13 Years Old with Severe Idiopathic Gastroparesis Showing Complete Recovery after a 6-Month Course of Pyridostigmine
13 Years Old with Severe Idiopathic Gastroparesis Showing Complete Recovery after a 6-Month Course of Pyridostigmine
Haifaa Alkabbani 1, Ahmed Saeed 2, Dr. Khaled Abouhazima 3*
1. Pediatric Resident, Sidra Hospital, Doha – Qatar.
2. Pediatric Gastroenterology and hepatology fellow, Sidra Hospital, Doha – Qatar.
*Correspondence to: Dr. Khaled Abouhazima, Pediatric Gastroenterology and hepatology Attending, Sidra Hospital, Doha – Qatar.
Copyright
© 2024: Dr. Khaled Abouhazima. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 24 Sep 2024
Published: 01 Nov 2024
DOI: https://doi.org/10.5281/zenodo.14064690
Abstract
This, the clinical odyssey of a previously healthy, 13 years old boy who was investigated and managed as a case of severe idiopathic gastroparesis and demonstrated complete recovery after a 6month course of pyridostigmine. No other known causes were identified. None is reported in the literature about developing this full-blown presentation in this age group and this is to highlight the clinical utilization of the Diagnostic standard 4-hours Gastric Emptying Study in diagnosis and follow-up and to report this remarkable recovery while drawing the need to standardize both test and treatment form management of such cases .
13 Years Old with Severe Idiopathic Gastroparesis Showing Complete Recovery after a 6-Month Course of Pyridostigmine
BACKGROUND
Gastroparesis can be debilitating especially for a growing teenager, and thought there are no known childhood rates, the growing impact is readily visible in hospitalizations and referrals (1) . High clinical suspicion in detecting the symptoms of early satiety , vomiting , abdominal pain and distention with elimination of other causes remains key to diagnosis along with a confirmatory Diagnostic standard 4-hours Gastric Emptying Study (2)
Causes for pediatric onset gastroparesis remain understudied, which means more questions are raised with each diagnosis. we also note that symptom control along with dietary support and prokinetics remain the main stay of treatment with varying Reponses as our case demonstrates.
Case Presentation
This is a 13-years-old male patient, previously healthy aside form a history of treated Pylori gastritis 4 years before he presented with a prolonged history of abdominal pain in the epigastric and umbilical area , No specific character. No aggravating factors. Associated with food intake and noted relief with vomits. He also complained of frequent bouts of vomiting, non-bilious and reaching up to 30 times per day the day of presentation. There were no associated symptoms like fever, constipation, bloody stool. he had started to lose weight as a result of the protracted symptoms.
On examination, the patient was looking sick and dehydrated, however, his vitals were within normal range, initial lab tests were done including CBC, electrolytes level, liver function test, renal function test and inflammatory markers (ESR and CRP) were reassuring with mild derangements.
Initial US Abdomen and surgical review cleared him from acute surgical causes and a first look upper GI scope showed the stomach was severely inflamed, mucosa was friable and bleeds easily, duodenum looked normal and Stool Pylori was positive, so patient was started on quadruple therapy and discharged home after improvement of symptoms. However, patient presented again to the ED with worsening symptoms and bilious vomiting after 2 weeks of h pylori eradication therapy. The patient was looking in moderate dehydration and the father mentioned weight loss of 5 kg in one month, so was admitted for further workup.
Investigations
During the admission, Upper GI radiography was done and it ruled out intestinal obstruction however it showed a transit time of contrast in the duodenum was delayed, after being repeated as the child was sever retching. Furthermore, CT scan / MR enterorrhaphy ruled out superior mesenteric artery syndrome and other masses or possible causes for the clinical picture. Physiatry and neurology reviews ruled out other possible non-GI related causes.
A second look Upper GI scope was done almost a month of admission and was normal, so a Diagnostic standard 4-hours Gastric Emptying Study was booked and it showed severely abnormal gastric emptying liquid phase study most supportive of gastroparesis. Electroesophegography was done as well keeping up with gastroparesis and it showed very dysrhythmic recording with mixed bradygasteria and tachygasteria. Investigations for the causes of the severe gastroparesis were all non-suggestive including genetic testing (combined Mito Genome Plus Focused Nuclear gene panel).
Image 1: Diagnostic standard 4-hours Gastric Emptying Study
Radiotracer activity is noted in the stomach and slowly progresses through the small bowel however with some liquid retention during the study indicating Severely abnormal gastric emptying liquid phase study most supportive of gastroparesis..There is no evidence of reflux during the acquisition.
Liquid gastric emptying at 1 hour is 16.82 %
Retention at 30 mn: 91.56 %
Retention at 60 mn: 83.18 %
Retention at 90 mn: 74.8 %
Retention at 4 hrs: 6 %
Treatment Course
The patient was persistently vomiting for weeks with decrease appetite and weight loss , despite good coverage with antiemetics and antiacids . he did’nt tolerate Nasogastric and Naso-jejenal feeds , and was started on total parenteral nutrition and a Gastrostomy tube was inserted to decompress the stomach as he the family requesting the keep on supplemental enteral feeds .
Erythromycin was started as prokinetic but stopped later as it did not help the patient or change hist tolerance. and so he was started on pyridostigmine (1.5 mg/kg/Day – divided BID Dosing via Gtube initially then shifted orally ) as a trial and his symptoms significantly improved, and After 4 months of admission, he was eventually discharged on oral feeds along with supplemental PN .
Follow up appointments showed complete clinical recovery and on demonstratable improvement of the Diagnostic standard 4-hours Gastric Emptying Study, pyridostigmine was stopped after 6 month, TPN was discontinued as he was achieving his caloric requirements on oral feeds and with good tolerance.
The patient is now 16 years old , and aside from 2 admissions with gastroenteritis , his severe symptoms didn’t recurre , gaining weight and enjoying home prepared table meals.
Image 2: Diagnostic standard 4-hours Gastric Emptying Study 6 weeks on Pyridostigmine
Radiotracer activity is noted in the stomach and slowly progresses through the small bowel. Demonstrating Markedly abnormal gastric emptying for liquids with notable improvement in comparison to recent examination.
There is no evidence of reflux during the acquisition
Liquid gastric emptying at 1 hour is 25.5%
Retention at 30 mn: 88%
Retention at 60 mn: 74.5%
Retention at 90 mn: 65.4%
Retention at 120 mn: 44.2%
Image 3: CDC weight for age chart tracking our case’s clinical course through recovery
Discussion
Idiopathic gastroparesis, in particular, poses a clinical challenge as the etiology remains unclear. The patient in this case experienced a severe clinical course, necessitating total parenteral nutrition (TPN) and gastric-jejunostomy (GJ) tube feeding, which emphasizes the extent of his gastrointestinal dysmotility.
The severity of presentation in pediatric idiopathic gastroparesis is variable, ranging from mild to severe symptoms such as persistent nausea, vomiting, abdominal pain, and poor nutritional intake. Several studies highlight that child with more severe presentations often require interventions such as enteral or parenteral nutrition due to failure of conventional medical therapies, similar to the case described here (4,5).
Pyridostigmine, an acetylcholinesterase inhibitor, has garnered attention as a novel therapeutic option for gastroparesis. It works by increasing the availability of acetylcholine at the neuromuscular junction, thereby enhancing gastrointestinal motility (6). The literature indicates an increasing number of pediatric and adult case reports documenting its efficacy in managing severe gastroparesis (7). The complete clinical recovery observed in the patient following the pyridostigmine trial mirrors similar cases where patients experienced significant symptom relief and improved gastric emptying times (8). Pyridostigmine, by enhancing cholinergic transmission, may help restore coordinated gastric motility, particularly in cases where neuromuscular dysfunction is suspected like cases of refractory idiopathic gastroparesis (6,9). The patient in this case tolerated the therapy well, and no significant adverse effects were noted throughout the treatment course.
Learning Points
This case contributes to the growing body of evidence supporting the use of pyridostigmine in managing severe pediatric gastroparesis. It highlights the potential for complete recovery, even in cases requiring aggressive supportive measures. Further research into the long-term outcomes and mechanisms of action of pyridostigmine in this patient population is warranted, but its role as a promising treatment option for severe cases of idiopathic gastroparesis is clear.
Contributors :Supervised by Dr. Khaled Abouhazima (Pediatric Gastroenterologist) ,. Report was co-written by (Pediatric Gastroentrology fellow , MBBS ,MSc, MD ) and Dr. Haifaa Alkabbani (Pediatric resident R3, MBBS)
Competing interests: None.
Funding: Open access funding provided by the Qatar National Library
Patient consent: Obtained.
References
1. Kovacic K, Elfar W, Rosen JM, Yacob D, Raynor J, Mostamand S, Punati J, Fortunato JE, Saps M. Update on pediatric gastroparesis: A review of the published literature and recommendations for future research. Neurogastroenterol Motil. 2020;32(3).
2. Maan El Halabi, Parkman HP. 2023 update on the clinical management of gastroparesis. Expert Rev Gastroenterol Hepatol. 2023;17(5):431-441
3. Sigurdsson L, Flores A, Putnam PE, Hyman PE, Di Lorenzo C. Postviral gastroparesis: presentation, treatment, and outcome. J Pediatr. 1997;131(5):751-754.
4. Bharucha AE, et al. Delayed gastric emptying in children: Epidemiology, clinical presentation, and diagnosis. J Pediatr Gastroenterol Nutr. 2015;61(4):446-455.
5. Parkman HP, et al. Gastroparesis: Clinical features, diagnosis, and treatment. Gastroenterology. 2019;156(5):1308-1321.
6.Mousa H, et al. Acetylcholinesterase inhibitors in pediatric gastroparesis. J Pediatr Gastroenterol Nutr. 2020;70(5):635-642.
7. Antiel RM, et al. Pediatric severe idiopathic gastroparesis: A retrospective case series. J Pediatr Surg. 2018;53(12):2395-2401.
8. Kuo B, et al. Pyridostigmine in the treatment of gastroparesis: A systematic review. Dig Dis Sci. 2021;66(7):2259-2271.
9. Abdallah H, et al. Pathophysiology of idiopathic gastroparesis and potential treatment with pyridostigmine. Neurogastroenterol Motil. 2022;34(1)
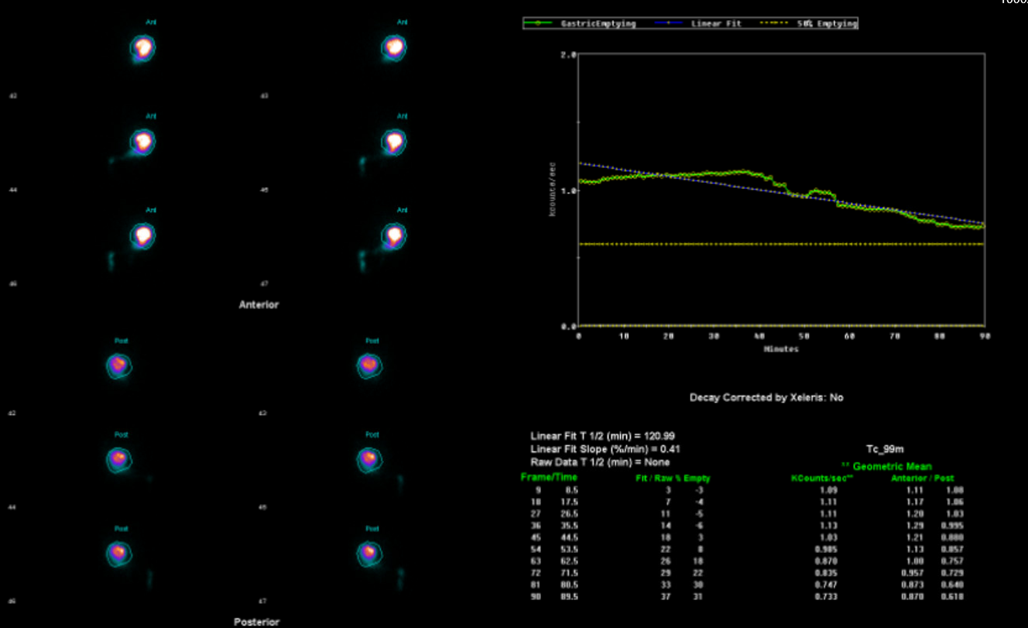
Figure 1
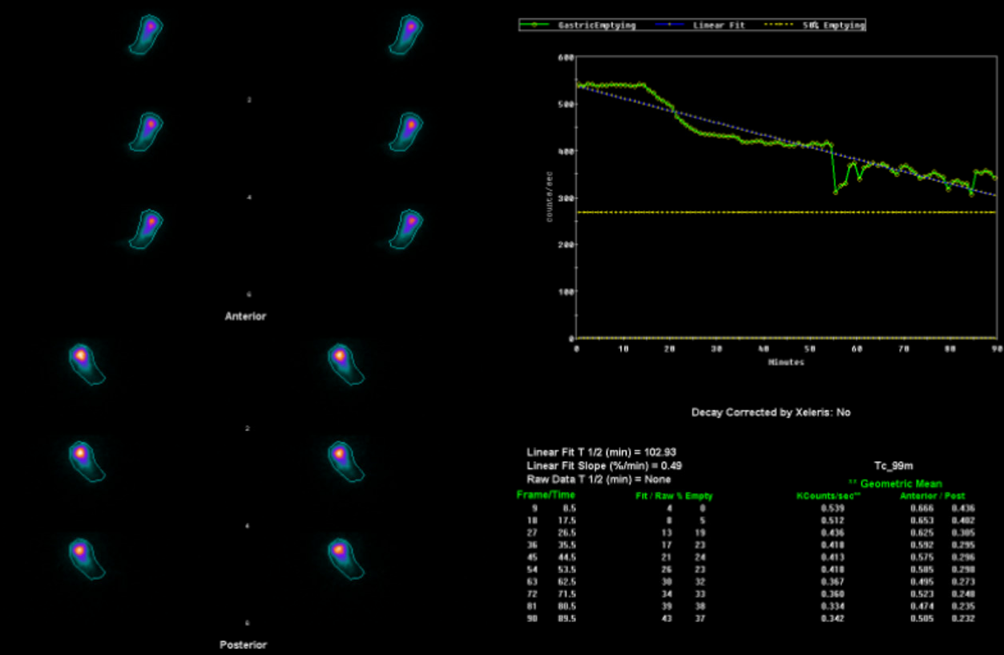
Figure 2
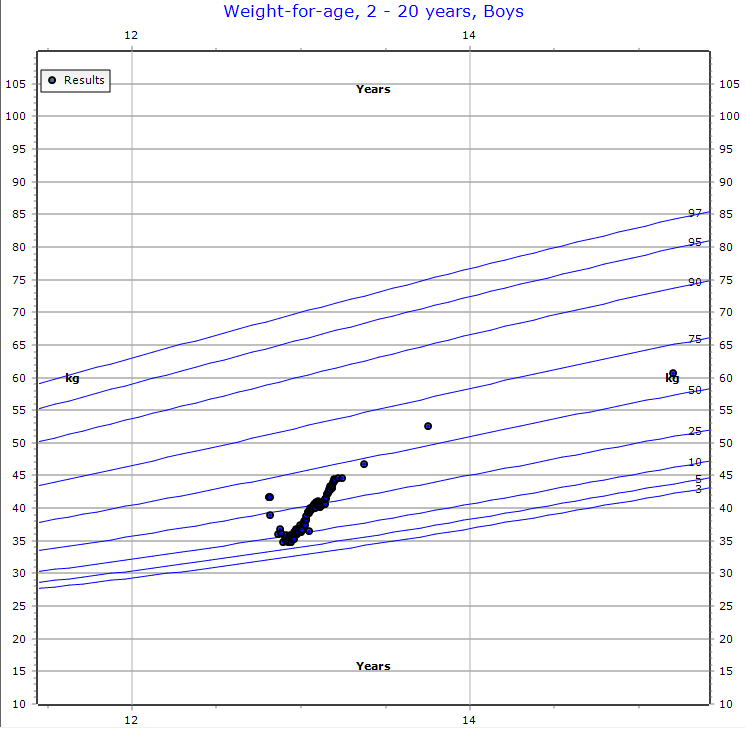
Figure 3
