Central Corneal Thickness and Associated Factors among Adult Patients Attended Menelik II Referal Hospital, Ethiopia 2024
Central Corneal Thickness and Associated Factors among Adult Patients Attended Menelik II Referal Hospital, Ethiopia 2024
Dr. Daniel Gebreegziabher Baraki*1, Dr. Abeba Teklegiorgis Weldegiorgis2, Dr. Abiye Mulugeta Alemu, Dr. Tesfaye Tadesse Dumecha4
1. Glaucoma Fellow, Department Of Ophthalmology, Addis Ababa University, Ethiopia.
2, 3. MD, Ass. Professor of Ophthalmology, Glaucoma Surgeon, CHS), Addis Ababa University, Ethiopia.
4. Assistant Professor of Ophthalmology Glaucoma Surgeon, CHS), Addis Ababa University, Ethiopia.
*Correspondence to: Dr. Daniel Gebreegziabher Baraki, Glaucoma Fellow, Department Of Ophthalmology, Addis Ababa University, Ethiopia.
Copyright
© 2024 Dr. Daniel Gebreegziabher Baraki. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 29 September 2024
Published: 11 November 2024
Abstract:
Background: Central corneal thickness (CCT) refers to the thickness of the central part of the cornea. This ocular parameter significantly influences corneal rigidity, which in turn affects the precision of intraocular pressure (IOP) measurements. Thinner corneas are often associated to more advanced stages of glaucomatous optic neuropathy and CCT varies among different ethnic groups. Therefore, considering both CCT and ethnic factors is crucial for effective glaucoma management
Objective: To determine the central corneal thickness and assess the associated factors among adults in Menellik II Referral Hospital Addis Abeba, Ethiopia, from April to May 2024.
Methodology: A Hospital based cross sectional study was conducted among 334 adult outpatients who attended Menelik II Referral Hospital from April to May 2024. Data was collected by PI using structured questionnaire then exported to SPSS version 26 for analysis. The descriptive statistics summarized and presented using summary statistics such as frequency tables and graphs. Variables having p-values of less than 0.05 is considered as statistically significant. The final result of the analysis was presented by tables and graphs.
Result: A total of 334 adults participated in the study with a response rate of 93.3%. The median ( ± IQR) age of study respondents was 60( ±12) years and 53.3% were males. Mean CCT for overall patient population was 519± 33.19(Range 421-630) microns in the right eye and 520 ±34.31 (420-665) in the left eye. There was no statistically significant difference in CCT between the right and left eyes (P>0.05) and no statistically significant mean CCT difference between males (520 ±34) and females (517±32) p value 0.56. The mean CCT of the participants decreases significantly as age goes up as 40-50 (528±33),51-60 (522±31),61-70(516±32),>71 (504±31) p value < 0.05. A weak negative correlation between CCT and age was statistically significant (r = -0.235, p < 0.05). Additionally, a weak positive correlation between CCT and IOP was found (r = 0.138, p < 0.05).
Conclusion: The average central corneal thickness (CCT) in the patient population was 519 ± 33.19 microns for the right eye, with a range of 421 to 630 microns, and 520 ± 34.31 microns for the left eye, ranging from 420 to 665 microns. There was no statistically significant difference in mean CCT between males and females, nor between the right and left eyes .Notably, CCT tends to decrease with age, leading to thinner corneas in older individuals. This thinning of the cornea with advancing age is accompanied by a positive correlation between CCT and intraocular pressure (IOP), and a negative correlation between CCT and age, indicating that as individual’s age increases, their corneal thickness decreases potentially influencing IOP measurements , our decision on diagnosis and managing glaucoma patients.
Key words CCT, Glaucoma, IOP, Ethiopia.
Central Corneal Thickness and Associated Factors among Adult Patients Attended Menelik II Referal Hospital, Ethiopia 2024
CCT………………………….CENTRAL CORNEAL THICKNESS
GAT………………………… GOLDMAN APPLANATION TONOMETRY
IOP………..………………….INTRAOCULAR PRESSURE
VCD………………………….VERTICAL CUP DISC RATIO
INTRODUCTION AND PURPOSE
BACKGROUND
Central corneal thickness (CCT) measures the thickness of the central portion of the cornea. This parameter significantly influences corneal rigidity, which in turn affects the precision of intraocular pressure (IOP) measurements obtained through Goldman applanation tonometry (GAT) (1).
Research has shown that individuals with glaucoma, as well as those suspected of having the disease, generally have thinner corneas compared to healthy individuals. Moreover, CCT tends to decrease with age (2) An increase in CCT is associated with a rise in IOP, while corneal thickness has been found to be inversely related to age, with IOP showing a positive correlation with age.(3)
Thinner corneas in glaucomatous eyes are often associated to more advanced stages of glaucomatous optic neuropathy. Therefore, considering both CCT and ethnic factors is crucial for effective glaucoma management (4)
STATEMENT OF THE PROBLEM
Central corneal thickness (CCT) not only influences the precision of intraocular pressure (IOP) measurements(1) but also reveals that individuals with thin corneas, including glaucoma suspects and glaucoma patients are at a higher risk of disease progression(2). Conversely, a thicker cornea can lead to elevated IOP readings, which can impact decision-making in managing glaucoma patients(3).
Additionally, research indicates that CCT tends to decrease with age, and since the prevalence of glaucoma increases as we grow older, assessing CCT is crucial in managing both glaucoma suspects and glaucoma patients(5).
By providing specific data on central corneal thickness of Ethiopian patients, it will contribute to more accurate diagnostics, better-informed treatment decisions, and ultimately improved patient care.
RATIONALE OF THE STUDY
Central corneal thickness (CCT) is a crucial ocular parameter, playing a significant role in the assessment of different eye diseases including glaucoma. Central corneal thickness can affect intraocular pressure (IOP) measurements which consequently influences our decision on diagnosis and management of glaucoma.
CCT varies among different ethnic groups in the world. African populations often have thinner CCT measurements compared to European or Asian populations. Understanding these differences is important for developing management protocols targeting to the specific needs of Ethiopian patients .It is also known that the prevalence of glaucoma is higher and it tends to be more aggressive in African populations and thin CCT is a well known risk factor for glaucoma; therefore, determining the average CCT of Ethiopian patients may has significant impact on early detection and treatment of Ethiopian patients. This study aims in narrowing the gap in ophthalmic researches by focusing on Ethiopian population for improved patient care.
Study Area
Menelik II Referral Hospital is located in Addis Ababa, the capital city of Ethiopia .It is one of the oldest hospitals in the country ,established and named after Emperor Menelik II in the late 19th century.it is tertiary eye care hospital . Moreover, Menelik II Referral Hospital is a peculiar institution in Ethiopia eye health care system, contributing tremendously in training residents and fellowship programs , research and eye care . The study has conducted among adult outpatient attending at this hospital.
Study design and period
Hospital based cross sectional study was conducted to determine the CCT and associated factors among adult outpatients visiting Minilik-II Referral Hospital Addis Abeba, Ethiopia from April to May 2024
Source and study population
Source of Population : All patients visiting outpatient department of Menelik II Referral Hospital during the study period
Study population: All adult patients (age >40) who visit ophthalmology department of Menelik II Referral Hospital during the study period were included
Study unit: Consecutive patients age 40 and above visiting ophthalmology department of Menelik II Referral Hospital ophthalmology during the study period
Eligibility criteria
Inclusion criteria: All adult patients age above 40 were included
Exclusion criteria: Patients with corneal opacity or corneal ulcer
Sample size and sampling technique
All consecutive patients who came during the study period were included
Dependent variable: Central corneal thickness
Independent variable
Ocular parameters
Age, Sex, IOP, disc evaluation
Data processing and analysis
Data collection tools and procedures
After getting written informed consent a structured questionnaire was used and administered to collect demographic, lifestyle, and systemic health information. All participants were new patients taken from triage clinic. All ophthalmic examination was done by first investigator. Intraocular pressure measurement was done with Zeiss Visuplan 500( Air puff tonometer), and visual acuity was assessed using illuminated snellens chart. Ophthalmic examinations, including slit-lamp biomicroscopy and hand held ultrasound pachymetry(Keeler PachPen ) was performed after applying topical tetracaine to measure central corneal thickness. Posterior segment was assessed with Volk lens 90 D after pupillary dilation with 1% tropicamide
Data quality assurance
At the end of each day, all of the collected data was reviewed and checked for completeness and entered into a prepared data analysis software using SPSS Version 26 by the first investigator
Data processing and analysis
- Data was entered, coded and analyzed using SPSS Version 26. Variables were compared using the appropriate statistical tests. P Values <0.05 was considered statistically significant.
- Data was analyzed for frequency, range, mean and standard deviation of the different sociodemographic characteristics.
- Any association of ocular parametrs with CCT was analyzed
RESULT
1. Socio-demographic Characteristics of Study Participants
This study consisted of 334 adults who are age of 40 and above, which represents 93.3% response rate and 178 of them were males and 156 were females. The mean and median age of participants was 60±11.89 and 60 respectively. The majority of the study participants were Orthodox (66.8%) followed by Muslim (21.3%), Protestant (9.9%) and Other (2.1%).
Table 1: Scio-demographic characteristics of the study participants in Menelik II Referral Hospital, Addis Ababa, Ethiopia 2024
|
Variable |
Frequency |
Percentage (%) |
|
Age(years) 40-50 51-60 61-70 >70 |
87 96 89 62 |
26.0 28.7 26.6 18.6 |
|
Sex Male Female |
178 156 |
53.3 46.7 |
|
Residence Rural Urban |
99 235 |
29.6 70.4 |
|
Religion Orthodox Muslim Protestant Other |
223 71 33 7 |
66.8 21.25 9.9 2.1 |
|
Educational level Unable to read and write Only able to read and write Primary education Secondary education College/University |
106 73 51 46 58 |
31.7 21.9 15.3 13.8 17.4 |
2. Ocular Characteristics of Study Participants
Ultrasound pachymetry with topical ansthesia was done for all patients and the result show as follows: Mean CCT for overall patient population was 519± 33.19(Range 421-630) microns in the right eye 520 ±34.31 (420-665) in the left eye.
Figure 1: Histogram of OD Central Corneal Thickness
Figure 2: Histogram of OS Central Corneal Thickness
The study found no statistically significant difference in central corneal thickness (CCT) between the eyes (P > 0.05), leading to the selection of the right eye for further analysis. Additionally, there was no significant difference in mean CCT between males (520 ± 34 microns) and females (517 ± 32 microns), with a p-value of 0.56. However, a one-way ANOVA with post hoc analysis revealed that mean CCT significantly decreases with age, with values of 528 ± 33 microns for ages 40-50, 522 ± 31 microns for ages 51-60, 516 ± 32 microns for ages 61-70, and 504 ± 31 microns for those over 71 years old, with a p-value of < 0.05.
The bar chart displays the mean central corneal thickness (CCT) across different age groups.
Figure 3: Mean CCT difference between Age groups
Table 2: One way ANOVA with post hoc analysis of CCT of the right eye of the study participants in Menelik II Referral Hospital, Addis Ababa, Ethiopia 2024
|
One way ANOVA with post hoc analysis showing Multiple Comparisons in the right eye |
||||||
|
(I) age cat |
(J) age cat |
Mean Difference (I-J) |
Std. Error |
Sig. |
95% Confidence Interval |
|
|
Lower Bound |
Upper Bound |
|||||
|
40-50 |
51-60 |
5.76365 |
4.78491 |
.624 |
-6.5918 |
18.1191 |
|
61-70 |
12.30040 |
4.87355 |
.058 |
-.2839 |
24.8847 |
|
|
>=71 |
23.57749* |
5.37256 |
.000 |
9.7046 |
37.4504 |
|
|
51-60 |
40-50 |
-5.76365 |
4.78491 |
.624 |
-18.1191 |
6.5918 |
|
61-70 |
6.53675 |
4.75663 |
.516 |
-5.7457 |
18.8192 |
|
|
>=71 |
17.81384* |
5.26673 |
.004 |
4.2143 |
31.4134 |
|
|
61-70 |
40-50 |
-12.30040 |
4.87355 |
.058 |
-24.8847 |
.2839 |
|
51-60 |
-6.53675 |
4.75663 |
.516 |
-18.8192 |
5.7457 |
|
|
>=71 |
11.27709 |
5.34738 |
.152 |
-2.5308 |
25.0849 |
|
|
>=71 |
40-50 |
-23.57749* |
5.37256 |
.000 |
-37.4504 |
-9.7046 |
|
51-60 |
-17.81384* |
5.26673 |
.004 |
-31.4134 |
-4.2143 |
|
|
61-70 |
-11.27709 |
5.34738 |
.152 |
-25.0849 |
2.5308 |
|
There was statistically significant mean CCT difference between those>71 and 40 -50(p value 0.000) and 50-60 (p value 0.04) on the right eye.
Fig 4: Line graph representing OD Mean of CCT with respect to age
Table 3: One way ANOVA with post hoc analysis of CCT of the left eye of the study participants in Menelik II Referral Hospital, Addis Ababa, Ethiopia 2024
|
One way ANOVA with post hoc analysis showing Multiple Comparisons in the left eye |
||||||
|
(I) age cat |
(J) age cat |
Mean Difference (I-J) |
Std. Error |
Sig. |
95% Confidence Interval |
|
|
Lower Bound |
Upper Bound |
|||||
|
40-50 |
51-60 |
4.38901 |
4.92766 |
.810 |
-8.3350 |
17.1131 |
|
61-70 |
15.09699* |
5.01894 |
.015 |
2.1372 |
28.0567 |
|
|
>=71 |
24.07416* |
5.53284 |
.000 |
9.7874 |
38.3609 |
|
|
51-60 |
40-50 |
-4.38901 |
4.92766 |
.810 |
-17.1131 |
8.3350 |
|
61-70 |
10.70798 |
4.89853 |
.129 |
-1.9408 |
23.3568 |
|
|
>=71 |
19.68515* |
5.42385 |
.002 |
5.6799 |
33.6904 |
|
|
61-70 |
40-50 |
-15.09699* |
5.01894 |
.015 |
-28.0567 |
-2.1372 |
|
51-60 |
-10.70798 |
4.89853 |
.129 |
-23.3568 |
1.9408 |
|
|
>=71 |
8.97717 |
5.50691 |
.363 |
-5.2426 |
23.1969 |
|
|
>=71 |
40-50 |
-24.07416* |
5.53284 |
.000 |
-38.3609 |
-9.7874 |
|
51-60 |
-19.68515* |
5.42385 |
.002 |
-33.6904 |
-5.6799 |
|
|
61-70 |
-8.97717 |
5.50691 |
.363 |
-23.1969 |
5.2426 |
|
|
||||||
Similarly there was statistically significant mean CCT difference between those>71 and 40 -50(p value 0.00) and 50-60 (p value 0.02 ) on the left eye.
Fig 5: Line graph representing OS Mean CCT with respect to age
The factors influencing central corneal thickness (CCT) are outlined below (table 4):
• CCT shows a negative correlation with age and a positive correlation with intraocular pressure (IOP), with p-values less than 0.005.
• The vertical cup-to-disc ratio (VCD) shows a positive correlation with both age and IOP, with p-values less than 0.005.
There was no significant statistical difference in the mean VCD between the right eye (0.45 ± 0.25) and the left eye (0.45 ± 0.24). A weak negative correlation between CCT and age was statistically significant (r = -0.235, p < 0.05). Additionally, a weak positive correlation between CCT and IOP was found (r = 0.138, p < 0.05). No significant correlation was observed between CCT and VCD (r = -0.046, p = 0.440). However, VCD showed a positive correlation with age (r = 0.131, p = 0.027) and IOP (r = 0.422, p < 0.000).
Table 4: Linear Regression Showing the factors associated with Central Corneal Thickness
|
Correlations |
|||||
|
|
OD CCT |
Age in completed year |
IOP OD |
OD-disc evaluation |
|
|
OD CCT
|
Pearson Correlation |
1 |
-.235** |
.138* |
-.046 |
|
Sig. (2-tailed) |
|
.000 |
.011 |
.440 |
|
|
N |
334 |
334 |
334 |
286 |
|
|
age in completed year |
Pearson Correlation |
-.235** |
1 |
-.010 |
.131* |
|
Sig. (2-tailed) |
.000 |
|
.853 |
.027 |
|
|
N |
334 |
334 |
334 |
286 |
|
|
IOP OD |
Pearson Correlation |
.138* |
-.010 |
1 |
.422** |
|
Sig. (2-tailed) |
.011 |
.853 |
|
.000 |
|
|
N |
334 |
334 |
334 |
286 |
|
|
OD disc evaluation |
Pearson Correlation |
-.046 |
.131* |
.422** |
1 |
|
Sig. (2-tailed) |
.440 |
.027 |
.000 |
|
|
|
N |
286 |
286 |
286 |
286 |
|
|
|||||
|
|||||
An independent t-test was conducted to compare the average central corneal thickness (CCT) between glaucoma and non-glaucoma patients. The results indicated that the mean CCT in glaucoma patients (516 ± 34) was thinner compared to that of non-glaucoma patients (519 ± 32), though this difference was not statistically significant.
Table 5: Central Corneal Thickness Mean among glaucomatous and non-glaucomatous patients
|
|
Glaucoma |
N |
Mean |
Std. Deviation |
Std. Error Mean |
P-value |
|
OD CCT |
No |
261 |
519.7816 |
32.73275 |
2.02611 |
0.451 |
|
Yes |
73 |
516.4658 |
34.91899 |
4.08696 |
DISCUSSION
Central corneal thickness (CCT) has recently been identified as a crucial element in diagnosing glaucoma.(1) Besides influencing intraocular pressure (IOP) measurements, CCT has been recognized as an independent risk factor for the glaucoma(12). CCT values vary across different racial groups with individuals of African descent having the thinnest CCT (7, 13)
In our study mean CCT of patients which is found to be 519± 33.19 μm is comparable to African Americans (right eye 531.0±36.3 µm; left eye, 530.0±34.6 µm) (7) and Egyptian population( 530.06 ± 38.03 μm)(8) Additionally non glaucoma patients from Menelik hospital in Ethiopia had shown similar findings (516.2±23.4μm)(11) However mean CCT of our patients is thinner than Caucasian (including those with and without glaucoma) (right eye, 558.0 ± 34.5 µm; left eye, 557.6 ± 34.5 µm) patients (7) which further strengthen that African American have thin central corneal thickness.
In contrast mean CCT of study participants was thicker than the normal tension glaucoma patients in Menelik II hospital ,Ethiopia (488.0±32.4 μm) (11)and Indian glaucoma patients (503.91 ± 11.31 μm) (14) which emphasizes normal tension glaucoma patients have thin CCT and are at risk of progression.
Some of the previous studies show that CCT correlates significantly with sex while others do not. We found no statistically significant difference between males ( 520 ±34 μm) and females(517±32 μm) p value 0.56 similar to studies done in Lithuanian patients (5) , Nepalese population(15) and Korean population(16)
We observed A statistically significant weak negative correlation between CCT and age (r=-0.235 P <0.05) and CCT significantly decreases as age goes up 40-50 ( 528 ±33 μm),51-60 (522±31 μm),61-70(516±32 μm),>71 (504±31 μm) p value < 0.05 similar to studies done in Egypt(8) Luthanian(5) , Jimma, south west Ethiopia (10) and Nigerian population(17)Reduced central corneal thickness on older people might be due to a reduction in keratocyte density and corneal dehydration over years.
Our study also showed statistically significant weak positive correlation between CCT and IOP (r =0.138 p <0.05) similar to researches done in Egypt (8) ,Jimma ,south west Ethiopia (10) and Pakistani population,2010(18) indicating that thick cornea results in high IOP readings.
We observed also mean CCT among glaucoma patients was thinner (261 ±32 μm) than non-glaucomatous patients (516± 34 μm) but not statistically significant similar to researches done in Jimma ,south west Ethiopia ,2015 (9) , Menelik hospital ,2014(11) ,Korean patients ,2002 (19),and Nepalese patients,2014(20)referring to thin cornea might be an independent risk factor for glaucoma.
CONCLUSION
The average central corneal thickness (CCT) in the patient population was 519 ± 33.19 microns for the right eye, with a range of 421 to 630 microns, and 520 ± 34.31 microns for the left eye, ranging from 420 to 665 microns. There was no statistically significant difference in mean CCT between males and females, nor between the right and left eyes .Notably, CCT tends to decrease with age, leading to thinner corneas in older individuals. This thinning of the cornea with advancing age is accompanied by a positive correlation between CCT and intraocular pressure (IOP), and a negative correlation between CCT and age, indicating that as individual’s age increases, their corneal thickness decreases potentially influencing IOP measurements , our decision on diagnosis and managing glaucoma patients.
RECOMMENDATION
Longitudinal studies to track changes in central corneal thickness over years and to possibly evaluate the impact of environmental factors on cornea is recommended.. Additionally, it is advisable to routinely practice pachymetry for all patients attending glaucoma clinics.
ACKNOWLEDGMNT
We would like to thank the Department of Ophthalmology and all the staff who were supportive throughout the study. Our appreciation goes to the study participants for their cooperation and willingness which made this study possible.
References
1. Brandt JD, Beiser JA, Kass MA, Gordon MO, Ocular Hypertension Treatment Study (OHTS) Group. Central corneal thickness in the ocular hypertension treatment study (OHTS). Ophthalmology. 2001;108(10):1779–88. https://www.sciencedirect.com/science/article/pii/S0161642001007606
2. Mercieca K, Odogu V, Fiebai B, Arowolo O, Chukwuka F. Comparing central corneal thickness in a sub-Saharan cohort to African Americans and Afro-Caribbeans. Cornea. 2007;26(5):557–60. https://journals.lww.com/corneajrnl/fulltext/2007/06000/Comparing_Central_Corneal_Thickness_in_a.00010.aspx
3. Eballe AO, Koki G, Ellong A, Owono D, Epée E, Bella LA, et al. Central corneal thickness and intraocular pressure in the Cameroonian nonglaucomatous population. Clinical ophthalmology. 2010;717–24. https://www.tandfonline.com/doi/abs/10.2147/opth.s10575
4. Muhsen S, Alkhalaileh F, Hamdan M, AlRyalat SA. Central corneal thickness in a Jordanian population and its association with different types of Glaucoma: cross-sectional study. BMC ophthalmology. 2018;18:1–7. https://link.springer.com/article/10.1186/s12886-018-0944-6
5. Galgauskas S, Juodkaite G, Tutkuvien? J. Age-related changes in central corneal thickness in normal eyes among the adult Lithuanian population. Clinical interventions in aging. 2014;1145–51. https://www.tandfonline.com/doi/abs/10.2147/CIA.S61790
6. Tayyab A, Masrur A, Afzal F, Iqbal F, Naseem K. Central corneal thickness and its relationship to intra-ocular and epidmiological determinants. J Coll Physicians Surg Pak. 2016;26(6):494–7. https://www.researchgate.net/profile/Ali-Tayyab/publication/305003800_Central_Corneal_Thickness_and_its_Relationship_to_Intra-Ocular_and_Epidmiological_Determinants/links/57862e2208aec5c2e4e2dc83/Central-Corneal-Thickness-and-its-Relationship-to-Intra-Ocular-and-Epidmiological-Determinants.pdf
7. La Rosa FA, Gross RL, Orengo-Nania S. Central corneal thickness of Caucasians and African Americans in glaucomatous and nonglaucomatous populations. Archives of ophthalmology. 2001;119(1):23–7. https://jamanetwork.com/journals/jamaophthalmology/article-abstract/264897
8. Mostafa EM. Central corneal thickness in southern Egypt. International ophthalmology. 2014;34:809–15. https://link.springer.com/article/10.1007/s10792-013-9885-5
9. Gelaw Y. The impact of central corneal thickness on intraocular pressure among Ethiopian glaucoma patients: a cross-sectional study. BMC ophthalmology. 2012;12:1–6. https://link.springer.com/article/10.1186/1471-2415-12-58
10. Tolesa K, Gessesse GW. Central corneal thickness in newly diagnosed glaucoma patients in South West Ethiopia: a cross-sectional study. BMC ophthalmology. 2016;16:1–6. https://link.springer.com/article/10.1186/s12886-016-0334-x
11. Mulugeta A, Gizachew Z. Central corneal thickness among glaucoma patients attending Menelik II Hospital, Addis Ababa, Ethiopia. Ethiopian Journal of Health Development. 2018;32(1). https://www.ajol.info/index.php/ejhd/article/view/171231
12. Congdon NG, Broman AT, Bandeen-Roche K, Grover D, Quigley HA. Central corneal thickness and corneal hysteresis associated with glaucoma damage. American journal of ophthalmology. 2006;141(5):868–75. https://www.sciencedirect.com/science/article/pii/S0002939405012924
13. Herndon LW, Weizer JS, Stinnett SS. Central corneal thickness as a risk factor for advanced glaucoma damage. Archives of ophthalmology. 2004;122(1):17–21. https://jamanetwork.com/journals/jamaophthalmology/article-abstract/416038
14. Shetgar AC, Mulimani MB. The central corneal thickness in normal tension glaucoma, primary open angle glaucoma and ocular hypertension. Journal of clinical and diagnostic research: JCDR. 2013;7(6):1063. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3708199/
15. Godar S, Kaini K, Khattri J. Factors affecting the central corneal thickness in Nepalese population. Nepal journal of medical sciences. 2012;1(1):7–10. https://nepjol.info/index.php/NJMS/article/view/5788
16. Lee DH, Kim DH, Park SH. Age and sex related changes in corneal thickness and anterior corneal curvature in Korean young population with Orbscan II topography system. Journal of the Optical Society of Korea. 2011;15(1):68–73. https://opg.optica.org/abstract.cfm?uri=josk-15-1-68
17. Iyamu E, Osuobeni E. Age, gender, corneal diameter, corneal curvature and central corneal thickness in Nigerians with normal intra ocular pressure. Journal of optometry. 2012;5(2):87–97. https://www.sciencedirect.com/science/article/pii/S1888429612000210
18. Ul Hassan M, ur Rehman A, Abbas M, Fawad U, Bhatti N, Daud A. Relationship between central corneal thickness and intraocular pressure in selected Pakistani population. Pakistan Journal of Ophthalmology. 2010;26(2). http://www.pjo.org.pk/index.php/pjo/article/view/583
19. Lee ES, Kim CY, Ha SJ, Seong GJ, Hong YJ. Central corneal thickness of Korean patients with glaucoma. Ophthalmology. 2007;114(5):927–30. https://www.sciencedirect.com/science/article/pii/S0161642006014837
20. Adhikari P, Chettry P, Thapa M. Central Corneal Thickness in Nepalese Glaucoma Patients and Glaucoma Suspects. Journal of Clinical Research and Ophthalmology. 2014;2(1):003–6. https://www.clinsurggroup.us/Clinical-Research-Ophthalmology/JCRO-2-107.php.
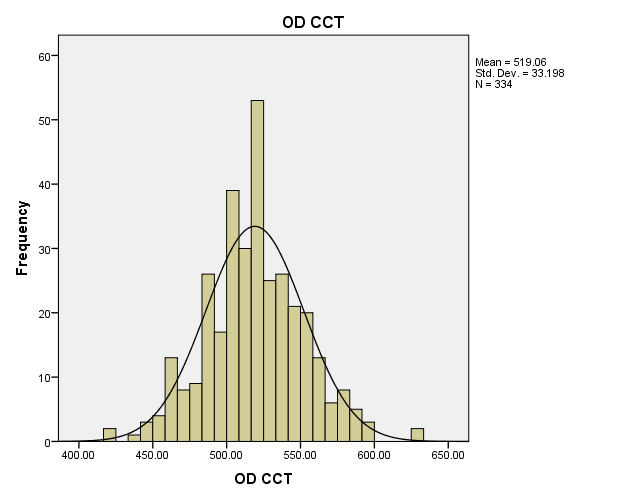
Figure 1
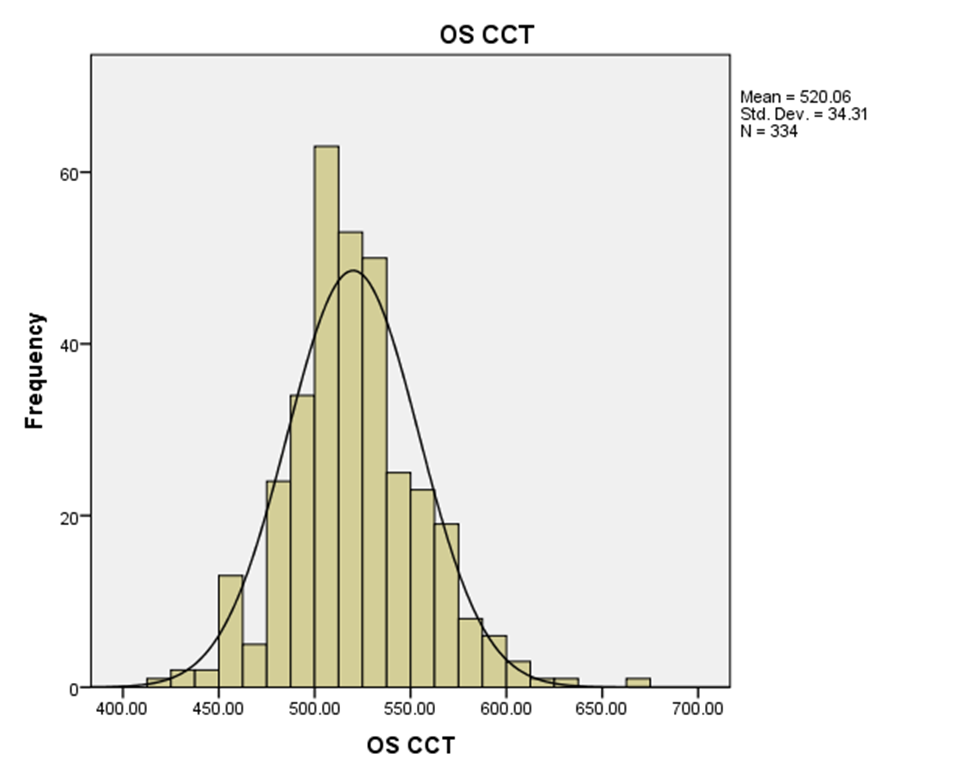
Figure 2
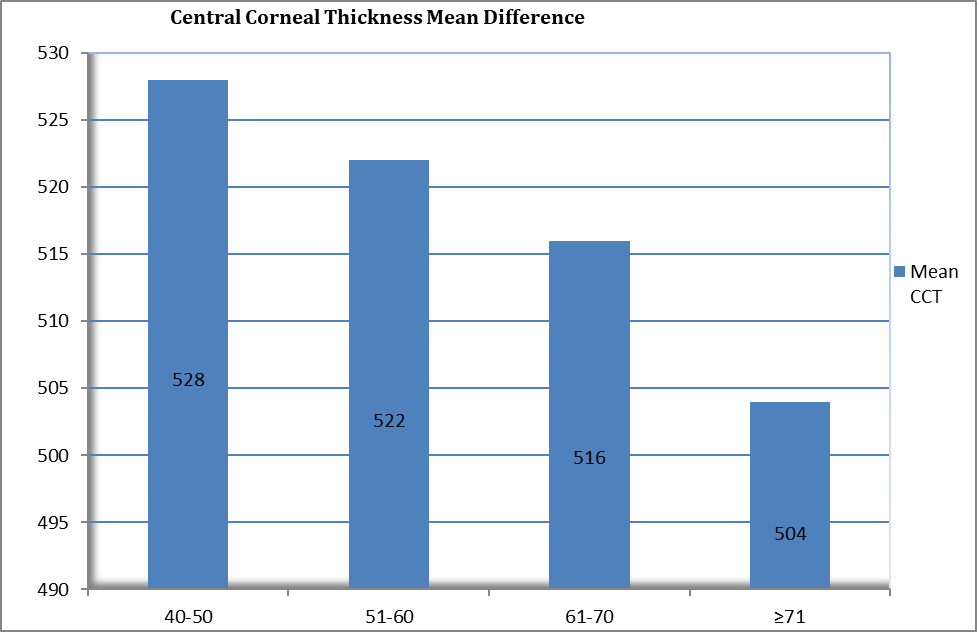
Figure 3
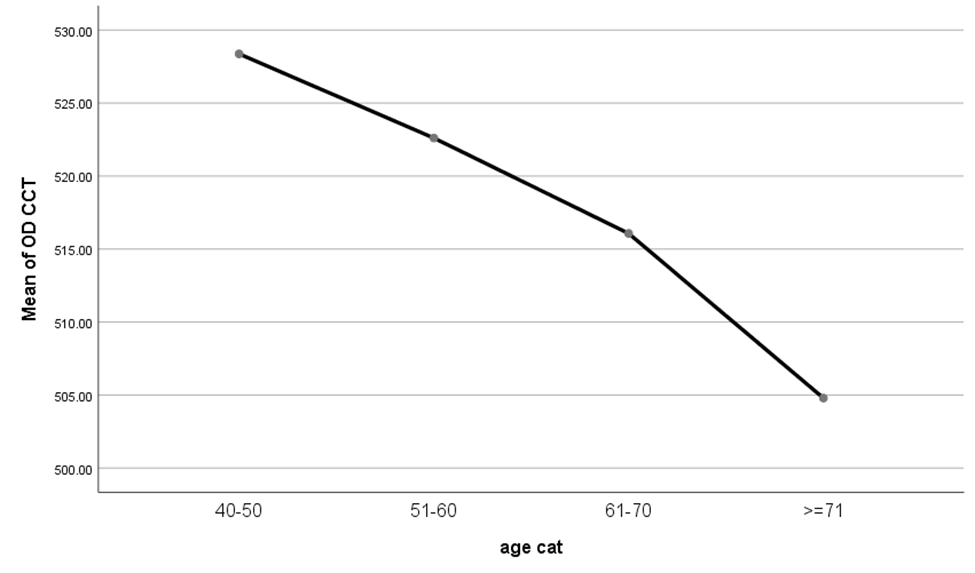
Figure 4
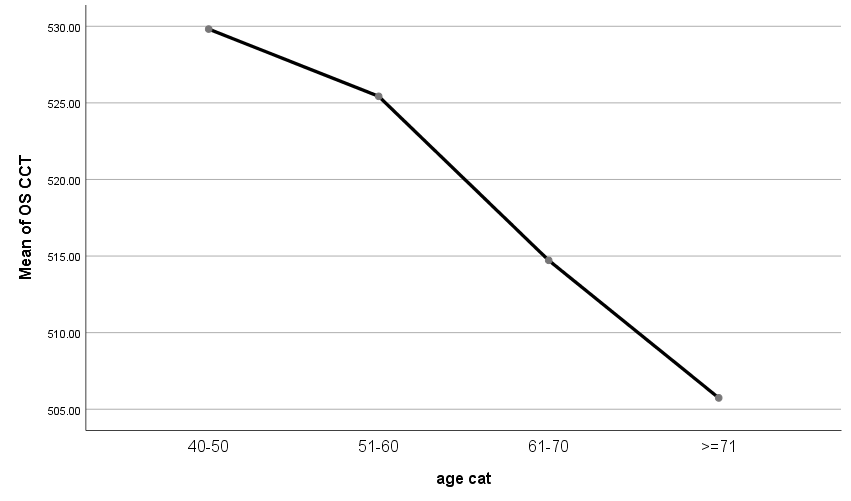
Figure 5
