wire fixation, and splinting. Five of the 32 fractures were treated with closed reduction and splint application.
Fig1: A proximal phalanx shaft fracture was found in the left hand, causing dislocation of the IP joint. The fracture was treated with a transverse K-wire and an extensor polyplicis longus tendon injury was repaired. Postoperative X-ray views were also taken.
Fixations were achieved with 1 mm percutaneous intramedullary K-wires, with two K-wires used for fixation when one K-wire did not provide enough stability. A splint was used for all patients, and elevation was recommended. Postoperatively, follow-up radiographs were taken to verify adequate reduction, and if there was a suspicion of inadequate reduction during the operation, intraoperative scopy was used. Empiric oral sulbactam-ampicillin treatment was usually administered postoperatively. K-wires were removed between 4-6 weeks, and Coban® bandage was applied to the fingers to control edema. Physiotherapy was started just after the removal of the K-wires. In the long-term evaluations, the following parameters were considered: total active movement (TAM), PIP or IP joint and MCP joint ROM, and the function of the hand and the injured finger (grip strength).
Fig2: A displaced oblique proximal phalanx shaft fracture in the right hand 3rd finger was treated with 2 oblique K-wires, resulting in excellent bone healing in the 8th year, as shown in preoperative, early, and late postoperative X-ray views.
Results
The study evaluated the radiological efficiency of reduction, total active movement (TAM) of the finger, ROM of the joints, and grip strength of the injured finger in patients aged 3 months to 9 years. After surgery, radiological efficiency was determined immediately, and when inadequate or poor reduction was present, reduction and fixation were repeated. The mean time for radiological bone healing was 6 weeks, with complete bone union in fracture lines taking approximately 4 months.
All patients were discharged from the hospital on the same day of the operation, and after bone healing was completed, K-wires were removed in an outpatient setting and controlled mobilization started immediately. No infection was observed in any of the cases.
The mean TAM score of 25 PP fractures in the 2nd, 3rd, 4th, and 5th fingers was 205.5° (normal: 260°). The mean ROM value of PIP (or IP) and MCP joints was 72° (mean ROM for MCP joints with PP fractures of 1st finger was 74%, and 71% for MCP joints with PP fractures of other fingers was 71%). Intraarticular PP fractures extending into the MCP joint were observed in 5 out of 32 fingers, with mean ROM for 2 MCP joint intraarticular PP fractures of the 1st finger being 62.5°, 77°, and 71° for these 5 fingers.
In long-term follow-ups, the grip strength of the broken fingers was compared with that of healthy fingers, and no difference was observed. In one patient, nonunion occurred, and bone ends were debrided again, and fixation was re-achieved with K-wire. Complete bone healing was achieved in the follow-up, and angulations occurred in 2 patients but did not interfere with normal finger function. There was no pain on fracture lines, and arthrodesis was applied in 2 patients with intraarticular PP fractures extending into the PIP joint. All patients were satisfied with the results.
Fig 3: The first metacarpal bone was reconstructed using a radial osteocutaneous pedicled flap and fixed with a plate-screw, but postoperatively, screws were observed to have extruded.
Fig 4: A patient had a comminuted T-fracture in the left hand 4th finger, unstable displaced extraarticular proximal phalanx shaft fracture in the 5th finger, and unstable displaced middle phalanx shaft fracture in the 3rd finger. The fractures were treated with K-wires. A second K-wire was used for further reduction and fixation, but its comminuted nature was unsuitable for additional placement. Good bone healing was observed in the postoperative 2nd year. Preoperative, early, and late postoperative X-ray views were used.
Fig 5: The patient had unstable displaced proximal phalanx shaft and base fractures extending to the MCP joint in the left hand 4th finger, extraarticular proximal phalanx shaft fracture in the 5th finger, and unstable displaced middle phalanx shaft fracture extending to the DIP joint in the 3rd finger in the postoperative 2nd year. The patient showed minimal angulation at the 5th finger and no extension deficit, with excellent ROM and TAM evaluations.
Discussion
The study focuses on the treatment of phalangeal (PP) fractures, which are the most common among phalanx and metacarpal fractures. The type of injury is mostly open unstable fracture complicated with soft tissue injury such as tendon, nerve or artery injury, or skin loss. The treatment of PP fractures is based on the presentation of the fracture, degree of displacement, and difficulty in maintaining fracture reduction. A wide array of treatment options exists for the variation in fracture patterns observed. Inherently stable fractures do not require surgical treatment; all other fractures should be considered for additional stabilization.
Many combinations of internal fixation are possible; K-wires and screw-and-plate fixation predominate. Plate fixation is used in comminuted PP and lag screws in spiral long oblique phalanx shaft fractures. Screw-and-plate fixation is used in metacarpal fractures in a limited number due to its disadvantages such as the requirement of extensive dissection over the phalanx or metacarpal, formation of a large bulk under the tendon, and the possibility of inadequate stabilization using microplates. Additionally, in some cases, the screws are extruded.
Complications after plate fixation of 64 phalangeal fractures in 54 consecutive patients and their outcome were assessed. Stiffness (TAM <180°) contributed the highest number (22 patients, 24 fractures). The authors thought that the undue amount of scarring and adhesion may arise from the implant itself or the difficulty in finding the perfect mixture between minimal surgical invasiveness and a sufficient restoration of skeletal stability. Otherwise, plate fixation of unstable and complex phalangeal fractures provided efficient and reliable results.
Al-Qattan et al. reported 78 male workers with displaced unstable transverse fractures of the PP shaft. They divided the patients into two groups according to the treatment applied. Group 1 (n=40) was treated with closed reduction and percutaneous K-wires, while Group 2 (n=38) was treated with open reduction and interosseous loop wire fixation. At the final follow-up, Group 2 had significantly better overall TAM scores than Group 1. The complication rate was higher in Group 1 than Group 2, but the difference did not reach statistical significance.
Sorene et al. reported a retrospective study of the non-operative treatment of displaced avulsion fractures of the ulnar base of the PP of the thumb. The study included 28 thumbs that were stable to lateral stress testing at the time of the initial investigation. The patients were treated by immobilization of the thumb in a spica cast.
Horton et al. randomly divided patients with an isolated spiral or long oblique fracture of the PP into two groups. Outcome measures, including radiological adequacy of reduction, total active ROM, development of joint contracture, grip strength, and digital grip strength, were assessed. Good or excellent results were obtained in 76% of fractures (19 of 25).
Elmaraghy et al. presented a retrospective review of 35 digits in 24 patients with unstable fractures of the PP treated using the technique of percutaneous transmetacarpal intramedullary K-wire fixation. In our cases, we used splint only when the fracture line was stable. In case of unstable fractures, we definitely used K-wire.
The study found that radiographic healing is not correlated well with clinical healing. The average time for clinical union was 5-7 weeks for the middle portion of the PP and up to 10-14 weeks for transverse fractures of the exceedingly hard cortical portion of the middle phalanx. Clinical healing occurred between 4-6 weeks. Complications such as malunion, nonunion, loss of movement, infection, or tendon rupture were observed in 32 PP cases. In late-term follow-ups, no significant angulation or rotation interfering with the finger's function was observed.
Conclusion
We concluded that Kirschner wire fixation is a reliable and technically simple method for treating unstable PP fractures, and results in long-term good or excellent results in appropriately selected patients. In stable PP fractures, it was observed that cast splint provides adequate treatment.
References
1. Dick HM, Carlson EC. Fractures of the fingers and thumb. In: Smith JW, Aston SJ, editors. Grabb and Smith’s plastic surgery. Boston: Little, Brown and Company; 1991. p. 909-16.
2. Stanton JS, Dias JJ, Burke FD. Fractures of the tubular bones of the hand. J Hand Surg Eur Vol 2007;32:626-36.
3. Stern PJ. Fractures of the metacarpals and phalanges. In: Green DP, Hotchkiss RN, Pederson WC, editors. Green’s operative hand surgery. New York: Churchill Livingstone; 1993. p. 711-71.
4. Koman LA, Coonrad R, Poehling GG. Sprains and dislocations of the fingers and thumb. In: Smith JW, Aston SJ, editors. Grabb and Smith’s Plastic Surgery. Boston: Little, Brown and Company; 1991. p. 889-907.
5. Henry MH. Fractures of the proximal phalanx and metacarpals in the hand: preferred methods of stabilization. J Am Acad Orthop Surg 2008;16:586-95.
6. Kurzen P, Fusetti C, Bonaccio M, Nagy L. Complications after plate fixation of phalangeal fractures. J Trauma 2006;60:841-3.
7. Al-Qattan MM. Closed reduction and percutaneous K-wires versus open reduction and interosseous loop wires for displaced unstable transverse fractures of the shaft of the proximal phalanx of the fingers in industrial workers. J Hand Surg Eur Vol 2008;33:552-6.
8. Sorene ED, Goodwin DR. Non-operative treatment of displaced avulsion fractures of the ulnar base of the proximal phalanx of the thumb. Scand J Plast Reconstr Surg Hand Surg 2003;37:225-7.
9. Horton TC, Hatton M, Davis TR. A prospective randomized controlled study of fixation of long oblique and spiral shaft fractures of the proximal phalanx: closed reduction and percutaneous Kirschner wiring versus open reduction and lag screw fixation. J Hand Surg Br 2003;28:5-9.
10.Elmaraghy MW, Elmaraghy AW, Richards RS, Chinchalkar SJ, Turner R, Roth JH. Transmetacarpal intramedullary Kwire fixation of proximal phalangeal fractures. Ann Plast Surg 1998;41:125-30.
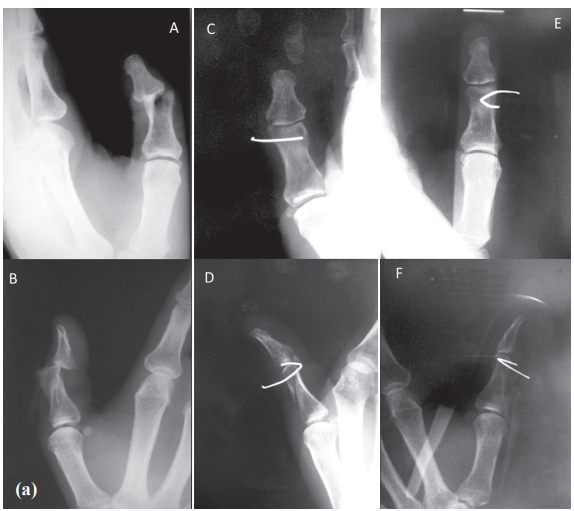
Figure 1
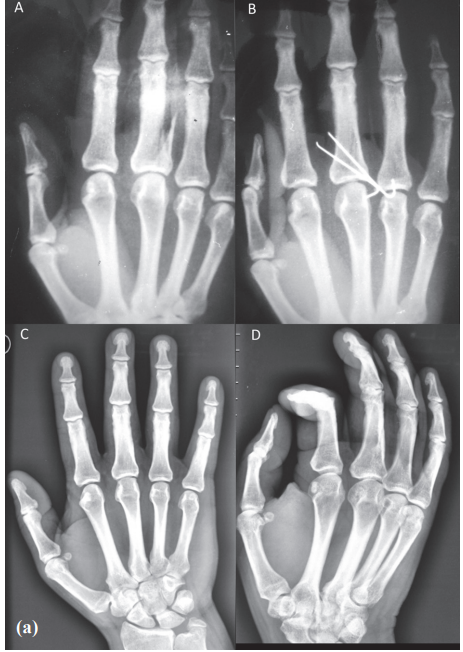
Figure 2

Figure 3
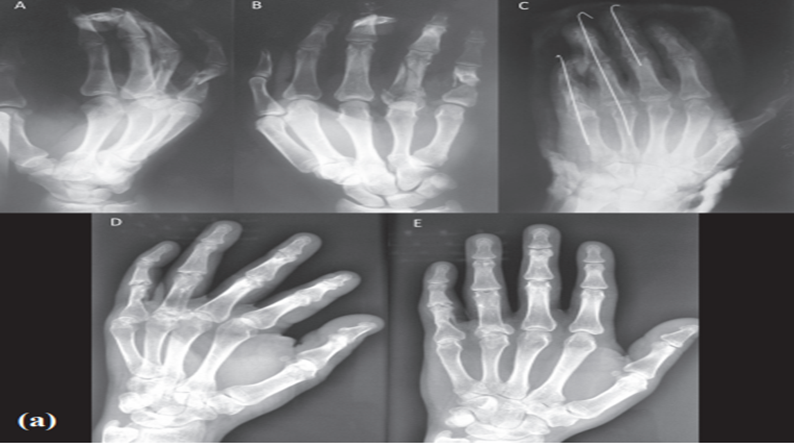
Figure 4

Figure 5
