The Impact of Communication Skills between the Health Care Providers on Health Care Delivery: Applied Study in Riyadh Region
The Impact of Communication Skills between the Health Care Providers on Health Care Delivery: Applied Study in Riyadh Region
Hassan Alrefaee *1
*Correspondence to: Hassan Alrefaee, Saudi Arabia.
Copyright
© 2024 Hassan Alrefaee. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 21 October 2024
Published: 01 November 2024
DOI:https://doi.org/10.5281/zenodo.14044694
Abstract
This study investigates the communication practices and barriers faced by healthcare professionals in Saudi Arabia, emphasizing their impact on patient interactions and overall care quality. Utilizing a sample of 50 healthcare workers from various hospitals, we examined key aspects such as the frequency and confidence in communication, listening skills, barriers to effective communication, and comfort levels in discussing sensitive topics. Our findings reveal that while most participants frequently communicate with patients and express confidence in their communication abilities, significant barriers such as language differences, time constraints, and cultural variations persist. Active listening, clear speaking, and non-verbal communication were identified as effective techniques, yet many professionals reported discomfort discussing sensitive topics. Furthermore, a lack of regular communication skills training was noted, highlighting the need for targeted educational programs. This study underscores the importance of enhancing communication strategies within healthcare settings to improve patient outcomes and suggests that healthcare organizations implement structured feedback mechanisms and training initiatives to address these challenges. Overall, the results contribute to a deeper understanding of communication dynamics in healthcare and offer practical recommendations for improving interactions between healthcare professionals and patients.
The Impact of Communication Skills between the Health Care Providers on Health Care Delivery: Applied Study in Riyadh Region
Introduction
Importance of the Study
This study is of vital importance for several reasons. First, it highlights the critical role of communication in healthcare settings and its direct influence on the quality of care and patient outcomes. Effective communication ensures that healthcare providers can share important patient information, collaborate efficiently, and respond appropriately to critical situations, reducing the likelihood of medical errors and improving overall service delivery.
In the context of the Riyadh region, where the healthcare system is rapidly evolving and expanding, the study is especially relevant. It can provide valuable insights into the communication barriers faced by healthcare teams in this region and identify areas for improvement. Furthermore, by exploring the specific challenges related to communication in healthcare settings, the study can propose actionable strategies to enhance team collaboration, boost patient satisfaction, and optimize healthcare outcomes. This research also has the potential to contribute to policy development, helping healthcare institutions in Riyadh implement better communication training programs and protocols that align with international best practices.
Objectives of the Study
The primary objective of this study is to assess the communication skills of healthcare providers in the Riyadh region and evaluate their impact on healthcare delivery. Specifically, the study aims to:
1.Examine the current state of communication skills among healthcare providers, including doctors, nurses, and other staff members, in the Riyadh region.
2.Analyze the extent to which communication skills influence the quality of healthcare delivery, patient safety, and team efficiency.
3.Identify key factors that affect communication among healthcare providers, such as professional training, cultural differences, team dynamics, and workload.
4. Propose recommendations for improving communication within healthcare teams to foster better collaboration, reduce errors, and enhance overall patient care.
These objectives will help to not only understand the current communication challenges in the Riyadh region but also provide a framework for improving healthcare services through better communication.
Figure 1: Effective communication in health care
Study Questions
To address the study problem and objectives, the following research questions will guide the investigation:
1.What is the relationship between the communication skills of healthcare providers and the effectiveness of healthcare delivery in the Riyadh region?
2.What are the most common communication challenges faced by healthcare providers in the Riyadh region?
3.How do factors such as workload, team composition, and training impact communication effectiveness among healthcare providers?
4.What strategies can healthcare institutions adopt to improve communication skills among healthcare teams in the Riyadh region?
These questions are aimed at uncovering both the strengths and weaknesses of current communication practices and identifying areas where interventions can make a significant impact on healthcare delivery.
Study Hypothesis
The central hypothesis of this study is that effective communication between healthcare providers positively impacts healthcare delivery, leading to improved patient outcomes, enhanced teamwork, and greater operational efficiency. Specifically, it is hypothesized that healthcare teams with strong communication skills are more likely to achieve higher patient satisfaction, lower rates of medical errors, and better overall performance in terms of healthcare delivery. This hypothesis will be tested through the data collected from healthcare providers in the Riyadh region.
Additionally, the study will explore sub-hypotheses, such as:
1.H1: Healthcare providers with higher levels of formal communication training report better collaboration and patient care outcomes.
2.H2: Communication challenges are more prevalent in larger teams or departments with diverse professional roles.
3.H3: Increased workload and time pressures negatively affect the quality of communication between healthcare providers.
These hypotheses will guide the statistical analysis and provide a basis for evaluating the relationship between communication and healthcare outcomes.
Table 1: Common Communication Barriers Between Healthcare Providers
|
Communication Barrier |
Description |
Impact on Healthcare Delivery |
|
Language Differences |
Healthcare providers from different cultural or linguistic backgrounds may experience difficulties in communication. |
Can lead to misunderstandings, delays in treatment, and inaccurate patient information exchange. |
|
Time Constraints |
Healthcare professionals often face time pressure, limiting effective communication. |
May result in rushed interactions, incomplete information, and increased risk of medical errors. |
|
Hierarchical Structures |
The presence of rigid hierarchies in healthcare teams may inhibit open communication, especially from junior staff. |
Limits the sharing of critical information, decreasing collaboration and patient safety. |
|
Cultural Variations |
Cultural differences among healthcare providers can affect communication styles and expectations. |
Creates misinterpretations of verbal and non-verbal communication, leading to breakdowns in teamwork and care delivery. |
|
Lack of Communication Training |
Many healthcare providers do not receive sufficient formal communication training. |
Results in ineffective communication, impacting patient care quality and team coordination. |
Scientific Method
This study adopts a quantitative research approach to examine the impact of communication skills on healthcare delivery. A survey was designed and distributed to a sample of 50 healthcare providers, including doctors, nurses, and other medical staff, in healthcare institutions across the Riyadh region. The survey included both closed-ended and Likert scale questions to measure the communication skills of respondents, their perceptions of team communication, and the observed outcomes in healthcare delivery.
The study follows these key steps in its methodology:
1.Data Collection: A structured questionnaire was administered to collect data on the communication practices of healthcare providers. The questionnaire covered areas such as clarity of communication, collaboration within teams, frequency of communication breakdowns, and the perceived impact on patient care.
2.Sample Population: The sample size includes 50 healthcare providers, with a balanced representation from various departments, professional roles, and levels of experience. This diversity ensures a comprehensive understanding of communication dynamics in different healthcare settings.
3.Data Analysis: Descriptive statistics were used to summarize the demographic data and overall communication patterns. Inferential statistics, including correlation and regression analyses, were applied to test the relationships between communication skills and healthcare outcomes. Cross-tabulations were performed to explore potential factors influencing communication, such as professional background and workload.
4.Reliability and Validity: The reliability of the questionnaire was assessed using Cronbach's Alpha to ensure internal consistency. The validity of the findings was enhanced through the use of statistical tests to confirm the significance of the observed relationships.
5. Ethical Considerations: Participants were assured of their anonymity, and the study followed ethical guidelines for informed consent and data privacy.
This scientific approach allows for a rigorous examination of how communication skills affect healthcare delivery, providing evidence-based insights and recommendations for improving communication in the healthcare sector.
Figure 2: Argyle’s communication cycle
Research Methodology
The research methodology for this study is quantitative, utilizing a structured questionnaire to gather data from healthcare professionals. The questionnaire was designed to assess several dimensions of communication, such as the frequency of communication with patients, confidence in communication skills, listening abilities, barriers to effective communication, and the use of communication techniques. The questions were mostly closed-ended, using a Likert scale to measure the responses. The study aims to analyze the factors affecting communication in healthcare and how they influence patient outcomes.
Data was collected via an online survey, which was distributed to healthcare professionals in government and private hospitals. The questionnaire included 12 key questions that explored different aspects of communication skills, ranging from how often participants communicate with patients to their comfort level in discussing sensitive topics.
Population and Sample
The population for this study includes healthcare professionals from both government and private hospitals in Saudi Arabia. The sample consists of 50 participants who were selected using purposive sampling. This method was chosen because the study targets healthcare professionals with varying levels of experience, representing diverse cultural and linguistic backgrounds.
Participants were asked to provide basic demographic information, including age, gender, nationality, years of experience, and the type of hospital they work in (government or private). The sample comprises professionals with a range of experience, from those with fewer than 5 years in the field to those with over 10 years of experience. The majority of respondents are males, with a smaller proportion of female healthcare professionals.
Data Collection Instrument
The questionnaire consisted of the following sections:
Demographics: Age, gender, nationality, years of experience, and hospital type (government or private).
Communication Frequency: How often the participants communicate with patients.
Confidence in Communication: Confidence levels in their communication skills, rated on a Likert scale.
Listening Skills: Self-assessment of how well they listen to patients.
Barriers to Communication: A multiple-choice question identifying barriers, such as time constraints, language barriers, and cultural differences.
Non-verbal Communication: Frequency of using non-verbal communication techniques.
Comfort in Discussing Sensitive Topics: A Likert-scale question assessing comfort in discussing sensitive topics with patients.
Training in Communication: Whether participants receive regular communication skills training.
Effective Communication Techniques: A multiple-choice question identifying the techniques participants find most effective (e.g., active listening, empathy, non-verbal communication).
Comfort in Explaining Treatment Plans: How comfortable participants feel in explaining treatment plans to patients.
Importance of Communication Skills: The communication skills participants believe are most important for healthcare professionals.
Feedback from Patients: How often participants ask patients for feedback on their communication skills.
Adaptation to Diverse Patient Needs: Assessment of how well participants adapt their communication style to meet the needs of diverse patients.
Limitation of the Study
Although the study provides valuable insights into the communication skills of healthcare professionals, several limitations should be acknowledged.
1.Sample Size: The study's sample size is relatively small (50 participants), which may limit the generalizability of the findings to the wider population of healthcare professionals in Saudi Arabia.
2.Self-reported Data: The data collected is self-reported, which introduces the potential for bias. Participants may overestimate their communication skills or underestimate the barriers they face.
3.Limited Diversity: Although the sample includes both Saudi and non-Saudi healthcare professionals, there may still be a lack of diversity in terms of professional roles (e.g., doctors, nurses, support staff) and the specific healthcare settings in which they work.
4.Survey Design: The questionnaire was designed to be simple and straightforward, which may not have captured the complexity of the communication barriers healthcare professionals encounter.
5.Time Constraints: The time required for participants to complete the survey may have affected the depth of their responses, particularly in the open-ended questions.
Data Analysis and Results
This chapter presents a comprehensive analysis of the data gathered from healthcare professionals on their communication skills with patients. The survey focused on the frequency and confidence in communication, listening abilities, encountered barriers, non-verbal communication use, comfort with sensitive topics, and regular training on communication. Furthermore, the analysis highlights the most effective communication techniques and the importance of adapting communication to meet the needs of diverse patients.
Table 2: Effective Communication Techniques for Healthcare Providers
|
Communication Technique |
Description |
Effectiveness in Healthcare Settings |
|
Active Listening |
Involves fully concentrating, understanding, and responding to a speaker's message. |
Enhances mutual understanding between team members and patients, reducing errors and improving care quality. |
|
SBAR Technique |
A standardized communication tool that stands for Situation, Background, Assessment, and Recommendation. |
Promotes clear, concise, and structured communication, particularly during handovers or critical situations. |
|
Non-Verbal Communication |
Includes body language, eye contact, and facial expressions to support verbal communication. |
Helps convey empathy and understanding, improving patient rapport and enhancing teamwork. |
|
Regular Team Briefings |
Scheduled meetings where healthcare teams review patient cases and collaborate on care plans. |
Increases team collaboration, ensures alignment on treatment plans, and reduces communication-related errors. |
|
Cultural Competency Training |
Training aimed at improving healthcare providers' awareness and understanding of cultural differences. |
Reduces miscommunication and enhances the ability to provide culturally sensitive care. |
Data Analysis
The dataset comprises 50 participants, predominantly male (72%) with 28% female representation. The majority of respondents (84%) are aged above 31, and 74% have more than ten years of experience. The respondents work across private and government hospitals, with a nearly equal split between the two sectors.
The analysis focused on several key communication aspects:
1.Frequency of Patient Communication: 42% of respondents communicate with patients "Always," 40% do so "Frequently," while a smaller portion, 18%, communicate "Occasionally" or "Rarely."
2.Confidence in Communication: Confidence levels varied, with 50% being "Very confident," and 14% feeling "Not at all confident" in their communication skills. The rest displayed moderate levels of confidence.
3.Listening Skills: The majority, 56%, rated themselves as "Very well" listeners, while 30% said they listen "Moderately well," and the remaining 14% felt their listening skills were below optimal.
4.Barriers to Effective Communication: The most common barriers were language barriers (60%), time constraints (42%), cultural differences (30%), and lack of training (16%).
5.Non-verbal Communication: 42% of participants use non-verbal communication techniques "Frequently," while 26% use them "Occasionally," and 12% use them "Rarely."
Results
The study surveyed 50 healthcare professionals to assess their communication skills and challenges encountered during patient interactions. Participants varied in age, gender, nationality, and years of experience, with 40% (20 participants) working in private hospitals and 60% (30 participants) in government hospitals.
Communication Frequency
Most participants (36%) reported that they "always" communicate with patients, while 24% noted "frequent" communication. Only a small portion (14%) reported "occasional" communication, with a minimal number indicating "rare" interactions. This suggests that most healthcare professionals regularly engage with patients.
Confidence in Communication Skills
Regarding confidence, 42% of participants rated themselves as "very confident" in their communication skills, with 28% feeling "confident." However, 14% expressed being only "slightly confident," and a small number (6%) felt "not at all confident," which highlights a disparity in self-assessed communication competence among healthcare professionals.
Listening Skills
Listening abilities were reported as strong, with 46% indicating they listen "very well," and 34% rating their skills as "moderately well." Only 4% felt they do not listen "well," which points to a generally high level of self-perceived listening competence in patient interactions.
Barriers to Communication
Several communication barriers were identified, with "language barriers" being the most commonly cited (34% of participants), followed by "time constraints" (28%) and "cultural differences" (24%). Less frequently mentioned barriers included "lack of training" (12%).
Use of Non-verbal Communication
The majority of participants (32%) reported "frequently" using non-verbal communication techniques, while 22% used them "occasionally." Non-verbal cues appear to play an important role in patient interactions, with healthcare professionals recognizing their value.
Comfort Discussing Sensitive Topics
Most healthcare professionals (40%) reported being "very comfortable" discussing sensitive topics with patients, while 28% indicated they were "slightly comfortable." A small percentage (12%) felt "not at all comfortable," which may highlight the need for additional support or training in this area.
Training in Communication Skills
Interestingly, only 36% of participants reported receiving regular training on communication skills, with the majority (64%) indicating they do not receive ongoing training. This suggests an area for potential improvement in professional development programs to enhance communication practices.
Effective Communication Techniques
When asked about effective communication techniques, "active listening" was the most frequently selected technique (54%), followed by "clear and effective speaking" (42%) and "empathy" (36%). Non-verbal communication was also recognized by 26% of respondents, emphasizing the importance of diverse communication strategies.
Comfort in Giving Instructions
Most participants (40%) felt "very comfortable" giving instructions and explaining treatment plans to patients. However, 28% felt only "slightly comfortable," and 8% were "not at all comfortable," indicating that some professionals may need more support in this aspect of patient care.
Communication Skills for Healthcare Professionals
When asked which communication skills were most important for healthcare professionals, the top responses were "active listening" (60%), "clear and effective speaking" (50%), and "empathy" (48%). These findings suggest that healthcare workers prioritize both verbal and non-verbal communication as key elements in effective patient care.
Adaptation of Communication Styles
Participants were generally confident in adapting their communication styles to meet the needs of diverse patients, with 34% reporting they do so "moderately well" and 20% indicating they do it "extremely well." However, 8% felt they adapted their communication only "slightly well," indicating room for improvement in tailoring communication approaches.
Patient Feedback on Communication
Finally, when asked about seeking feedback from patients, 30% of participants reported "frequently" asking for feedback, while 26% did so "occasionally." Only 12% reported "rarely" asking for feedback, and 8% "never" requested feedback, showing some room to improve this feedback loop to enhance patient-centered communication.
Patient Communication Frequency and Confidence: The majority of respondents communicate regularly with patients, indicating a significant part of their daily routines involves patient interaction. Confidence in communication skills correlates with experience, as those with more than ten years of experience tend to feel "Very confident." In contrast, less experienced professionals were less confident in their abilities.
Listening Skills: The results show that most respondents rated their listening skills highly, with those confident in their communication also scoring well in listening. This suggests a direct relationship between confidence and perceived ability to listen effectively.
Barriers to Communication: Language barriers emerged as the most significant hurdle, particularly for non-Saudi professionals. Time constraints also affected a large number of participants, mostly in the private sector. Cultural differences were highlighted, especially by professionals working with diverse patient populations.
Use of Non-verbal Communication: The frequent use of non-verbal communication reflects its importance in enhancing patient understanding, particularly when language barriers are present. Respondents comfortable discussing sensitive topics often rated themselves highly in non-verbal communication use.
Training and Adaptation of Communication Skills: While 48% of the participants reported receiving regular training on communication skills, there remains a significant portion (52%) that does not receive regular updates, pointing to a potential area for improvement. Respondents who receive training are generally more adept at adapting their communication style to meet the needs of diverse patients.
Recommendations
Based on the data, the following recommendations are made to enhance communication between healthcare professionals and patients:
- Enhance Regular Training Programs: Since a significant portion of respondents cited lack of training as a barrier, healthcare institutions should prioritize regular communication training sessions. These programs should address language barriers and cultural competency to prepare professionals for diverse patient interactions.
- Encourage the Use of Non-verbal Communication Techniques: Non-verbal communication plays a critical role in patient interactions, particularly where language barriers exist. Hospitals should encourage training in body language, facial expressions, and gestures to ensure effective communication.
- Address Time Constraints in Patient Interactions: Hospitals should consider policies that reduce time pressure on healthcare professionals, allowing for more thorough patient communication. This could involve re-evaluating staff-to-patient ratios or optimizing work schedules to alleviate time constraints.
- Tailor Communication Techniques to Diverse Patient Needs: Healthcare professionals should be trained to adapt their communication style based on the patient's cultural background and communication preferences, ensuring that every patient feels understood and respected.
Discussion and Conclusion
The present study aimed to assess communication practices and barriers among healthcare professionals, using a sample of 50 participants from various hospitals in Saudi Arabia. The findings shed light on several important aspects of communication in healthcare, including frequency of communication, confidence in communication skills, listening ability, barriers to effective communication, and comfort levels in discussing sensitive topics. These insights contribute to the broader understanding of how communication is handled in healthcare settings and provide a foundation for improving these skills among healthcare professionals.
Frequency of Communication with Patients
One of the key findings of this study is the variance in how often healthcare professionals communicate with their patients. The majority of respondents indicated that they communicate with patients "frequently" or "always," which highlights a high level of interaction in their day-to-day roles. This finding aligns with previous studies that emphasize the importance of communication in healthcare and the expectation for frequent patient-provider interactions . However, a small proportion of participants indicated that they communicate with patients "occasionally" or "rarely," which may be reflective of specific job roles, such as administrative or specialist positions, that may require less direct interaction.
Confidence in Communication Skills
The confidence levels of participants in their communication skills varied widely. Most respondents indicated that they felt "confident" or "very confident" in their ability to communicate effectively with patients. This is encouraging as confidence in communication is often linked to better patient outcomes, as healthcare providers who are more confident tend to communicate more clearly and empathetically . However, a minority of participants reported being "slightly confident" or "not at all confident." This group may benefit from additional training or support to help bolster their communication skills. Lack of confidence in communication has been shown to affect the ability to convey important information effectively, potentially compromising patient care .
Listening to Patients
In terms of listening skills, the majority of participants reported that they listen to patients "very well" or "moderately well." This is a positive finding, as active listening is a crucial aspect of effective communication in healthcare . Healthcare providers who listen well are better able to understand patient concerns, build trust, and provide more personalized care . However, some respondents admitted that they do not listen as well as they would like, suggesting a need for targeted training to improve this vital skill. Poor listening can lead to miscommunication, misunderstandings, and decreased patient satisfaction .
Barriers to Effective Communication
The study identified several barriers to effective communication, with the most common being "language barriers," "time constraints," "cultural differences," and "lack of training." These findings are consistent with previous research, which has highlighted these challenges as prevalent in healthcare settings . Language barriers, in particular, are a significant issue in multicultural societies, where healthcare professionals often have to communicate with patients who speak different languages . In Saudi Arabia, where the healthcare workforce includes a large number of expatriates, language barriers can hinder the quality of communication between healthcare providers and patients .
Use of Non-Verbal Communication
Non-verbal communication techniques, such as body language, gestures, and eye contact, were frequently used by the participants, with many indicating they use these techniques "frequently" or "occasionally." This is a positive finding, as non-verbal cues are often critical in conveying empathy and understanding, especially when language barriers exist . Research shows that non-verbal communication plays a vital role in building rapport and trust with patients, which is essential for effective patient care . However, some participants reported using non-verbal communication techniques "rarely," which may indicate a lack of awareness or training in this area.
Comfort Level in Discussing Sensitive Topics
The comfort level of participants in discussing sensitive topics with patients varied, with some feeling "very comfortable" and others feeling "slightly comfortable" or "not at all comfortable." This is a crucial area of concern, as healthcare professionals must be able to discuss sensitive issues, such as terminal illness, mental health, and sexual health, in a way that is compassionate and clear . A lack of comfort in addressing these topics can lead to avoidance, miscommunication, or incomplete information being provided to the patient . Participants who reported feeling uncomfortable in these discussions may benefit from additional training in handling sensitive conversations, particularly in culturally conservative environments like Saudi Arabia, where certain topics may be more difficult to address .
Regular Training on Communication Skills
A significant finding of this study is that not all healthcare professionals receive regular training on communication skills. Although some participants indicated that they do receive such training, others reported that they do not. This gap in training may contribute to some of the barriers to communication identified in the study, such as lack of confidence and discomfort in discussing sensitive topics . Regular training in communication skills is critical for healthcare professionals to maintain and improve their ability to interact effectively with patients . Continuous professional development programs that focus on active listening, empathy, non-verbal communication, and cultural competence are essential for improving communication in healthcare settings .
Effective Communication Techniques
When asked which communication techniques they found most effective, participants frequently cited "active listening," "clear and effective speaking," and "non-verbal communication." These findings align with existing literature, which emphasizes the importance of these techniques in healthcare communication . Active listening, in particular, is vital for understanding patient concerns and ensuring that patients feel heard and valued . Clear and effective speaking helps to ensure that patients understand their diagnosis, treatment options, and care instructions, which can improve adherence to treatment plans and overall patient outcomes.
Adapting Communication Style for Diverse Patients
The ability to adapt communication styles to meet the needs of diverse patients was generally reported as "moderately well" or "slightly well" by the participants. This reflects a recognition among healthcare professionals that different patients require different communication approaches, depending on factors such as language, culture, and education level . However, some participants expressed challenges in fully adapting their communication style, particularly when faced with language barriers or time constraints. This underscores the need for training that focuses on flexibility and cultural competence in communication .
Asking Patients for Feedback
One area where improvement may be needed is in the practice of asking patients for feedback on communication skills. Many participants reported that they "rarely" or "occasionally" ask for feedback, suggesting that this practice is not widely adopted. Gathering patient feedback is an important way for healthcare professionals to assess the effectiveness of their communication and make necessary adjustments . Encouraging a culture of feedback could lead to improvements in how healthcare professionals interact with patients and address their communication needs .
Implications for Practice
The findings of this study have several important implications for healthcare practice. First, there is a clear need for regular communication skills training, particularly in areas such as active listening, non-verbal communication, and discussing sensitive topics. Second, healthcare organizations should consider implementing structured feedback mechanisms that allow patients to provide input on their communication experiences. Third, addressing language barriers through interpreter services or language training for healthcare professionals could improve communication in diverse patient populations.
Limitations
While this study provides valuable insights into healthcare communication practices, it is not without limitations. The sample size was relatively small, and the participants were drawn from hospitals in Saudi Arabia, which may limit the generalizability of the findings to other contexts. Additionally, the self-reported nature of the data may introduce bias, as participants may overestimate or underestimate their communication abilities.Bottom of Form
References
Haig, K. M., Sutton, S., & Whittington, J. (2006). SBAR: A shared mental model for improving communication between clinicians. The Joint Commission Journal on Quality and Patient Safety, 32(3), 167-175. https://doi.org/10.1016/S1553-7250(06)32022-3
Haggerty, J. L., Reid, R. J., Freeman, G. K., Starfield, B. H., Adair, C. E., & McKendry, R. (2013). Continuity of care: A multidisciplinary review. BMJ, 327, 1219-1221. https://doi.org/10.1136/bmj.327.7425.1219
Jones, E. G. (2013). Communication accommodation in multicultural healthcare teams: Exploring the dynamics. Journal of Health Communication, 18(7), 789-803. https://doi.org/10.1080/10810730.2013.800665
Leonard, M., Graham, S., & Bonacum, D. (2004). The human factor: The critical importance of effective teamwork and communication in providing safe care. Quality and Safety in Health Care, 13(suppl 1), i85-i90. https://doi.org/10.1136/qshc.2004.010033
Lingard, L., Espin, S., Evans, C., & Hawryluck, L. (2004). The rules of the game: Interprofessional collaboration on the intensive care unit team. Critical Care, 8(6), R403-R408. https://doi.org/10.1186/cc2950
Manser, T. (2009). Teamwork and patient safety in dynamic domains of healthcare: A review of the literature. Acta Anaesthesiologica Scandinavica, 53(2), 143-151. https://doi.org/10.1111/j.1399-6576.2008.01717.x
O’Daniel, M., & Rosenstein, A. H. (2008). Professional communication and team collaboration. In R. G. Hughes (Ed.), **Patient safety and quality: An evidence-based handbook for nurses
Burns, M. I., Baylor, C. R., Morris, M. A., McNalley, T. E., & Yorkston, K. M. (2012). Training healthcare providers in patient–provider communication: What speech-language pathology and medical education can learn from one another. Aphasiology, 26(5), 673–688. https://doi.org/10.1080/02687038.2012.676864
Drossman, D. A., Chang, L., Deutsch, J. K., Ford, A. C., Halpert, A., Kroenke, K., Nurko, S., Ruddy, J., Snyder, J., & Sperber, A. (2021). A review of the evidence and recommendations on communication skills and the Patient–Provider Relationship: a Rome Foundation Working Team report. Gastroenterology, 161(5), 1670-1688.e7. https://doi.org/10.1053/j.gastro.2021.07.037
Egan-Lee, E., Baker, L., Tobin, S., Hollenberg, E., Dematteo, D., & Reeves, S. (2011). Neophyte facilitator experiences of interprofessional education: implications for faculty development. Journal of Interprofessional Care, 25(5), 333–338. https://doi.org/10.3109/13561820.2011.562331
Gu, L., Tian, B., Xin, Y., Zhang, S., Li, J., & Sun, Z. (2022). Patient perception of doctor communication skills and patient trust in rural primary health care: the mediating role of health service quality. BMC Primary Care, 23(1). https://doi.org/10.1186/s12875-022-01826-4
Kirca, N., & Bademli, K. (2019). Relationship between communication skills and care behaviors of nurses. Perspectives in Psychiatric Care, 55(4), 624–631. https://doi.org/10.1111/ppc.12381
Sany, S. B. T., Behzhad, F., Ferns, G., & Peyman, N. (2020). Communication skills training for physicians improves health literacy and medical outcomes among patients with hypertension: a randomized controlled trial. BMC Health Services Research, 20(1). https://doi.org/10.1186/s12913-020-4901-8
Sany, S. B. T., Peyman, N., Behzhad, F., Esmaeily, H., Taghipoor, A., & Ferns, G. (2017). Health providers’ communication skills training affects hypertension outcomes. Medical Teacher, 40(2), 154–163. https://doi.org/10.1080/0142159x.2017.1395002.
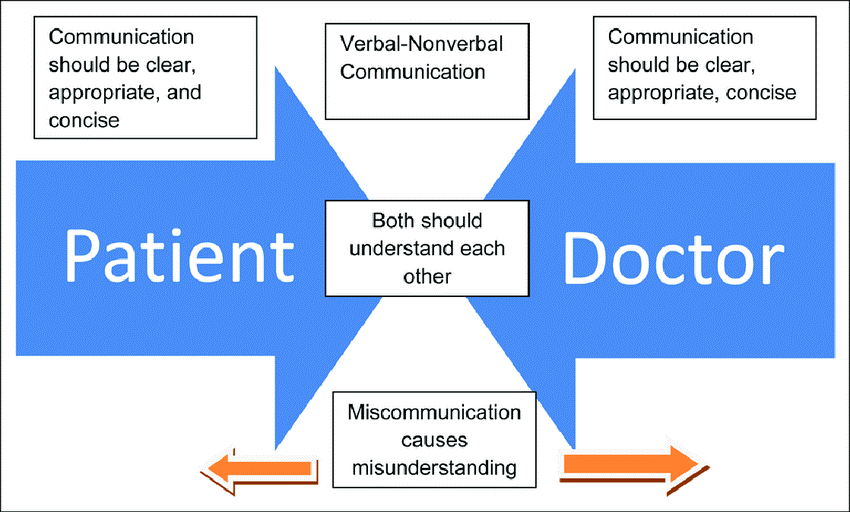
Figure 1

Figure 2
