Biochemical Study in a Porcine Tibial Model to Compare the Fixation Strengths Provided by different Intraosseous Tendon Lengths during Anterior Cruciate Ligament Reconstruction
Biochemical Study in a Porcine Tibial Model to Compare the Fixation Strengths Provided by different Intraosseous Tendon Lengths during Anterior Cruciate Ligament Reconstruction
Haytham Al Husari1*, Dr Kassem El Houcheimi 2
1. Dr Kassem El Houcheimi, FACS, MBA, Orthopedic surgeon, Clemenceau Medical Center Dubai.
*Correspondence to: H Haytham Al Husari, MD, DFMSA, Lower Limb Arthroplasty and Sports Fellowship Orthopaedic Trauma Fellowship, University Diploma in Arthroscopy and Microsurgery.
Copyright
© 2024 Haytham Al Husari. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 01 Nov 2024
Published: 15 Nov 2024
DOI: https://doi.org/10.5281/zenodo.14168484
Abstract:
This study aimed to determine the tibial fixation strength provided by different intraosseous soft tissue graft lengths within the tibial tunnel. Porcine tibial bones and digital flexor tendons were tested, and bone mineral densities of proximal tibial medial condyles were measured. Two-strand tendon bundles of 8 mm diameter were used. Two groups were tested: one group used a 2 cm intraosseous graft length, while the other used a 4 cm graft length. Tibial fixation was performed using a suture tied around a screw post with a washer and an additional inserted 7 × 20 mm bioabsorbable screw. After applying preconditioning loading of 10 cycles, 1,000 cycles between 70–220 N were applied at a frequency of 1 Hz. Graft slippage and total graft movement were recorded, and ultimate tensile strength was measured by pull-out testing at an Instron crosshead speed of 1,000 mm/min. No significant intergroup difference was found for total graft movement after cyclic loading. The results show that a 2 cm intraosseous graft length in the tibial tunnel is safe and has sufficient strength (> 450 N) for adequate rehabilitation after anterior cruciate ligament reconstruction.
Keywords; Fixation strength, Tendon length, Anterior cruciate ligament reconstruction, Biomechanical study.
Biochemical Study in a Porcine Tibial Model to Compare the Fixation Strengths Provided by different Intraosseous Tendon Lengths during Anterior Cruciate Ligament Reconstruction
Introduction
The anterior cruciate ligament (ACL) is a crucial part of the body, carrying only small loads during normal daily functions. Soft tissue grafts, such as hamstring tendon grafts, require a long intraaosseous length within the bone tunnel for adequate fixation strength due to delayed healing. However, if the strengths of shorter tendon lengths within the bone tunnel are similar to those currently used, ACL reconstruction could be performed using a single tendon instead of a doubletendon, reducing donor site morbidity and allowing earlier rehabilitation.
The ACL carries only small loads during normal daily functions, with a fixation strength of 450 N being sufficient for rehabilitation after ACL reconstruction. If a minimum of 28 cm of semitendinosus tendon is harvested, a 7 cm four-strand semitendinosus graft can be made for ACL reconstruction, a 2 cm graft for the femoral tunnel, a 3 cm graft for the intra-articular portion, and a 2 cm graft for the tibial tunnel.
Some studies have considered optimal graft length in the femoral bone tunnel, finding that reducing tendon graft length from 25 to 15 mm did not have any adverse histological or biomechanical effects in a small animal model. The hypothesis is that fixation with a 2 cm tendon length in a bone tunnel would achieve the fixation strength of 450 N required for adequate rehabilitation after ACL reconstruction.
Methods
This study was conducted using 20 frozen porcine hind limbs from 90 kg pigs aged 8-9 months. After removing all muscles, ligaments, and knee joint capsules, the tibiae were prepared for testing. Hind limb flexor digitorum tendons were harvested and stored at -20°C until required for testing. The specimens were thawed overnight at 4°C before being allocated to one of two study groups (group 1 [n = 10], the 2 cm intraosseous graft length group; and group 2 [n = 10], the 4 cm graft length group).
Bone mineral densities (BMD) were measured by dual-emission X-ray absorptiometry at the anteromedial tibial metaphysis, and in 10 healthy young men. Graft tendons of length 8 and 6 cm were prepared, and graft ends were sewn using Ticron #2 non-absorbable sutures with an interlocking stitch. In group 1, grafts had an intraosseous length of 2 cm and an extraosseous length of 4 cm, while in group 2, grafts had an intraosseous length of 4 cm and an extraosseous length of graft of 4 cm.
Grafts were fixed using four-strand sutures tied around a screw post with a washer and a single 7 × 20 mm bioabsorbable screw inserted between the tibial bone tunnels and grafts. An Electroplus E3000 unit was used for tensile strength testing, with samples subjected to preconditioning, 1,000 cycles of 70–220 N at 1 Hz, and pull-out testing at a crosshead speed of 1,000 mm/min after completing the cyclic tensile loading test.
Failure modes were evaluated, and the means, ranges, and standard deviations of graft slippage, total graft movement, and ultimate tensile strength were calculated. The Mann-Whitney U-test was used to compare graft slippage, total graft movement, and ultimate tensile strength, while the Kruskal-Wallis test was used to compare BMD differences. The required study sample size was determined using biomechanical data from earlier studies. Results were analyzed using IBM SPSS ver. 19, and p-value < 0.05 was considered significant.
Fig 1: Graft Preparation
Fig 2: Tendon graft was fixed at the tibial tunnel by a post-tie suture and a bioabsorbable screw
Results
The study analyzed the bone mineral density (BMD) at the anteromedial tibial condyle in two experimental groups. The mean BMD was 1.119 g/cm2 in group 1, 1.025 g/cm2 in group 2, and 0.974 g/cm2 in the human control group. All grafts were pulled out from the bone tunnel, except one in group 2 that failed due to graft rupture. After cyclic loading, mean graft slippage was 1.2 mm in group 1 and 1.2 mm in group 2, with the upper 95% confidence limit of graft slippage being less than 2.0 mm in both groups. Total graft movement was 3.3 mm in group 1 and 2.7 mm in group 2, with the upper 95% confidence limit of total graft movement being 4.1 mm in group 1 and 3.1 mm in group 2. No significant intergroup difference was observed for graft slippage or total graft movement. However, the fixation strength of the 2 cm graft (> 450 N) was suitable for early rehabilitation after ACL reconstruction.
Discussion
This study aimed to determine the strength of a 2 cm long graft within a bone tunnel for early rehabilitation after ACL reconstruction. The ultimate tensile loads for a four-strand suture tied around a screw post with a washer and secured with additional a bioabsorbable interference screw were 649.9 N and 938 N, respectively, which were greater than previous studies reported in these studies.
The findings indicate that the ultimate tensile loads of 2 cm grafts meet early rehabilitation requirements, despite being lower than those provided by a 4 cm graft. Early rehabilitation after ACL reconstruction is associated with better outcomes, but previous fixation strength studies have usually focused on fixation methods and graft materials or on the biomechanical properties of interference screw fixed soft-tissue grafts. Insufficient scientific evidence is available to make recommendations regarding graft length in the femoral tunnel during ACL reconstruction using a soft tissue graft, but it is commonly believed that graft healing is improved by having more graft tissue within the bone tunnel, as this provides a tighter fit.
Some biomechanical and clinical studies have been conducted on ACL reconstruction using a single semitendinosus tendon, that is, without gracilis harvesting. Most of these studies concluded that ACL reconstruction using a single four-strand semitendinosus tendon short graft produces good clinical results, does not compromise joint stability, and reduces donor site morbidity. They concluded that this technique provide a good option for ACL reconstruction.
Some limitations of the current study include using a porcine model, which raises questions about its clinical applicability, and the specimen type used when performing graft fixation experiments using animal models. Direct comparisons between human specimens are difficult due to factors such as donor age and bone density differences. The study also involved time-zero biomechanical testing under immediate postoperative conditions, which led to no histological comparison.
In conclusion, a 2 cm graft is suitable for an early rehabilitation program after ACL reconstruction as it can cope with loads in excess of 450 N.
References
1. Zantop T, Ferretti M, Bell KM, Brucker PU, Gilbertson L, Fu FH. Effect of tunnel-graft length on the biomechanics of anterior cruciate ligament-reconstructed knees: intra-articular study in a goat model. Am J Sports Med. 2008;36(11):2158- 66.
2. Yamazaki S, Yasuda K, Tomita F, Minami A, Tohyama H.The effect of intraosseous graft length on tendon-bone healing in anterior cruciate ligament reconstruction using flexor tendon. Knee Surg Sports Traumatol Arthrosc. 2006;14(11):1086-93.
3. Qi L, Chang C, Jian L, Xin T, Gang Z. Effect of varying the length of soft-tissue grafts in the tibial tunnel in a canine anterior cruciate ligament reconstruction model. Arthroscopy. 2011;27(6):825-33.
4. Kyung HS, Kim TG, Oh CW, Yoon SH. Anterior cruciate ligament reconstruction with a four-strand single semitendinosus tendon autograft. J Korean Arthrosc Soc. 2009;13(2):138-42.
5. Herrera A, Martinez F, Iglesias D, Cegonino J, Ibarz E, Gracia L. Fixation strength of biocomposite wedge interference screw in ACL reconstruction: effect of screw length and tunnel/screw ratio: a controlled laboratory study. BMC Musculoskelet Disord. 2010;11:139.
6. Nagarkatti DG, McKeon BP, Donahue BS, Fulkerson JP. Mechanical evaluation of a soft tissue interference screw in free tendon anterior cruciate ligament graft fixation. Am J Sports Med. 2001;29(1):67-71.
7. Coleridge SD, Amis AA. A comparison of five tibial fixation systems in hamstring-graft anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2004;12(5):391-7.
8. Halewood C, Hirschmann MT, Newman S, Hleihil J, Chaimski G, Amis AA. The fixation strength of a novel ACL soft-tissue graft fixation device compared with conventional interference screws: a biomechanical study in vitro. Knee Surg Sports Traumatol Arthrosc. 2011;19(4):559-67.
9. Fleming BC, Magarian EM, Harrison SL, Paller DJ, Murray MM. Collagen scaffold supplementation does not improve the functional properties of the repaired anterior cruciate ligament. J Orthop Res. 2010;28(6):703-9.
10. Murray MM, Magarian EM, Harrison SL, Mastrangelo AN, Zurakowski D, Fleming BC. The effect of skeletal maturity on functional healing of the anterior cruciate ligament. J Bone Joint Surg Am. 2010;92(11):2039-49.
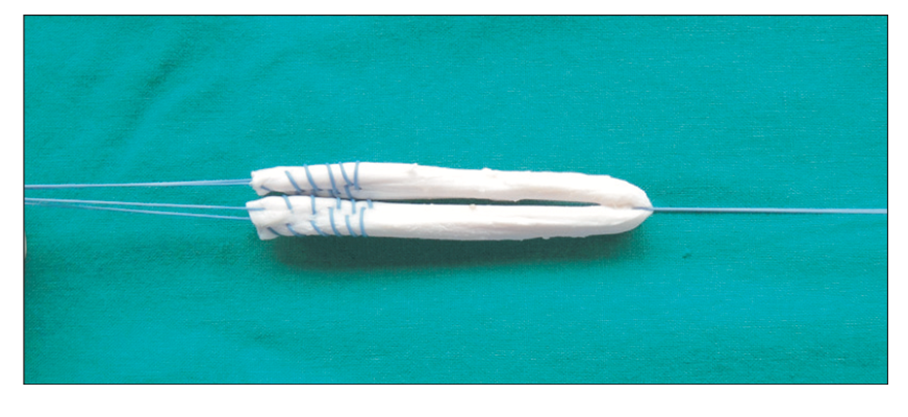
Figure 1
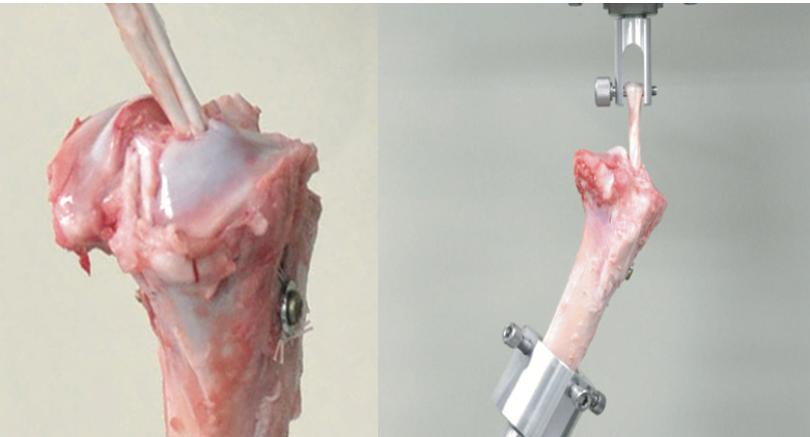
Figure 2

Figure 3
