A Prospective Comparative Study of Lateral Approach vs Posterior Approach in Bipolar Hemiarthroplasty in Rural Setup
A Prospective Comparative Study of Lateral Approach vs Posterior Approach in Bipolar Hemiarthroplasty in Rural Setup
Dr Durgaprasad H Devihosur1*, Dr Bavithran S2, Dr Praveen Ravindra Hegde3, Dr Guruprasad S4
1,2,3,4. Department of Orthopaedics, Gadag Institute of medical sciences, Gadag.
*Correspondence to: Dr Durgaprasad H Devihosur, Senior Resident, Gadag Institute of medical sciences, Gadag.
Copyright
© 2024 Dr. Durgaprasad H Devihosur. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 23 Oct 2024
Published: 01 Nov 2024
DOI: https://doi.org/10.5281/zenodo.14051294
Abstract
Objectives: To assess and compare the functional outcome of lateral and posterior approaches in fracture neck of femur treated with bipolar prosthesis at tertiary centre in rural setup. To compare the intraoperative blood loss, duration of surgery and complications between mentioned group.
Materials and methods: A total of 41 patients admitted in Gadag Institute of Medical Sciences under the department of Orthopaedics who have suffered from fracture neck of femur fracture from June 2023 – December 2024 were assigned to the study by systemic random sampling. patients in both groups were coompared for fracture pattern, co-morbidities, intraoperative assessment such as blood loss, duration and post op complications. Functional outcome was assessed using Harris Hip Score at 1 month, 3 month and 6 month.
Results: The mean harris hip score was similar in both groups, high chances of nerve injury leading to foot drop and dislocation was higher in posterior group.average duration of surgery lateral approach- 83 mins; posterior- 95mins Average blood loss lateral approach- 4.8mops posterior approach -5 mops
Conclusion: There is no significant statistcal difference in both approaches at 1 month, 3month and 6 month. Both the surgeries are good options for displaced neck of femur fractures and can be used as surgeons preference.
Keywords- Fracture neck of femur, Hardinge approach, posterior
A Prospective Comparative Study of Lateral Approach vs Posterior Approach in Bipolar Hemiarthroplasty in Rural Setup
Introduction
The neck of femur fracture is one of the common fractures in elderly. It hasbeenalways a challenge to the Orthopaedic surgeons to manage these fractures. Theprevalence of neck of femur fractures has increasing with increased incidenceof osteoporosis, poor vision in elderly, poor neuro muscular coordination, life stylechanges, sedentary habits, improvement in life expectancy. The burden of neckof femurfractures and its sequelae continued to be on the rise [1]. The treatment goal for thisfracture is restoring of functions without morbidity, still controversy exists inmanagement of neck of femur fracture in elderly and consume a potential propotionofour resources [2]a.
The introduction of unipolar prosthesis by Thompson in 1954 & Austin Moorein1957toreplace the femoral head ushered in the era of hemiarthroplasty and as standardtreatment for neck of femur fractures in elderly patients [3,4]a. With higher chanceof non union & avascular necrosis in internal fixation, hip arthroplasty has becomethebesttreatment choice in elderly for early mobilization and reduce morbidity. CurrentlytheOrthopaedic surgeons can choose between unipolar, bipolar and total hip replacementin the treatment of intracapsular fractures in elderly. The problemwith unipolar prosthesis seen were like acetabular erosion, stem loosening. In 1974, bipolar prosthesis was introduced by bateman which had mobile head element and hadadditional head surface to allow movement within acetabulum. This reduces theerosionin acetabulum and reduction in pain and incidence of protrusion. The motionoccursbetween metal head and polyethylene socket (inner bearing) as well as betweenmetallic head and acetabulum (outer bearing)[5]a.
The best approach for the hip joint arthroplasty, however remains controversial but recently some new less invasive modifications have been described and comparedtothe standard approches like anterior, anterolateral, posterior and lateral approaches. This study is to compare the outcomes of bipolar hemiarthroplasty performedbylateral and posterior approach.
Materials and Methods
Elderly patients admitted in Gadag Institute of Medical Sciences under thedepartment of Orthopaedics who have suffered from fracture neck of femur fracturewho fall under the inclusion criteria after clinical and radiological assessment. After informing the patient about diagnosis & all treatment options available and therelativemerits and demerits of each of the options, the patients willing to undergo bipolar hemiarthroplasty for displaced neck of femur fracture are explained the expectedfunctional improvement associated adverse outcomes and specific surgical complications of hemiarthroplasty are discussed with the patient. The patient wouldbesubjected to preoperative general examination and investigations as detailedbelow. Fitness from cardiologist was taken if deemed necessary If patient is found tobefit forsurgery, written consent for the surgery and the study is taken. The patient was subjected to the proposed intervention- bipolar hemiarthroplasty under subarachanoidblock or epidural anaesthesia..
Surgical technique:
Posterior approach
With the hip flexed approximately 45 degrees, a straight incision is madeapproximately 10 cm distal to the posterior superior iliac spine and extend it distallyandlaterally parallel with the fibres of the gluteus maximus to the posterior marginof thegreater trochanter. Direct the incision distally 10 to 13 cm parallel with the femoral shaft.Incise the fascia lata on the lateral aspect of the femur to uncover the vastus lateralis. Lengthen the fascial incision superiorly in line with the skin incision, and split thefibersof the gluteus maximus by blunt dissection There is no true internervous planeinthisapproach. However, the gluteus maximus, which is split in the line of its fibers, isnot significantly denervated because it receives its nerve supply well medial to thesplit. Retract the fibers of the split gluteus maximus and the deep fascia of the thigh. Underneath is the posterolateral aspect of the hip joint, still covered by the short external rotator muscles, which attach to the upper part of the posterolateral aspect ofthe femur Internally rotate the hip to put the short external rotator muscles onastretch(making them more prominent) and to pull the operative field farther fromthesciaticnerve Insert stay sutures into the piriformis and obturator internus tendons just beforethey insert into the greater trochanter.
Detach the muscles close to their femoral insertion and reflect thembackward, laying them over the sciatic nerve to protect it during the rest of the procedure. (Theupper part of the quadratus femoris may also have to be divided to fully exposetheposterior aspect of the joint capsule, but the muscle contains troublesome vesselsthatarise from the lateral circumflex artery. Normally, it should be left alone.) The posterioraspect of the hip joint capsule is now fully exposed. The hip joint capsule canbeincisedwith a longitudinal or T-shaped incision... Posterior joint capsulotomy will haveexposedthe femoral head and neck.
Fig 1
Direct Lateral approach
Make a posteriorly directed lazy-J incision centered over the greater trochanter. Divide the fascia lata in line with the skin incision and centered over the greater trochanter Retract the tensor fasciae lata anteriorly and the gluteus maximus posteriorly, exposing the origin of the vastus lateralis and the insertion of the gluteusmedius. Incise the tendon of the gluteus medius obliquely across the greater trochanter, leaving the posterior half still attached to the trochanter. Carry the incision proximallyinline with the fibers of the gluteus medius at the junction of the middle and posterior thirds of the muscle. Placing the abductor "split" more anterior, directly over thefemoral head and neck. This gluteus medius split should be no farther than 4 to 5 cmfromthetip of the greater trochanter to avoid damage to the superior gluteal nerve andartery. Distally, carry the incision anteriorly in line with the fibers of the vastus lateralisdowntobene along the anterolateral surface of the femur. Elevate the tendinous insertionsofthe anterior portions of the gluteus minimus and vastus lateralis .Abduction of thighexposes the anterior capsule of the hip joint . Incise the capsule as required . Limbplaced in figure of four position , and head extracted . During closure , repair thetendonof gluteus medius with non absorbable braided suture.
Post operative protocol
a. Patients pulse, blood pressure, respiration, temperature was monitored b. Limb elevation over pillow and patient kept under observation in recovery roomuntil stable then shifted to ward
c. IV antibiotics were continued for first 3 days followed by oral antibiotics andanalgesic for another 1 week
d. Blood transfusion was given depending on the requirement e. Dressing changed on 2nd, 5th and 14th post operative day f. Sutures removed on 14th post operative day
g. Static quadriceps exercises were started on 1st postoperative day. h. Active quadriceps and knee flexion exercises were started on 3rd postoperativeday. i. Patients were advised to walk with partial weight bearing as soon as tolerable. j. Full weight bearing walking was allowed after assessing for radiological andclinical union
Follow up
Radiological examination was repeated postoperatively and patients werefollowed up at 1 month , 3 months and 6 months. Healing is judged clinically bothbypain and motion at fracture site. At each follow up , X ray of operated hip anteroposterior is taken and Harris hip score is assessed. Parameters assessedarepain , shortening, range of hip and knee movements and walking ability with or withoutsupport.
Results
|
APPROACHES |
N |
Mean |
Std.Deviation |
Std.ErrorMean |
|
|
|
Lateral |
20 |
55.9000 |
8.41615 |
1.88191 |
|
FOLLOW_UP_1 |
|
|
|
|
|
|
|
Posterior |
21 |
56.0952 |
5.98251 |
1.30549 |
|
|
Lateral |
20 |
78.8000 |
4.87313 |
1.08966 |
|
FOLLOW_UP_2 |
|
|
|
|
|
|
|
Posterior |
21 |
76.8095 |
4.46787 |
.97497 |
|
|
Lateral |
20 |
86.7500 |
3.46220 |
.77417 |
|
FOLLOW_UP_3 |
|
|
|
|
|
|
|
Posterior |
21 |
86.0952 |
3.04803 |
.66513 |
|
|
Lateral |
20 |
74.4500 |
4.66200 |
1.04245 |
|
Average |
|
|
|
|
|
|
|
Posterior |
21 |
73.4286 |
3.64104 |
.79454 |
|
|
Lateral |
20 |
3.2500 |
.44426 |
.09934 |
|
BLOOD_LOSS |
|
|
|
|
|
|
|
Posterior |
21 |
3.9048 |
.62488 |
.13636 |
|
|
Lateral |
20 |
83.9500 |
4.81746 |
1.07722 |
|
DURATION_OF_SURGERY |
|
|
|
|
|
|
|
Posterior |
21 |
95.6667 |
5.03322 |
1.09834 |
Frequency Table
|
|
t-testforEqualityofMeans |
|||
|
t |
df |
Sig.(2-tailed) |
MeanDifference |
|
|
FOLLOW_UP_1 |
-.086 |
39 |
.932 |
-.19524 |
|
FOLLOW_UP_2 |
1.364 |
39 |
.180 |
1.99048 |
|
FOLLOW_UP_3 |
.644 |
39 |
.524 |
.65476 |
|
Average |
.784 |
39 |
.438 |
1.02143 |
|
BLOOD_LOSS |
-3.849 |
39 |
.000 |
-.65476 |
|
DURATION_OF_SURGERY |
-7.608 |
39 |
.000 |
-11.71667 |
Sex
|
|
Frequency |
Percent |
|
|
|
MALE |
27 |
65.9 |
|
Valid |
FEMALE |
14 |
34.1 |
|
|
Total |
41 |
100.0 |
Diagnosis
|
|
Frequency |
Percent |
|
|
|
Leftsideneckoffemur fracture |
21 |
51.2 |
|
Valid |
Rightsideneckoffemur fracture |
13 |
31.7 |
|
|
Rightsideneckoffemur fracture |
7 |
17.1 |
|
|
Total |
41 |
100.0 |
Approaches
|
|
Frequency |
Percent |
|
|
Valid |
Lateral |
20 |
48.8 |
|
|
Posterior |
21 |
51.2 |
|
|
Total |
41 |
100.0 |
General Linear Model
Descriptive Statistics
|
APPROACHES |
Mean |
Std.Deviation |
N |
|
|
|
Lateral |
55.9000 |
8.41615 |
20 |
|
FOLLOW_UP_1 |
Posterior |
56.0952 |
5.98251 |
21 |
|
|
Total |
56.0000 |
7.17983 |
41 |
|
|
Lateral |
78.8000 |
4.87313 |
20 |
|
FOLLOW_UP_2 |
Posterior |
76.8095 |
4.46787 |
21 |
|
|
Total |
77.7805 |
4.71970 |
41 |
|
|
Lateral |
86.7500 |
3.46220 |
20 |
|
FOLLOW_UP_3 |
Posterior |
86.0952 |
3.04803 |
21 |
|
|
Total |
86.4146 |
3.23246 |
41 |
Tests of Within Subjects Effects
Measure: Merasure 1
|
Source |
TypeIII Sumof Squares |
df |
MeanSquare |
F |
Sig. |
|
Change |
20153.165 |
2 |
10076.582 |
685.069 |
.000 |
|
Change*APPROACHES |
24.872 |
2 |
12.436 |
.845 |
.433 |
|
Error(Change) |
1147.290 |
78 |
14.709 |
|
|
T- Test
Group Statistics
|
SEX |
N |
Mean |
Std.Deviation |
Std.ErrorMean |
|
|
|
MALE |
27 |
62.0000 |
9.08507 |
1.74842 |
|
AGE |
|
|
|
|
|
|
|
FEMALE |
14 |
63.9286 |
9.39283 |
2.51034 |
Discussion
The most common treatment for a displaced neck of femur fracture in elderly is hemiarthroplkasty. In a metaanalysis of randomised controlled trials by Cecilia Rogmark, comparing hip replacement with internal fixation in displaced femoral neck fractures, has clearly shown that for major method-related complications as well as for reoperations with open surgery, there is an advantage to performing hip replacements with an odds ratio of about 0.12 with a tight confidence limit. One concern has been increased mortality. After 30days, there was an odds ratio of 1.30 but no significant difference in mortality. After 1 year, the mortality was the same in both groups. There was various approaches described for hip arthroplasties. The best approach for hip arthroplasty , hopwever remains controversial recently some less invasive modifications have been described and compared to the standard approaches such as posterior, lateral, anterolateral and anterior. We undertook the present study to evaluate the immediate result of comparitive study of posterior and lateral approach in hemiarthroplasty in elderly population in rural setup.
Age incidence: The mean age of the our study was 63 years, and other studies which were comparable inculde
|
CLINICAL STUDIES |
MEAN AGE IN YEARS |
|
M.T.Hongisto et.al |
82.8 |
|
S Mukka et.al |
78.3 |
|
Roland Biber et.al |
80.4 |
|
The current study |
63 |
Complications
In our case study in the posterior group there was 1 complication which was postoperative and there was no complication in lateral group.
in our study there was less blood loss in lateral approach group compared to the posterior group and less operative time lateral approach group compared to the posterior group.In our study the post operative hip dislocation was seen in 1 patient and mortality of the same patient.
Here are some of the complications of the similar clinical trials.
|
Clinical studies |
Dislocation in percentage
|
|
|
Posterlateral approach
|
Posterior approach |
|
|
in our study |
5 |
0 |
|
M.T.Hongisto et.al |
3.4 |
0 |
|
S Mukka et.al |
6 |
1 |
|
Roland Biber et.al |
3.9 |
0.5 |
There were no surgical site infection in our study. Here are some similar clinical trials which show result as follows.
|
Clinical studies |
SSI rate in percentage |
|
|
Posterior approach
|
Lateral approach |
|
|
Firat ozan et.al |
7.4 |
3.4 |
|
Svenoy et.al |
6 |
5 |
|
Roland Biber et.al |
2.5 |
3.2 |
|
In our study |
NIL |
NIL |
Fuctional outcome
In our study the functional outcome was assessed by Harris Hip Score
In our study among the lateral group 2 patients had good outcome, 16 had fair outcome and 2 had poor outcome.In our study among the posterior group 1 patients had good outcome, 18 had fair outcome and 2 had poor outcome. In both the groups the patients improved over the period and there was no statistical difference among two groups.
In our study there was no significant difference with repect to performing day to day activities, pain and walking aid requiremnents. But 3 patients complained of abductor weakness in the 2 follow up in lateral group.
Conclusion
Fracture neck of femur in elcommon is more common due to self fall. Average duratioon of time, blood loss are less in lateral approach compared to posterior approach, and intraoperative and postoperative complications were seen in posterior group. However there was no significant difference in functional outcome on subsequent followups.
The end result depended upon the age of the patient, post operative physiotherapy, associated co-morbidities. Both lateral and posterior approach are good options for hemiarthroplasty for displaced fracture neck in elderly and can also be a surgeons preference.
References
1. Schmidt AH, Swiontkowski MF. Femoral neck fractures. Orthop Clin NorthAm 2002;33(1):97-111
2. Mark F. Simontkoski et.al. Current concepts review of intracapsular fracture of hip.JBJS 1994;76A:129-135
3. Robert W.B, James D.H. Rockwood Green's Fracture in Adults, %th Edition. Lippincot Williams & Wilkins, 2001
4. Austin T Moore: The self locking metallic hip prosthesis.JBJS 1957;39A:811-27
5. Austin T Moore and H.R. Bohlman: Metallic hip joint, A case report. JBJS1963; 25:688-92.
6. Bateman J.E : Single assemply total hip arthroplasty , preliminary report. Orthop DIgest 1974;15:35-43.
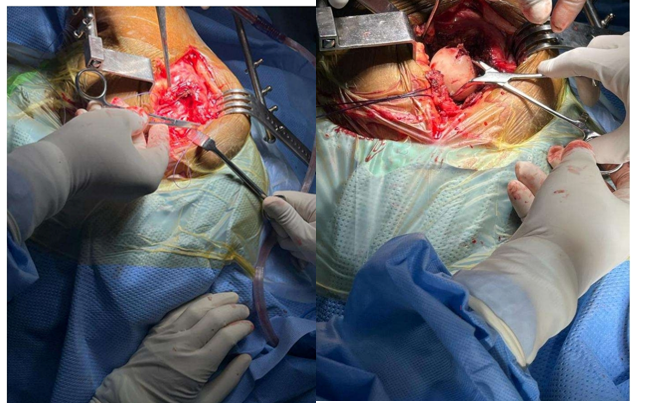
Figure 1
