Study of Patients with Centrotemporal (Rolandic) Epilepsy Aged Four to Fifteen Years that Suffer from Attention Deficit Hyperactivity Disorder
Study of Patients with Centrotemporal (Rolandic) Epilepsy Aged Four to Fifteen Years that Suffer from Attention Deficit Hyperactivity Disorder
Dr. Shivali Desai *, Dr Vijay Kolhar1, Dr Varsha2
1. Assistant Professor in Dept of Paediatrics, ESIC Medical College and Hospital Kalaburagi.
2. Senior Resident in Dept of Paediatrics, ESIC Medical College and Hospital Kalaburagi
*Correspondence to: Dr. Shivali Desai, Senior Resident in Dept of Paediatrics, ESIC Medical College and Hospital Kalaburagi.
Copyright
© 2024: Dr. Shivali Desai. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 20 Nov 2024
Published: 01 Dec 2024
Abstract
Introduction: Rolandic epilepsy (also known as benign epilepsy with centrotemporal spikes) is one of the most common focal epilepsies in childhood. Though often labeled "benign," concerns have arisen regarding its association with neurocognitive and behavioral challenges, including attention deficit hyperactivity disorder (ADHD).
Objective: This study aimed to determine the prevalence and characteristics of ADHD in children aged 4–15 diagnosed with rolandic epilepsy.
Methods: A descriptive cross-sectional study was conducted on a sample of 33 patients with typical rolandic epilepsy. Parents and teachers of these children completed the DSM-5 ADHD questionnaire and Conners scale. Data were analyzed using SPSS version 21.
Results: ADHD was identified in 36.4% of the participants, with inattentive ADHD being the most prevalent subtype. Teachers reported significantly fewer ADHD traits compared to parents. Academic difficulties were noted in nearly half the sample.
Conclusion: ADHD is a frequent comorbidity in children with rolandic epilepsy. Systematic behavioral screening during follow-up care is critical to ensure early intervention and improve outcomes.
Keywords: Rolandic epilepsy, ADHD, childhood epilepsy, neurocognitive disorders, pediatric neurology.
Study of Patients with Centrotemporal (Rolandic) Epilepsy Aged Four to Fifteen Years that Suffer from Attention Deficit Hyperactivity Disorder
Introduction
Rolandic epilepsy, often termed benign epilepsy with centrotemporal spikes, is the most prevalent focal epilepsy among children, typically appearing between ages 7 and 10. Most seizures occur during the non-rapid eye movement (NREM) sleep phase and resolve without long-term complications during adolescence. However, emerging evidence suggests potential cognitive and behavioral issues in affected children, particularly ADHD. ADHD, the most common neurobehavioral disorder in childhood, has a worldwide prevalence of 5.2%, but its incidence is notably higher in children with epilepsy.
This study explores the prevalence and characteristics of ADHD in children with rolandic epilepsy in Medellín, Colombia, based on clinical and sociodemographic factors.
Methodology
This descriptive, cross-sectional study included 33 children aged 4 to 15 years diagnosed with typical rolandic epilepsy. Participants were selected from a larger cohort involved in epilepsy genetics research. Children with atypical rolandic epilepsy, intellectual disabilities, or brain lesions were excluded.
Parents completed demographic questionnaires, the DSM-5 ADHD diagnostic tool, and the Conners scale. Teachers also provided feedback via the Conners scale and DSM-5 questionnaires. ADHD was identified when more than six positive responses were recorded on the DSM-5 or when Conners scale scores exceeded 70.
Data collection shifted to a virtual format due to the COVID-19 pandemic, and responses were analyzed using SPSS version 21.
Results
Among the 33 participants, 60.6% were female, and 24.2% had a prior ADHD diagnosis. The cumulative prevalence of ADHD, based on new diagnoses and existing cases, was 36.4%.
- Subtype distribution: Inattentive ADHD was the most common subtype, followed by the combined subtype.
- Academic challenges: Over 50% of participants experienced academic difficulties, and 18.2% had repeated a school year.
- Parental versus teacher reports: Parents identified more ADHD symptoms than teachers, a discrepancy potentially influenced by the pandemic and extended parental observation during isolation.
Table No. I Sociodemographic characteristics of a patient museum with Rolándica epilepsia (N: 33)
|
Category |
n/N (%) |
|
Age |
4-15 years |
|
of rolandic epilepsy At 3 years old |
3-11 years 9/33 (27.2%) |
|
Female |
20/33 (60.6%) |
|
Recurrence of seizures |
26/33 (78.8%) |
|
Treatment with anticonvulsants |
27/33 (81.8%) |
|
Academic support requirement |
16/33 (48.5%) |
|
School indiscipline |
17/33 (51.5%) |
|
He has repeated subjects |
8/33 (24.2%) |
|
Academic: has repeated a school year |
6/33 (18.2%) |
|
Family History 1-2 grade Rolandic epilepsy ADHD |
8/33 (24.2%) 10/33 (30.3%) |
|
Previous ADHD diagnoses Inattentive Hyperactivity Combined Non-pharmacological therapy for ADHD Drug therapy for ADHD |
8/33 (24.2%) 6/8 1/8 1/8 5/8 3/8 |
Figure No. I. Prevalence of ADHD in a sample of patients with Rolandic epilepsy, Medellín 2020 (N: 33)
Table II Distribution and subtype of ADHD in children with Rolandic epilepsy
According to DSM 5 survey applied to Parents, Medellín 2020 (N: 33)
|
ADHD subtype |
n/N ( % ) |
|
Inattentive |
4/33 (12.1%) |
|
Hyperactive |
1/33 ( 3%) |
|
Combined |
2/33 (6%) |
|
Total |
7/33 ( 21.1%) |
Table No. III Academic impact on children with ADHD,
According to DSM 5 survey applied to parents, Medellín 2020 (N:7)
|
|
n/N (%) |
|
Behaviors began before age 12 |
7/7 (100%) |
|
It affects school performance |
7/7 (100%) |
|
Discipline: warnings from the teacher |
6/7 (85.7%) |
|
He has repeated a school year |
2/7 (28.5%) |
|
He has repeated subjects |
2/7 (28.5%) |
Table IV Frequency of sociodemographic and clinical characteristics of patients with rolandic epilepsy with a previous diagnosis of ADHD and according to questionnaires applied to parents and teachers (N:12)
|
Age |
7-15 years |
|
of rolandic epilepsy |
3-10 years |
|
|
n/N (%) |
|
Female gender |
7/12 (58.3%) |
|
Anticonvulsant Treatment |
10/12 (83.3%) |
|
Recurrence of seizures |
9/12 (75%) |
|
Family history of Rolandic epilepsy |
5/12 (41.6%) |
|
Previous ADHD diagnosis |
8/12 (66%) |
|
Previous drug therapy for ADHD |
3/12 (25%) |
|
Family history of ADHD |
4/12 (33.3%) |
|
Psychological intervention |
6/12 (50%) |
|
Academic support |
8/12 (66.6%) |
Discussion
The findings reveal a significant overlap between rolandic epilepsy and ADHD, supporting previous research that links focal epilepsy with behavioral disorders. The inattentive ADHD subtype aligns with trends in similar studies. Academic struggles, noted in almost half the participants, highlight the broader cognitive impact of epilepsy.
Parental over-reporting during the pandemic, compared to teachers’ responses, suggests environmental influences on ADHD diagnosis. Additionally, the study's findings emphasize the need for genetic exploration, given a family history of rolandic epilepsy in 24.2% of participants.
Conclusion
ADHD is a common comorbidity in children with rolandic epilepsy, with significant implications for academic performance and social development. Comprehensive follow-up, including behavioral screening with validated tools like the DSM-5 and Conners scales, is essential. Early identification and intervention, involving multidisciplinary care, can enhance quality of life for these children.
References
1. Dry?a?owski P, Jó?wiak S, Franckiewicz M, Strzelecka J. Benign epilepsy with centrotemporal spikes – Current concepts of diagnosis and treatment. Neurol Neurochir Pol. 2018;459:1–13.
2. Lee YJ, Hwang SK, Kwon S. The Clinical Spectrum of Benign Epilepsy with Centro-Temporal Spikes?: a Challenge in Categorization and Predictability. J Epilepsy Res. 2017;7(1).
3. Larsson K, Eeg-olofsson O. A population based study of epilepsy in children from a Swedish county. Off J Eur Paediatr Neurol Soc. 2006;10:107–13.
4. The National Institute for Health and Clinical Excellence. Epilepsies?: diagnosis and management. NICE. 2012;
5. Wheless JW, Clarke DF, Carpenter D. Treatment of Pediatric Epilepsy: Expert Opinion, 2005. J Child Neurol. 2005;20(1):1–56.
6. Corda D, Gelisse P, Genton P, Dravet C, Baldy-Moulinier M. Incidence of drug-induced aggravation in benign epilepsy with centrotemporal spikes. Epilepsia. 2001;42(6):754–9.
7. Eom T-H, Shin J-H, Kim Y-H, Chung S-Y, Lee I-G, Kim J-M. Distributed source localization of interictal spikes in benign childhood epilepsy with centrotemporal spikes: A standardized low-resolution brain electromagnetic tomography (sLORETA) study. J Clin Neurosci. 2017 Apr;38:49–54.
8. Polanczyk G, De Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: A systematic review and metaregression analysis. Am J Psychiatry. 2007;164(6):942–8.
9. Thomas R, Sanders S, Doust J, Beller E, Glasziou P. Prevalence of attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. Pediatrics. 2015;135(4):e994–1001.
10. Wolraich ML, Hagan JF, Allan C, Chan E, Davison D, Earls M, et al. Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2019;144(4).
11. Cornejo Ochoa JW, Osío Uribe O, Sánchez Mosquera Y, Carrizosa Moog J, Sánchez Aldana G, Grisales Romero H, et al. Prevalence of attention-deficit hyperactivity disorder in Colombian children and adolescents. Rev Neurol. 2005;40 (12):716–22.
12. Pineda Salazar DA, Lopera F, Palacio JD, Ramirez D, Henao GC. Prevalence estimates of attention-deficit/hyperactivity disorder: Differential diagnoses and comorbidities in a Colombian sample. Int J Neurosci. 2003;113(1):49–71.
13. Duran MHC, Guimarães CA, Montenegro MA, Neri ML, Guerreiro MM. ADHD in idiopathic epilepsy. Arq Neuropsiquiatr. 2014;72(1):12–6.
14. Hermann B, Jones J, Dabbs K, Allen CA, Sheth R, Fine J, et al. The frequency, complications and aetiology of ADHD in new onset paediatric epilepsy. Brain. 2007;130(12):3135–48.
15. Ross EE, Stoyell SM, Kramer MA, Berg AT, Chu CJ. The natural history of seizures and neuropsychiatric symptoms in childhood epilepsy with centrotemporal spikes (CECTS). Epilepsy Behav. 2020;103:106437.
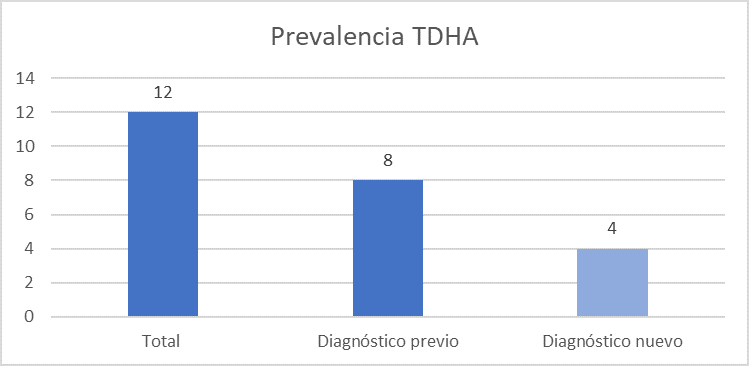
Figure 1
