EUS Guided Gastroenterostomy for Gastric Outlet Obstruction: A Valid Therapeutic Option
EUS Guided Gastroenterostomy for Gastric Outlet Obstruction: A Valid Therapeutic Option
Khaled AlMojil1, Salah Termos *
1. Department of Surgery AlAmiri Hospital, MOH, Kuwait.
*Correspondence to: Salah Termos MD FACS, Consultant General & HPB Surgeon, AlAmiri Hospital, Kuwait.
Copyright
© 2024 Salah Termos. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 05 November 2024
Published: 26 November 2024
DOI: https://doi.org/10.5281/zenodo.14219896
Abstract
Gastric outlet obstruction (GOO) can occur to different etiologies that cause distal stomach narrowing and eventually occlusion. Management of these cases is usually by endoscopic stenting or surgical alimentary diversion. However these options may not always feasible due patient conditions or many other reasons.
In our manuscript we describe two cases of GOO due to advanced cancer disease. Both patients had complete occlusion and were not medical fit for any surgical intervention. They underwent endoscopic ultrasound guided gastroenterostomy with uneventful peri-procedure period.
EUS guided gastroenterostomy can be considered as potential alternative to traditional surgery or endoscopic approach mainly in terminally ill patients with gastric outlet obstruction.
Keywords: Gastric Outlet Obstruction (GOO); Endoscopic Ultrasound (EUS); Gastrojejunostomy (GJ); Gastroenterostomy (GE)
EUS Guided Gastroenterostomy for Gastric Outlet Obstruction: A Valid Therapeutic Option
Introduction
Endoscopic ultrasound guided gastrojejunostomy or gastroenterostomy (EUS-GJ, EUS-GE) is novel endoscopic procedure that has recently emerged as a new treatment for some benign and malignant etiologies. For the most part, EUS-GJ has been employed in the treatment of benign and malignant gastric outlet obstruction (GOO) [1]. Additionally, EUS-GJ has been used in the treatment of afferent loop syndrome [2].
EUS-GJ involves obtaining access to the jejunum endoscopically and sonographically from the stomach, using a biflanged lumen apposing metal stent (LAMS). This is achieved through a newly formed fistulous tract. Thus creating a gastrojejunal bypass fully endoscopically.
In our study, we describes two cases of end stage cancer disease who underwent minimal invasive EUS guided gastrojejunostomy for gastric outlet obstruction (GOO).
Case 1: 69-year-old male with metastatic gastric carcinoma, who refused chemotherapy. He eventually developed food intolerance due to GOO and was initially placed with a transpyloric uncovered self-expandable metal stent (SEMS) for improvement of his clinical condition However, symptoms recurred after one month, and tumoral ingrowth of the SEMS was confirmed. After a multidisciplinary team meeting, it was decided to propose EUS-GJ.
The procedure involved instilling 900 cc of saline solution with methylene blue to promote jejunal dilation using a catheter. Under ultrasonographic guidance, the bowel loop was accessed using a "wireless endoscopic simplified technique" (WEST), placing a lumen-apposing stent (LAMS) through the greater curvature of the stomach. The enteral communication was created and dilated with a through-the-scope balloon up to 15 mm .[3-4]. The patient restarted oral food intake within 12 hours and remained food-tolerant until he passed away, 3 months after the procedure
Case 2: 78-year-old female patient with pancreatic ductal adenocarcinoma of the uncinate process, locally advanced with mesenteric vessels involvement. She presented with obstructive jaundice and underwent an endoscopic retrograde cholangiopancreatography with successful placement of metal biliary stent. Patient refused any neoadjuvant chemotherapy and six weeks later, she developed GOO symptoms and stricturing tumoral infiltration of the distal second portion of the duodenum [5-6]. After multidisciplinary discussion, she was proposed for EUS-GJ. Procedure was performed with a 20 mm × 10-mm LAMS through the posterior gastric wall using WEST [7]. Patient has a successful 6 months period of food tolerance after which she passed away from the progression of her disease.
Fig. 1.: Jejunal loop
Fig. 2: Gastroenterostomy endoscopic appearance after LAMS lumen balloon dilation.
Fig. 3: Fluoroscopic confirmation of LAMS correct placement (arrows) in patient 1 (a), 2 (b), and 3 (c).
Discussion
Gastric outlet obstruction can be due to different etiologies. Malignant causes usually are due to advanced gastric, duodenal and pancreatic cancers however, benign causes include peptic ulcer disease, chronic pancreatitis, caustic injury and NSAID injury. Since the identification of Helicobacter Pylori and the increase of use of proton pump inhibitors, benign entities become the less common cause of GOO than malignant [8].
GOO has been conventionally treated using two methods, which are surgery (laparoscopic, robotic or open approach) and endoscopic enteral stenting or balloon dilation. Surgical method is associated with a high complications rate mainly in high risk patient. Endoscopic placement of an enteral self-expanding metal stent (SEMS) is associated with fewer complications, shorter hospitalization however there is a concern about long term patency and recurrence rates necessitating reintervention. Endoscopic balloon dilation is another endoscopic modality that is effective in treating gastric outlet obstruction.
Recently EUS-GJ has emerged as a new treatment modality for patients with GOO. Several case reports and more recently few retrospective studies demonstrated promising from the use of EUS-GJ in treatment benign and malignant GOO. EUS-GE offers a less invasive approach than surgery without the associated morbidity. EUS-GE offers as solution to the long-term patency and recurrence issue encountered with enteral stenting and endoscopic balloon dilation [9].
The procedure can be performed using cautery enhanced or non-cautery enhanced LAMS. Dilation of the of the tract is preformed using a balloon catheter or a cystatome over a guidewire which is followed by LAMS deployment. Regardless of the technique used the afferent limb is distended using a mixed solution of contrast saline and methylene blue [2].
Since the introduction of EUS-GJ adequate positioning and deployment of the stent has been high ranging between 86 to 100% irrespective of the technique used with a clinical success reaching 80 to 100 % [10]. Commonly reported adverse events have included stent misdeployment, peritonitis, bleeding and leakage [7,10].
In our manuscript, we report two cases of advanced gastric and pancreatic malignancies presenting with GOO. Both patients refused chemotherapy or any surgical option. After MDT meeting they underwent successful endoscopic ultrasound guided gastroenterostomy with acceptable clinical outcomes.
Conclusion
Gastric outlet obstruction is a clinically significant manifestation that requires abrupt medical attention. EUS guided gastroenterostomy is a safe and less invasive procedure that in expert hands can be considered as potential alternative to traditional surgery or endoscopic approach only in certain group of patients. More studies are needed to establish an algorithm and clear indication for EUS-GE for GOO.
References
1- Khashab MA, Bukhari M, Baron TH, et al. International multicenter comparative trial of endoscopic ultrasonography-guided gastroenterostomy versus surgical gastrojejunostomy for the treatment of malignant gastric outlet obstruction. Endosc Int Open 2017;5:E275-81. 10.1055/s-0043-101695 [DOI] [PMC free article] [PubMed] [Google Scholar]
2- Brewer Gutierrez OI, Irani SS, Ngamruengphong S, et al. Endoscopic ultrasound-guided entero-enterostomy for the treatment of afferent loop syndrome: a multicenter experience. Endoscopy 2018;50:891-5. 10.1055/s-0044-102254 [DOI] [PubMed] [Google Scholar]
3- Takeno A, Takiguchi S, Fujita J, et al. Clinical outcome and indications for palliative gastrojejunostomy in unresectable advanced gastric cancer: Multi-institutional retrospective analysis. Ann Surg Oncol. 2013; 20: 3527-3533.
4- Tendler DA. Malignant gastric outlet obstruction: bridging another divide . Am J Gastroenterol. 2002; Tyberg A, Perez-Miranda M, Sanchez-Ocaña R, et al. Endoscopic ultrasound-guided gastrojejunostomy with a lumen-apposing metal stent: A multicenter, international experience. Endosc Int Open. 2016; 4(03): E276-E281.
5- Khashab MA, Baron, TH, Binmoeller KF, Itoi T. EUS-guided gastroenterostomy: a new promising technique in evolution. Gastrointest Endosc. 2015 May; 81 (5):1234 – 6. Google Scholar Crossref PubMed
6- Carbajo AY, Kahaleh M , Tyberg A. Clinical review of EUS-guided gastroenterostomy (EUS-GE). J Clin Gastroenterol. 2020 Jan; 54 (1): 1–7.Google Scholar Crossref PubMed
7- van der Merwe SW, van Wanrooij RLJ, Bronswijk M, Everett S, Lakhtakia S, Rimbas M , . Therapeutic endoscopic ultrasound: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2022 Feb; 54 (2): 185 – 205. Google Scholar PubMed
8- Chen YI, James TW, Agarwal A, et al. EUS-guided gastroenterostomy in management of benign gastric outlet obstruction. Endosc Int Open 2018;6:E363-8. 10.1055/s-0043-123468 [DOI] [PMC free article] [PubMed] [Google Scholar]
9- Hosono S, Ohtani H, Arimoto Y, Kanamiya Y. Endoscopic stenting versus surgical gastroenterostomy for palliation of malignant gastroduodenal obstruction: A meta-analysis. J Gastroenterol. 2007; 42: 283-290.
10- Iqbal U, Khara HS, Hu Y, Kumar V, Tufail K, Confer B, EUS-guided gastroenterostomy for the management of gastric outlet obstruction: a systematic review and meta-analysis. Endosc Ultrasound. 2020 Jan–Feb; 9 (1): 16 – 23. Google Scholar Crossref PubMed.
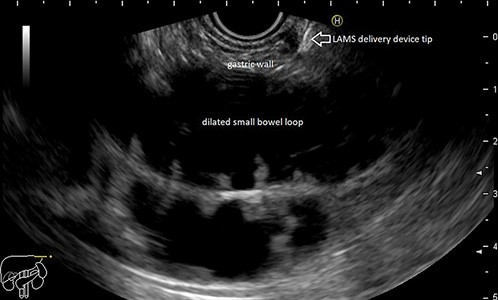
Figure 1
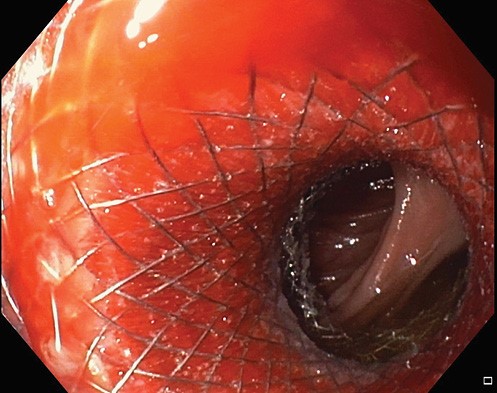
Figure 2
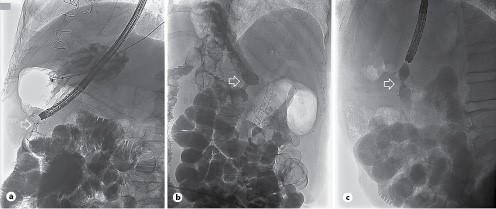
Figure 3
