Case Report on Necrotizing Fasciitis following Cesarean Section
Case Report on Necrotizing Fasciitis following Cesarean Section
Shamaila Mahboob*
*Correspondence to: Shamaila Mahboob, MRCOG UK.
Copyright
© 2024 Shamaila Mahboob. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 03 November 2024
Published: 07 November 2024
DOI: https://doi.org/10.5281/zenodo.14051135
Abstract
A 28-year-old female, six days post-cesarean section, presented with severe wound pain, fever, and night sweats. Clinical examination revealed necrotic tissue and signs of sepsis. Prompt surgical debridement and antibiotic therapy led to significant improvement and eventual discharge.
Case Report on Necrotizing Fasciitis following Cesarean Section
Introduction
Necrotizing fasciitis is a rare but life-threatening infection characterized by rapidly progressing necrosis of subcutaneous tissue and fascia. This condition is often referred to as a "flesh-eating disease" due to the aggressive nature of tissue destruction and can result in significant morbidity or mortality if not diagnosed and treated promptly. Early diagnosis and aggressive treatment, including surgical intervention and broad-spectrum antibiotics, are crucial for patient survival. This case report describes a postpartum patient who developed necrotizing fasciitis following a cesarean section and highlights the importance of timely intervention in managing this severe condition.
Case Presentation
Patient Description:
-Age: 28 years old
- Gravida/Para: P2 (2 pregnancies, 2 live births)- Postpartum: 6 days post-cesarean section performed at 37 weeks + 6 days due to cord presentation
- Estimated Blood Loss during surgery: 1.2 L- Baby: Well and healthy
- Allergies: Penicillin
Medical History:
-Psychiatric History:
The patient has a history of Obsessive-Compulsive Disorder (OCD) and previously used sertraline.
- Cardiology Review:
Reviewed by cardiology for tachycardia during pregnancy; investigations including bedside echocardiogram, CT pulmonary angiography (CTPA), and 24-hour Holter monitor were reassuring.
Current Medications:
- Regular Medications: None reported.
- Postoperative Medications: Lactulose, Dihydrocodeine 30 mg as needed, Dalteparin 5000 units once daily for 10 days postoperatively.
Presenting Complaints:
Pain: Patient reported severe, sharp wound pain rated 8/10 since the cesarean section, constant in nature, with no radiation.
Other Symptoms: The patient also experienced fever and night sweats. There were no complaints of shortness of breath, cough, chest pain, palpitations, calf pain, edema, or urinary/bowel symptoms.
Examination Findings:
- General Appearance: The patient appeared unwell and in distress.
- Airway: Patent; chest clear upon auscultation.- Breathing: Clear bilaterally with good air entry.
- Circulation: Notable findings included a bounding peripheral pulse, tachycardia (HR 142 bpm), warm peripheries, and capillary refill time <3 seconds. The patient was sweating and clammy.- Disability: Glasgow Coma Scale (GCS) scored 15, indicating full consciousness and alertness.
- Exposure: Examination of the abdomen revealed erythema and skin blistering across the lower abdomen, with crepitation noted. The wound site was clean; however, a 4x4 cm area in the right lower quadrant exhibited necrotic black tissue surrounded by green discoloration, with significant tenderness and foul odor.
Vital Signs:
- Heart Rate: 142 bpm
- Temperature: 38.2°C- Blood Pressure: 114/59 mmHg
-Oxygen Saturation: 97%- Modified Early Warning Score (MEWS): 2 (red).
Laboratory Results:
- Hemoglobin (Hb): 99 g/L- Lactate: 7 mmol/L (indicative of possible tissue hypoperfusion)
- C-reactive Protein (CRP): 348 mg/L (indicating inflammation)- Estimated Glomerular Filtration Rate (eGFR): >60 mL/min (normal renal function)
- Alkaline Phosphatase (ALP): 153 IU/L (mild elevation)- Platelets: 628 x 10^9/L (thrombocytosis)
- White Blood Cell Count (WBC): 16 x 10^9/L (leukocytosis)- Neutrophils: 14 x 10^9/L (indicating bacterial infection)
-Coagulation Profile: Normal.
Initial Management and Investigations
Based on the clinical presentation and examination findings, the impression of necrotizing fasciitis with associated sepsis was made. The Sepsis 6 protocol was initiated:
- **Blood
Cultures:** Obtained to identify any potential causative organisms.- Lactate Measurement: Elevated lactate level noted, suggesting sepsis.
- CRP Measurement: Conducted to evaluate inflammatory response.- Intravenous Access: Two large-bore cannulae were established in the antecubital fossa.
-Intravenous Fluids: 0.9% NaCl 500 mL stat, followed by 1 liter over 1 hour.- NPO Status: Patient was made nil by mouth in preparation for potential surgical intervention.
- Microbiology Consultation: Engaged to guide antibiotic choice due to penicillin allergy.- Wound Swab: Obtained for culture.
- Antibiotic Regimen Initiated: Ceftriaxone, metronidazole, and clindamycin were administered intravenously, accounting for the patient's allergy history.
Radiological findings
Imaging Modality: CT Pelvis and Abdomen
1. Subcutaneous and Fascial Gas: Presence of gas within the subcutaneous tissues and fascial planes of the pelvic region, particularly around the lower abdomen, perineum, and pelvic floor. Air tracking along fascial planes is a hallmark of necrotizing fasciitis, strongly suggesting infection in postpartum cases.
2. Soft Tissue Edema and Thickening: Extensive thickening and increased density of subcutaneous tissues and fascial layers in the pelvic and perineal regions, with widespread edema beyond typical boundaries. This indicates rapid spread of infection, especially relevant in the postpartum period.
3. Loss of Fascial Plane Definition: Loss of normal fat plane definition between muscles and fascial layers in the pelvic region. This "fascial blurring" is characteristic of aggressive soft tissue infection.
4. Fluid Collections or Abscesses: Irregular fluid collections may be present, potentially indicating abscess formation along the pelvic fascial planes or in perineal tissues. These collections often have heterogeneous densities and may contain gas bubbles or necrotic tissue.
Surgical Intervention
Following initial resuscitation and stabilization, the patient consented to undergo an exploratory laparotomy with the potential for necrotic tissue removal.
Day 1 Surgery: Primary debridement was performed, where all necrotic tissue was excised. The procedure was extensive due to the significant extent of tissue involvement.- Day 2 Surgery: Wound closure was performed after adequate hemostasis and ensuring clean margins.
Postoperative Care: The patient was admitted to the Intensive Treatment Unit (ITU) for close monitoring and one-to-one nursing care. Patient-controlled analgesia was established for effective pain management.
Microbiology Findings- Organisms Identified:
Culture results revealed Enterococcus faecalis along with mixed anaerobes.
- Antibiotic Adjustment: Based on culture results, the antibiotic regimen was adjusted to include vancomycin along with the continuation of metronidazole.
Follow-up and Progress
-Day 3:
Patient's CRP showed improvement, decreasing to 203 mg/L from 348 mg/L. Platelet counts increased to 726 x 10^9/L. The wound appeared clean and dry, indicating effective debridement and control of the infection. Vancomycin levels were checked.
- Day 4:
Laboratory results indicated further improvement: Hemoglobin dropped to 84 g/L (possibly due to blood loss during surgery), WBC count decreased to 10 x 10^9/L, and platelets rose to 755 x 10^9/L. CRP levels continued to decrease to 123 mg/L, and lactate normalized to 0.7 mmol/L. Routine laboratory tests for urea, electrolytes, and liver function returned normal. Vancomycin levels were recorded at 6.8 (subtherapeutic), prompting an increase in the dosage from 1500 mg BD to 2000 mg BD. Additionally, the patient was started on oral iron supplementation.
-Day 6:
The patient's condition had significantly improved. She appeared well, was able to eat and drink, and her pain was well-controlled. She had normal urinary and bowel movements, with no fever present. Lochia was within normal limits, and the MEWS score was recorded at 0, indicating stable clinical status.
Discussion
Necrotizing fasciitis, although rare, poses a serious threat, particularly in the postpartum setting where surgical interventions like cesarean sections can create a pathway for infection. This case illustrates the importance of recognizing early signs of infection, such as increased pain, fever, and changes in wound appearance. The rapid initiation of the Sepsis 6 protocol and aggressive surgical intervention were pivotal in the management of this patient.
Timely diagnosis and treatment are essential for a favorable outcome in cases of necrotizing fasciitis. The collaborative approach among surgical, medical, and microbiology teams ensures a comprehensive treatment strategy. This case underscores the need for awareness of the risk factors and clinical presentations of necrotizing fasciitis, particularly following surgical procedures, and the necessity for vigilance in monitoring postpartum patients for potential complications.
Conclusion
This case report emphasizes the critical importance of early identification and intervention in cases of necrotizing fasciitis, particularly in a postpartum context. It illustrates how a coordinated, multidisciplinary approach can effectively manage complex surgical infections, resulting in positive patient outcomes.
Regular follow-up and monitoring for complications are essential in the postoperative period, especially in cases with significant risk factors such as surgical history and underlying medical conditions.
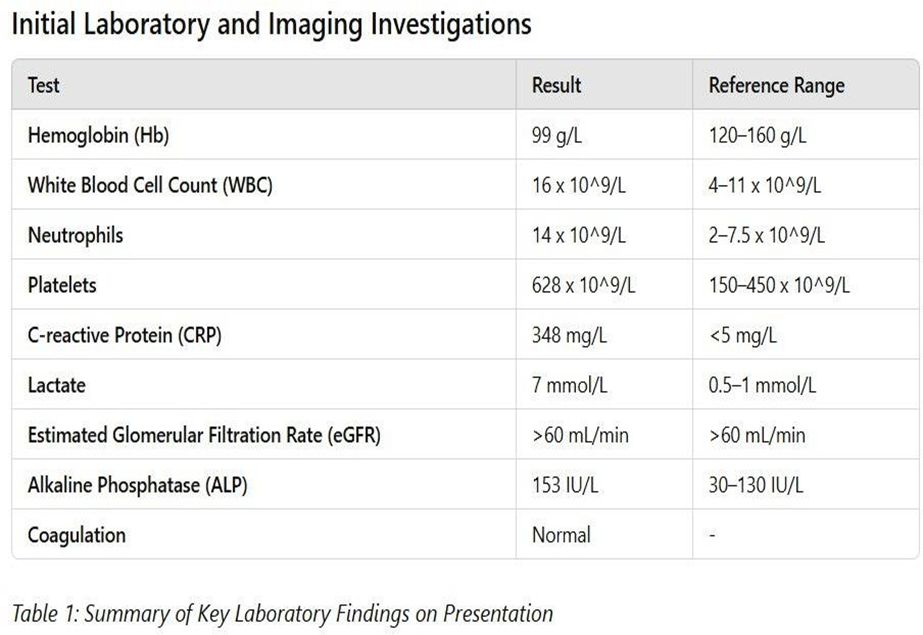
Figure 1
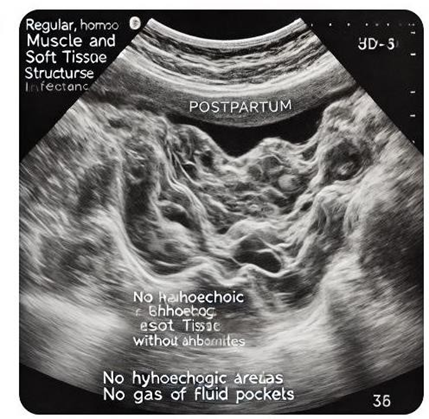
Figure 2
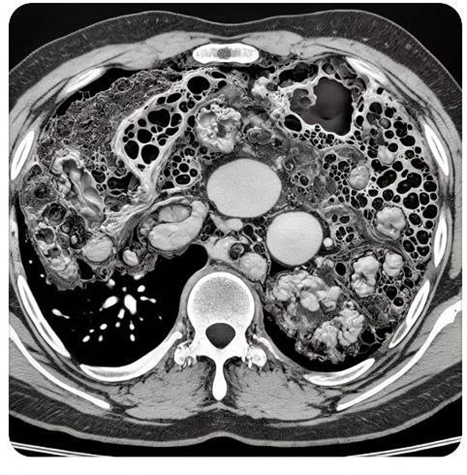
Figure 3
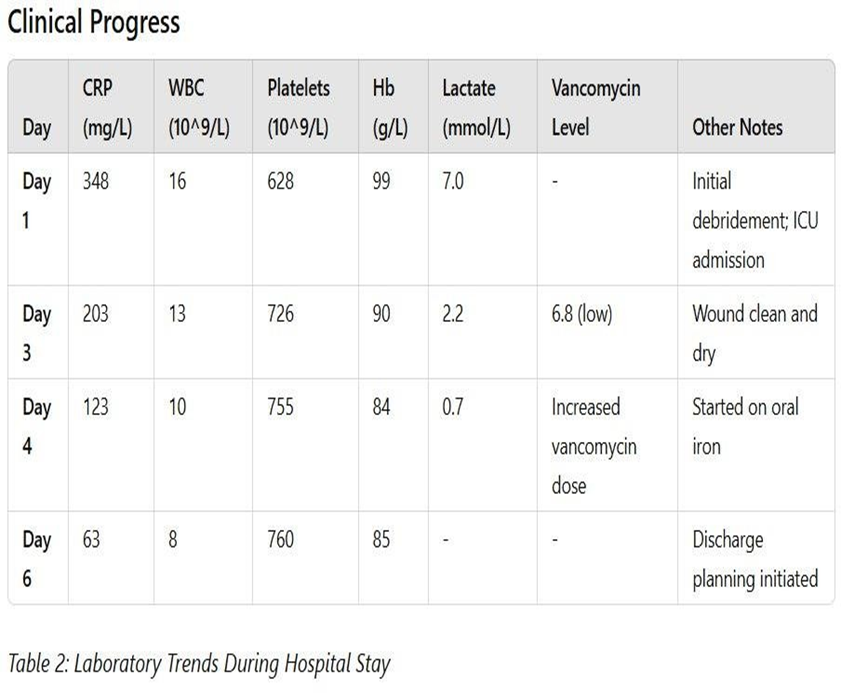
Figure 4
