Management of Vascular Injury Utilizing Aortic Covered Stent in a Child after Button Battery Ingestion
Management of Vascular Injury Utilizing Aortic Covered Stent in a Child after Button Battery Ingestion
Nicholas Houska DO 1, Barry O’Callaghan 2, Sarah A Basaham, MBBS, D. ABA 3, Sal H, Ratliff DO 4, Gareth J. Morgan MD 5, Richard J. Ing MBBCh FCA (SA) 6
1, 4,6. Department of Anesthesiology, The University of Colorado, Children’s Hospital Colorado, Aurora, Colorado, USA.
2 Department of Radiology, Saolta University Healthcare Group, University Hospital Galway, Galway, Ireland.
3. Department of Anesthesia and Critical Care, King Abdulaziz, University Hospital, Jeddah, Saudi Arabia.
5. Department of Cardiology, The University of Colorado, Children’s Hospital Colorado, Aurora, Colorado, USA.
*Correspondence to: Richard J Ing. Department of Anesthesiology. The University of Colorado. Children’s Hospital Colorado, 13123 E 16th Avenue, Aurora, CO 80045, 720-777-1234.
Copyright
© 2024 Richard J Ing. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 22 Sept 2024
Published: 01 Nov 2024
Abstract
The complications of ingested button batteries in children are related to the size of the ingested button battery, the age of the child, and the location of esophageal impaction. Damage to vascular structures such as the aorta and resulting hemorrhage remains one of the most severe complications. Delayed vascular injuries are possible even days following removal of button batteries. We report on the multidisciplinary anesthesiology and interventional cardiology management of a child with a severe esophageal injury with erosion adjacent to the aorta following ingestion and esophageal impaction of a button battery. Vascular injury was mitigated utilizing a percutaneously delivered aortic covered stent placed accurately with state-of-the-art vessel navigation.
Management of Vascular Injury Utilizing Aortic Covered Stent in a Child after Button Battery Ingestion
Introduction
Button batteries (BBs) are found in many households’ electronic equipment including children’s toys, remote controls, tracking devices and musical greeting cards. Manufacturing changes in 2006 led to larger 20 mm diameter and more powerful 3-volt lithium (BB) being introduced.1 These larger diameter batteries are more likely to become impacted in the esophagus if ingested and lead to severe complications in young children.2, 3 In children under six years old who ingest 20 mm batteries, the rates of major complications has been reported to be 12.6%.1 Button battery induced esophageal tissue injury begins to develop within 15 minutes of tissue contact and the risk of severe injury increases with the duration of button battery impaction. As many young children who ingest BBs are poor historians, may be non-verbal, and have a delay in presentation following ingestion, vascular imaging is often recommended as part of the work-up and clinical management decision making. Vascular imaging is important to determine the extent of injury to surrounding esophageal structures, and depending on the extent of injury, where the safest place in the hospital is to remove button batteries. In cases of unwitnessed ingestion, the severe complication rate is greater than 50%.4 Additionally, vascular preventative intervention via catheterization has limited representation in the scientific literature though its potential utility is acknowledged within the anesthesiology and interventional cardiology community.5, 6 A concern when caring for children who have ingested button batteries, is the possibility of delayed secondary vascular rupture, which can occur even up to 18 days after the successful removal of an esophageal impacted button battery.7 We present a case of severe esophageal injury following a button battery ingestion with extended tissue injury towards the aorta in a young child who then required an aortic covered stent to mitigate the risk of a delayed aortic bleed.
Case Report
We report the case of a previously healthy 8-year-old female patient weighing 26.4 kilograms. She presented to her local pediatric hospital emergency department with abdominal pain 14 hours after swallowing a 20 mm 1.5V Lithium button battery (BB) while jumping on a trampoline with the battery in her mouth. An abdominal radiograph was performed demonstrating the position of a circular radio-opaque foreign body in the distal esophagus, initially thought to be a coin. Repeat imaging the object was noted to have smooth edges with concern to be a button battery and the patient was transferred to a hospital with esophagoscopy capabilities. Twenty hours after ingestion she underwent removal of the BB with esophageal endoscopy under general anesthesia (GA). At this procedure a circumferential erosion in the lower ¼ of the esophagus was identified. She was transferred to the pediatric intensive care unit of our tertiary care center 24 hours after removal, prior to which she had one episode of blood-tinged emesis. She underwent repeat endoscopy under GA to define the extent of the injury and a black eschar was documented involving 50% of the distal anterior esophagus. (Figure 1) Twenty-four hours later she underwent a third GA for thoracic Magnetic Resonance Angiography (MRA) and a Computed Tomography Angiography scan to further evaluate for any extension of the esophageal erosion to surrounding critical structures.
Figure 1: Esophagoscopy showing eschar and erosion in the distal anterior esophagus.
Multisequence multiplanar magnetic resonance imaging examination of the chest was performed before and after the administration of intravenous gadolinium. There was evidence of enhancement and edema involving the wall of the esophagus just above the gastroesophageal junction. Additionally, adjacent blooming artifact was noted but no evidence of significant mediastinal enhancement. The aortic arch was of normal caliber without evidence of wall irregularity, aneurysm or dissection.
Helical Computed Tomography Angiography (CTA) of the chest was performed following the bolus intravenous administration of contrast. Circumferential esophageal wall thickening around the distal esophagus at the site of esophageal injury was seen. There was a linear arterial blush from the descending thoracic aorta into the posterior inflamed wall of the esophagus at the site of the esophageal injury. There was no mediastinal enhancement nor fluid. (Figure 2).
Figure 2: Helical Computed Tomography Angiography of the chest showing linear arterial blush from the descending thoracic aorta into the posterior inflamed wall of the esophagus at the site of the esophageal injury (green arrow).
Multidisciplinary discussion with pediatric cardiac anesthesia, interventional cardiology, gastroenterology, cardiothoracic surgery, and radiology resulted in a consensus decision that there was adequate evidence to suggest potential evolution of her esophageal erosion towards the thoracic aorta which could potentially result in a delayed morbid hemorrhage. We therefore elected to take her to the cardiac catheterization laboratory for covered stent implantation over the endangered area of aorta. Aortic Stent placement adjacent to the esophageal area of injury was to be facilitated using 3D visualization Philips © VesselNavigator software, (Andover, Massachusetts) which would allow live procedural guidance utilizing post-processing of the prior CTA. Pediatric cardiothoracic surgery and the perfusion team were immediately available as backup in the event of emergent need for cardiopulmonary bypass and vascular repair.
Following a balanced induction of general anesthesia with intravenous fentanyl, propofol, inhaled sevoflurane, lidocaine topicalization of the vocal cords, and rocuronium bromide for muscle relaxation, the patient was intubated with a cuffed endotracheal tube. The patient remained hemodynamically stable throughout induction and intubation. No pharyngeal mucosal injury was noted by direct laryngoscopy. Two 20-gauge peripheral intravenous catheters were placed and crossmatched blood products were stored in the cardiac catheterization laboratory.
The patient was prepped and draped in a sterile fashion. Access was obtained under ultrasound and fluoroscopic guidance. A working access point was achieved in the right femoral artery and additional catheters were placed in the left common femoral artery, and in an antegrade direction in the left superficial femoral artery. The right internal jugular vein and right femoral veins were similarly accessed. This is standard practice in our catheterization laboratory in high-risk cases to facilitate expeditious percutaneous extracorporeal membrane oxygenation (ECMO) cannulation in the event of cardiovascular collapse. Biplane angiography was performed before placing a guide wire with its tip in the right subclavian artery and upsizing the access sheath for a 12 French 65 cm long sheath (Figure 3A). At this point, the pre-procedural CT imaging that had been post-processed using Philips © VesselNav software (Image Z) was overlayed for live procedural guidance. The landing zone for the stent had been marked on the 3D CT dataset to ensure coverage of the zone of evolving aorta-enteric communication (Figure 3B). A 34 mm long covered stent along with a 36 mm uncovered stent were piggyback mounted on a balloon. The balloon stent complex was inserted to the intended position using fluoroscopic live overlay guidance. The inner and outer balloons were inflated using single inflations after which the balloon was removed over the wire and an additional balloon was inserted and inflated with good stent expansion on fluoroscopy. Pullback pressures documented no gradient across the stent. The catheter was removed, and post intervention angiography was performed demonstrating a satisfactory result (Figure 3C). Local anesthetic was given, and the sheaths were removed. The patient was extubated and transferred to the cardiac intensive care unit for further management. The total procedural time was 89 minutes and total blood loss was twenty milliliters.
Figure 3: Panel A demonstrates a single plane aortic angiogram with a pigtail catheter in the aortic arch. There is no evidence of descending thoracic aortic luminal interruption at the level of the gastro- esophageal junction.
Panel B demonstrates live overlay of the 3D CT imaging with a ring landmark (green) in place at the intended zone of stent deployment. There is a stent partially expanded on the fluoroscopic image in the intended landing zone.
Panel C demonstrates a still frame from a 3D rotational angiogram demonstrating satisfactory expansion of a stent complex within the intended landing zone in the descending thoracic aorta.
Post procedure, the patient was started on a proton pump inhibitor, a nasogastric tube was placed, and she was put on a mechanical soft diet. Repeat imaging four days later included an MRA that showed improved esophageal inflammation and esophagram that showed mild irregularity of the distal esophagus without contrast extravasation. The patient was discharged on postoperative day seven with a nasogastric tube in place until gastroenterology follow-up in the setting of possible stricture development. Follow up at two weeks and three months showed no symptoms of dysphagia and no signs of stricture. No cardiology follow-up was recommended. No thromboprophylaxis was indicated post procedurally due to the large stent caliber. A CT for aortic stent re-evaluation was recommended in two years’ time.
Discussion
Ingestion of button batteries causes a rapid alkaline caustic injury to surrounding tissues and may lead to necrosis and erosion into adjacent structures. Given the anatomical relationship between the esophagus and aorta, the most devasting complication of BB ingestion is vascular perforation leading to massive blood loss. The prompt medical management of small children with ingested and impacted button battery has evolved and recent recommendations include a multidisciplinary team approach for rapid triage and treatment. Immediate home treatment includes mitigation of tissue damage by administration of a pH neutralizing substance, able to coat the battery and limit the electric current injury, most commonly honey is prescribed but jam may also be helpful.8 Honey should be avoided in children <1 years of age and should not be given if greater than 12 hours after ingestion due to increased risk of esophageal perforation. Transportation for triage to the emergency department of a hospital well equipped to perform pediatric endoscopy should not be delayed after a witnessed or suspected BB ingestion. Triage and disposition are based on patient age, battery size, location on imaging, and symptomatology. Batteries in the esophagus require immediate endoscopic removal, within 2 hours after ingestion. If no perforation is visualized, irrigation with a neutralizing substance is warranted. If esophageal injury is present, the patient should be observed and imaged via endoscopy or bronchoscopy for later complications.6 Gastrointestinal, airway, and vascular damage may require surgical intervention. More recently there has been the introduction of more minimally invasive endovascular procedures for management and prevention of vascular injury.
Anesthetic considerations for BB removal include airway management and preparation for the possibility of hemorrhage. Children should be considered a full stomach and are likely to have ingested large amounts of honey or other neutralizing substances and anesthesia should not be delayed for nil per mouth time.9 During laryngoscopy, there should be observation for evidence of mucosal damage, and if so, bronchoscopy may be warranted. Careful airway management during the EGD should be used to avoid accidental extubation while the proceduralist is focusing on BB removal. Based on the presentation and risk assessment, preparation for possible massive hemorrhage may be warranted including adequate vascular access, blood product availability, rapid blood delivery systems, and hemodynamic monitoring. Patients at highest risk should be cared for with a multidisciplinary team in an appropriate location for resuscitation and complex endovascular or surgical interventions. These patients are also likely to require numerous subsequent anesthetics for further imaging and endoscopy.6
Summary
Button battery ingestion is associated with morbidity and mortality and requires prompt multi-disciplinary management. Vascular injury can quickly evolve into devasting hemorrhage warranting novel techniques for prevention and treatment. We demonstrated successful management of a patient with evidence of early aortic injury utilizing an endovascular covered stent. Given the subtlety of early evidence of extraluminal aortic injury, intraprocedural angiography was unlikely to highlight the area of injury. Prior high resolution MRA and CT were able to be utilized with a novel 3-dimensional imaging software to allow live procedural placement at the site of injury, improving efficacy and reducing procedural time and contrast exposure. The anesthesiologist caring for these patients needs to be prepared for multiple anesthetics to facilitate diagnosis, battery removal, peri-procedural imaging, and follow-up. Knowledge of the pathophysiology of button battery ingestion and anesthetic implication is essential for positive patient outcomes.
Acknowledgements: The authors thank the contributions of the Departments of Radiology and Gastroenterology of the University of Colorado, Children’s Hospital Colorado.
Declaration of conflicting of interest: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Single patient case report is not considered human research per Colorado Multiple Institutional Review Board and does not require review per policy. Written parental consent was obtained to publish this case report.
Reference
1. Sharpe SJ, Rochette LM, Smith GA: Pediatric battery-related emergency department visits in the United States, 1990-2009. Pediatrics. 129:1111-1117, 2012.
2. Jatana KR, Litovitz T, Reilly JS, et al.: Pediatric button battery injuries: 2013 task force update. Int. J. Pediatr. Otorhinolaryngol. 77:1392-1399, 2013.
3. Mubarak A, Benninga MA, Broekaert I, et al.: Diagnosis, Management, and Prevention of Button Battery Ingestion in Childhood: A European Society for Paediatric Gastroenterology Hepatology and Nutrition Position Paper. J. Pediatr. Gastroenterol. Nutr. 73:129-136, 2021.
4. Litovitz T, Whitaker N, Clark L: Preventing battery ingestions: an analysis of 8648 cases. Pediatrics. 125:1178-1183, 2010.
5. Ing RJ, Kramer RE, Darst J, et al.: Button battery ingestion in children: a role for angiography? Can. J. Anaesth. 64:321-322, 2017.
6. Hoagland MA, Ing RJ, Jatana KR, et al.: Anesthetic Implications of the New Guidelines for Button Battery Ingestion in Children. Anesth Analg. 130:665-672, 2020.
7. Leinwand K, Brumbaugh DE, Kramer RE: Button Battery Ingestion in Children: A Paradigm for Management of Severe Pediatric Foreign Body Ingestions. Gastrointest. Endosc. Clin. N. Am. 26:99-118, 2016.
8. Chiew AL, Lin CS, Nguyen DT, et al.: Home Therapies to Neutralize Button Battery Injury in a Porcine Esophageal Model. Ann Emerg Med. 83:351-359, 2024.
9. Vaucel JA, Gil-Jardine C, Paradis C, et al.: Pre-hospital triage of children at risk of oesophageal button battery impaction: the button battery impaction score. Clin. Toxicol. (Phila.). 61:1047-1054, 2023.
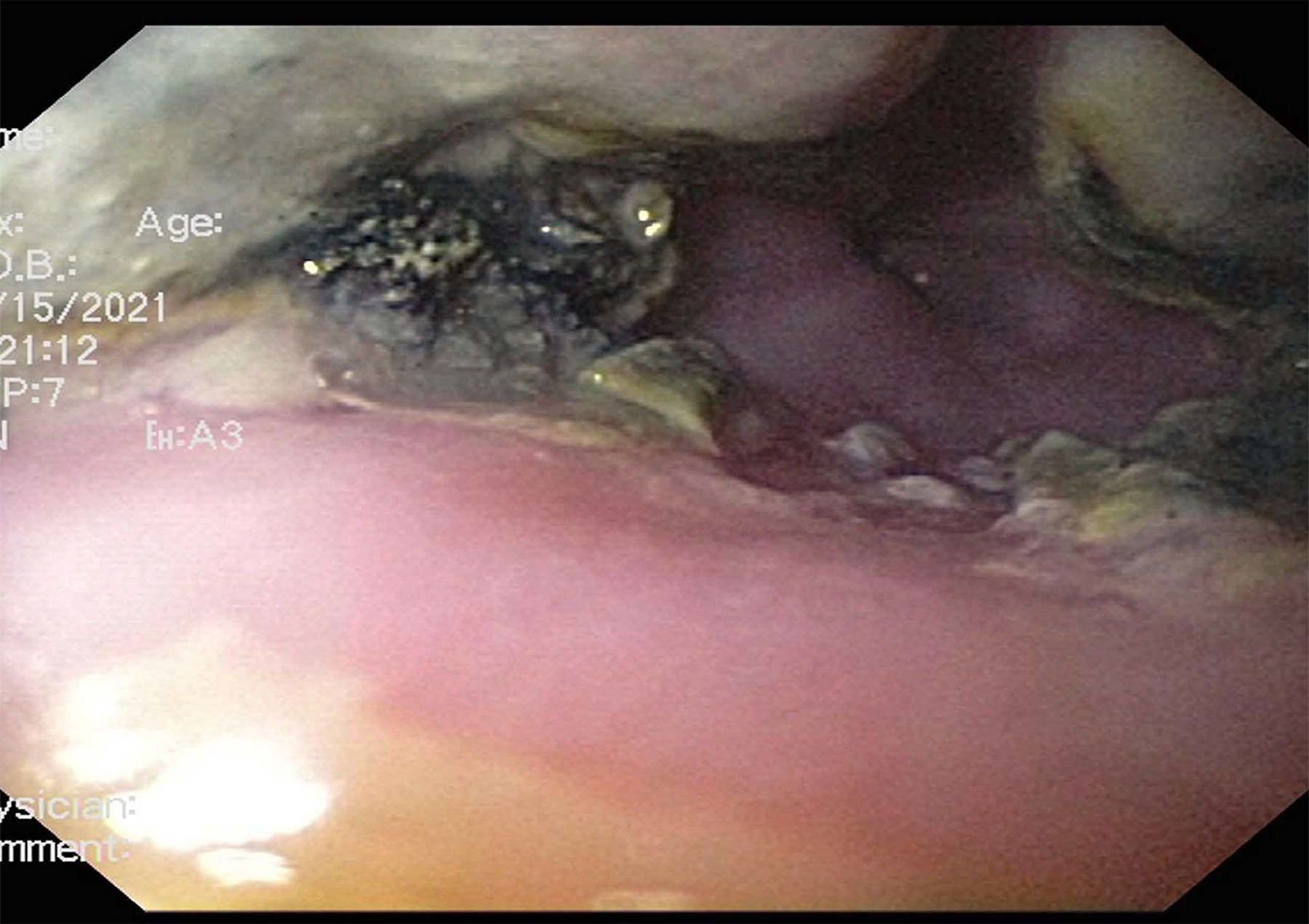
Figure 1
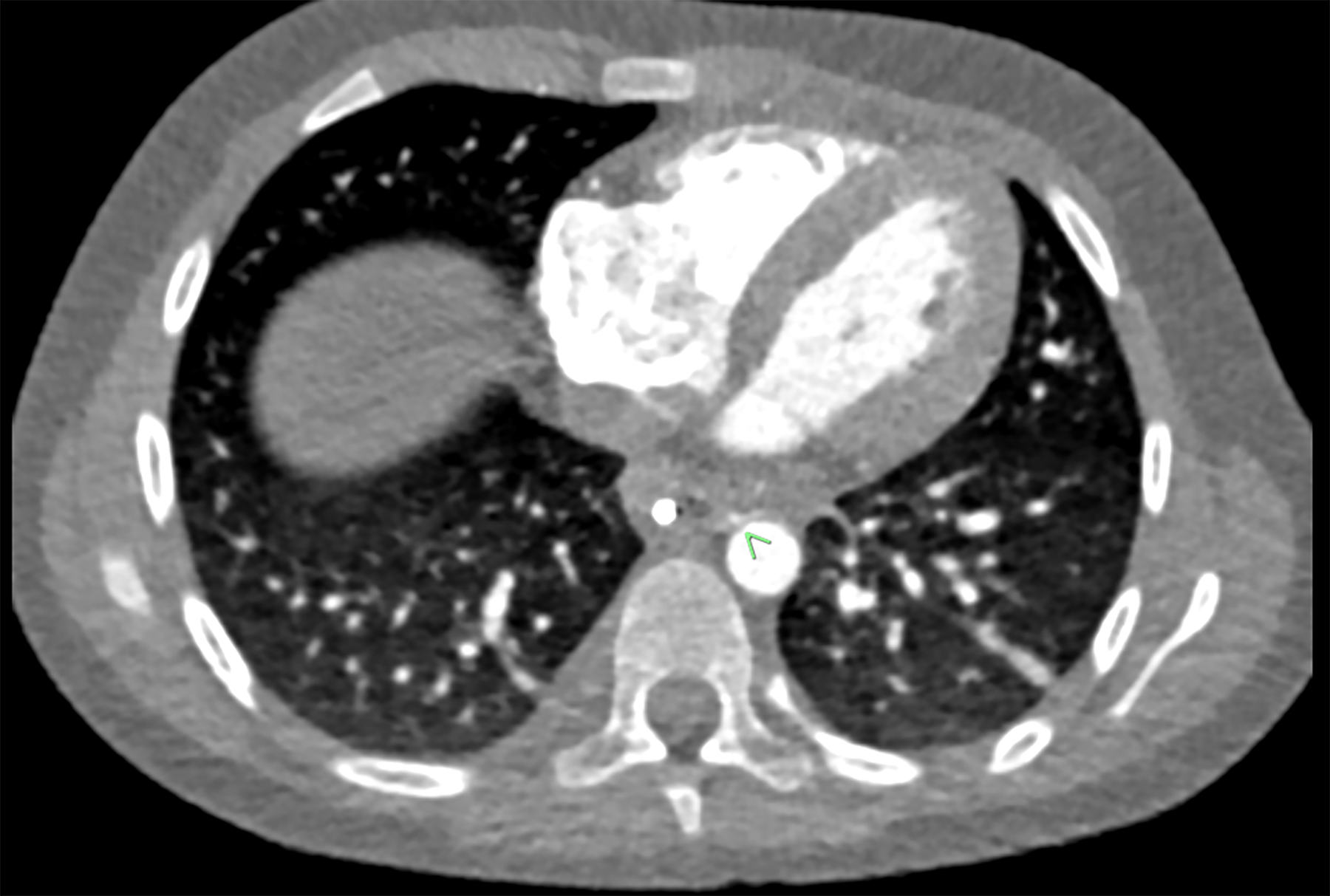
Figure 2
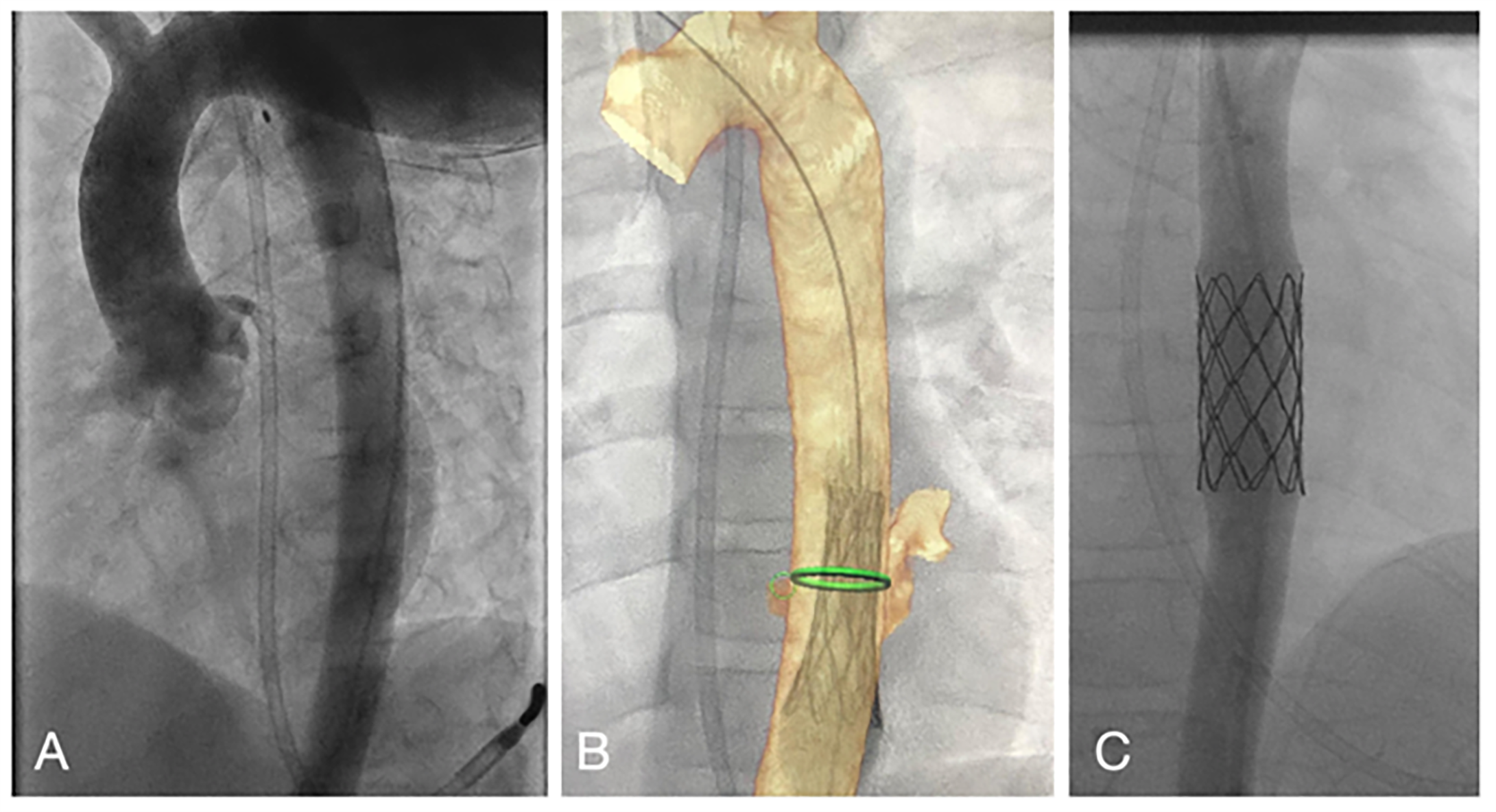
Figure 3
