Zieve’s Syndrome: A Case of Hemolytic Anemia in the Setting of Alcohol Liver Disease
Zieve’s Syndrome: A Case of Hemolytic Anemia in the Setting of Alcohol Liver Disease
Aleena Qazi*, Ayesha Alam, Mohammed Ezzeldin, Saif Elsonbaty
*Correspondence to: Aleena Qazi, Acute Medicine, Russells Hall Hospital.
Copyright
© 2024 Aleena Qazi. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 29 November 2024
Published: 06 December 2024
ABSTRACT
Zieve’s syndrome is a rare condition which typically manifests with hemolytic anemia, hyperlipidemia and jaundice in the setting of alcohol induced liver injury.
A 40-year-old male with a history of alcohol abuse presented to the same day emergency care for evaluation of 7 days of fatigue and jaundice in the setting of heavy alcohol use. The patient mentioned taking alcohol in excessive amounts but could not quantify it. Initial blood tests results were consistent with hemolytic anemia, deranged liver function tests, hyperbilirubinemia, severely deranged lipid panel and coagulopathy. A negative Direct Coomb’s test, low haptoglobin and Increased LDH was consistent with Hemolytic anemia. The pt was treated with supportive measures. The patient’s symptoms and blood investigations improved over the course of 4-day hospital admission and was discharged with statin and omega 3 acid ethyl ester to an alcohol detoxification programme with regular monitoring of his blood in our department.
Zieve’s Syndrome: A Case of Hemolytic Anemia in the Setting of Alcohol Liver Disease
Introduction
Zieve’s syndrome is a rare condition which typically manifests with hemolytic anemia, hyperlipidemia, Jaundice in the setting of alcohol induced liver injury. This is distinct from alcoholic hepatitis which may present simultaneously or develop later.
It is frequently under-diagnosed & mis-diagnosed possibly due to lack of awareness- however many studies have mentioned the prevalence of Zieve’s syndrome to be 1/1600 admissions. It is important to recognize and correctly diagnose this as the management of Zieve Syndrome greatly varies from acute alcoholic hepatitis- the latter needing steroids as a management plan.
The following is a case seen by us in our same day emergency care- appropriately managed and showed significant improvement in the following couple of weeks. This is distinct from alcoholic hepatitis which may present simultaneously or develop later and involves the use of steroids to manage the condition.
Case Presentation
We received a 40-year-old male with a history of alcohol abuse presented to the same day emergency care for evaluation of 7 days of fatigue and jaundice in the setting of heavy alcohol use. Patient mentioned taking Alcohol in excessive amount but could not quantify the amount, however the pt mentioned that he had been binging on alcohol for past few days. Patient mentioned noticing progressive yellowing of his eyes and skin afterwards. He denied any abdominal pain, nausea, vomiting, fever, itching, dark colored urine or pale stool. He had not noticed any hematemesis or melena. Denied any history of past liver disease. Initial physical assessment revealed blood pressure of 130/87 mmHg, temperature of 36.7ºC, generalized jaundice and hepatomegaly on abdominal examination. A digital rectal exam was not suggestive of digestive blood loss.
CXR was unremarkable, however initial CT Abdomen showed that the liver appeared to have diffuse slightly decreased attenuation-features suggestive of liver steatosis. Later MRI Liver had the same findings.
Initial blood revealed AST of 125, ALT of 50, Bil of 125, GGT of 2555, LDH- 319, Hemoglobin of 100, Direct and Indirect Coomb's test were negative, Haptoglobin level 0.15. Lipid profile was as follow: Cholesterol: 20.1, Triglycerides: 20.7, Calculated LDL: 11, Ferritin: 3023 The blood film showed thrombocytopenia along with acanthocytes, polychromasia, anisocytosis with schistocytes -- All features suggestive of Zieve’s syndrome.
Pt was admitted as in patient for further observation and investigations. An MRI liver was done for him which showed decreased liver attenuation, features suggestive of liver steatosis. An endoscopy was also done for him- which was normal.
Pt was symptomatically managed over the next four days along with regular observation of his blood results. On the day of discharge his blood results were as follows.
Figure 1
The patient was discharged with statin and omega 3 acid ethyl ester to an alcohol detoxification programme with regular monitoring of his blood in our department.
We continued to follow the pt in our clinic- at 2 weeks' time, his ALT came out to be 21, Bil: 28, TG: 5, Cholesterol: 14.6, Ferritin: 1060. He continued to abstain from drinking and states that he felt tremendously well in 2 weeks' time.
Discussion
Zieve’s Syndrome is a relatively rare complication of chronic Alcohol use which manifests as a triad of hemolytic anemia, Jaundice and Hyperlipidemia.
The exact pathogenesis of ZS is not completely known. Hyperlipidemia in ZS is thought to be due to by massive fat mobilization to or from a fatty liver and dysregulation of blood lipids because of injured pancreatic alpha cells [i] The protein that extracts lipids from plasma, lipoprotein lipase, is thought to be deficient, which may also lead to hyperlipidemia.
Hemolysis in people with ZS is thought to be caused by hyperlipidemia. According to Dr. Zieve, hemolysis may be caused by aberrant lipids, such as lysolecithin, and hyperlipidemia, which can damage the RBC membrane[ii]. Although hemolysis causes hyperbilirubinemia, alcoholism-related hepatocyte damage is mostly responsible for the direct bilirubin elevation that is seen. Alcohol consumption combined with a vitamin E deficiency can cause pyruvate kinase instability, which alters RBC metabolism and causes hemolysis[iii].
It is important to differentiate ZS from Alcoholic hepatitis as the treatment of the latter involves glucocorticoids. Since bilirubin is expected to be elevated in ZS patients, the Maddrey discriminant function—which is used to determine prognosis of the illness course in alcohol hepatitis—can be artificially raised in this patient population. Glucocorticoid use in ZS has been associated with higher rates of infection and morbidity in individuals who are sick[iv] . To distinguish ZS from alcoholic hepatitis, hemolytic anemia rather than macrocytic anemia should be recognized.
Conservative therapy combined with alcohol abstinence usually results in a 4–6-week resolution of symptoms. Due to the increased risk of complications from hypertriglyceridemia, plasmapheresis is recommended for high-risk individuals with significantly raised lipid levels, a history of pancreatitis, and intracerebral hemorrhage. In the case we presented hyperlipidemia dramatically improved over the course of 2 weeks following alcohol cessation. If the patient remains transfusion dependent and there is no change in liver function and hemoglobin despite alcohol abstinence, liver transplantation has been proposed as a treatment[v]
References
[i] Choudhry, Faiza DO1; Kathawa, Jolian DO1; Kerton, Kelsey DO1; Farshadsefat, Seina DO2; Piper, Marc MD, MSc2. Zieve's Syndrome Presenting With Severe Hypertriglyceridemia. ACG Case Reports Journal 6(7):p e00133, July 2019. | DOI: 10.14309/crj.0000000000000133
[ii] ZIEVE L. Jaundice, hyperlipemia and hemolytic anemia: a heretofore unrecognized syndrome associated with alcoholic fatty liver and cirrhosis. Ann Intern Med. 1958 Mar;48(3):471-96. doi: 10.7326/0003-4819-48-3-471. PMID: 13521581.
[iii] Abughanimeh O, Kaur A, Numan L, Bahaj W, Madhusudhana S. Zieve's Syndrome: An Under-reported Cause of Anemia in Alcoholics. Cureus. 2019 Feb 22;11(2):e4121. doi: 10.7759/cureus.4121. PMID: 31037235; PMCID: PMC6478496.
[iv] Rady MY, Johnson DJ, Patel B, Larson J, Helmers R. Corticosteroids influence the mortality and morbidity of acute critical illness. Crit Care. 2006;10(4):R101. doi: 10.1186/cc4971. PMID: 16846529; PMCID: PMC1750970.
[v] Abughanimeh O, Kaur A, Numan L, Bahaj W, Madhusudhana S. Zieve's Syndrome: An Under-reported Cause of Anemia in Alcoholics. Cureus. 2019 Feb 22;11(2):e4121. doi: 10.7759/cureus.4121. PMID: 31037235; PMCID: PMC6478.
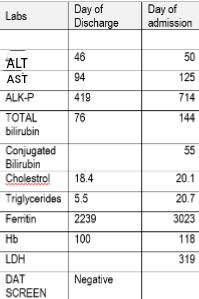
Figure 1
