Septic Complications Following Uterine Artery Embolization: A Case Report of Necrotic Degenerative Fibroid and Successful Surgical Management
Septic Complications Following Uterine Artery Embolization: A Case Report of Necrotic Degenerative Fibroid and Successful Surgical Management
Riham Desougi1, Rawia Ahmed 2, Sami Farrag 3, Mona Mohamed 4
1. Registrar ,Department of Obstetrics and Gynaecology, Limerick University Hospital, Limerick , Ireland.
2. Consultant, Department of Obstetrics and Gynaecology, Cavan General hospital, Cavan, Ireland
3. Consultant, Department of Obstetrics and Gynaecology, Cavan General hospital, Cavan, Ireland
4. Registrar, Department of Obstetrics and Gynaecology, Cavan General hospital, Cavan, Ireland.
*Correspondence to: Riham Desougi, Registrar ,Department of Obstetrics and Gynaecology, Limerick University Hospital, Limerick , Ireland.
Copyright
© 2024 Riham Desougi. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 02 November 2024
Published: 06 December 2024
DOI: https://doi.org/10.5281/zenodo.14286820
Abstract
This case report presents a 33-year-old woman who developed pyomyoma complicated by sepsis six weeks following uterine artery embolization (UAE) for symptomatic fibroids. The initial postoperative period was uneventful; however she developed pelvic discomfort progressed over weeks to severe lower abdominal pain, high-grade fever, and offensive vaginal discharge. Imaging revealed necrotic fibroids with fluid-air levels, consistent with pyomyoma. Despite initial broad-spectrum antibiotics and supportive care, the patient required surgical removal of the prolapsed necrotic fibroid. Postoperatively, the patient stabilized with targeted antibiotic therapy and supportive management, achieving full recovery. This case underscores the importance of early recognition and intervention in UAE-related complications to prevent severe outcomes and showed the potential for uterus-preserving management strategies.
Keywords: Pyomyoma, uterine artery embolization, uterine leiomyoma, sepsis, necrotic fibroid, fertility-preserving surgery.
Septic Complications Following Uterine Artery Embolization: A Case Report of Necrotic Degenerative Fibroid and Successful Surgical Management
Introduction
Pyomyoma, also known as suppurative leiomyoma, is a rare but severe complication of uterine leiomyomas characterized by an intra myometrial abscess. First described in 1871, fewer than 100 cases have been reported in the literature, with approximately 10 documented following uterine artery embolization (UAE) (Iwahashi et al., 2016). This condition arises from infection within a necrotic fibroid and is often associated with polymicrobial bacteremia, leading to systemic complications such as sepsis, septic shock, and even death if not treated promptly (Greenspoon et al., 1990). The pathophysiology involves infarction and subsequent necrosis of leiomyomas, commonly triggered by UAE, postpartum uterine changes, or post-miscarriage complications. Symptoms such as abdominal pain, fever, and elevated inflammatory markers often mimic post-embolization syndrome, which can delay diagnosis (Verma et al., 2010). Advanced cases may exhibit localized gas collections within necrotic fibroids on imaging, a key diagnostic clue (Verma et al., 2010).
Despite its rarity, pyomyoma carries significant morbidity and mortality, with untreated cases reporting mortality rates as high as 20% (Iwahashi et al., 2016). Traditionally, hysterectomy combined with broad-spectrum antibiotics has been the mainstay of treatment. However, fertility-preserving approaches, including hysteroscopic and laparoscopic drainage, are gaining attention as viable alternatives (Pinto et al., 2012; Yu et al., 2019). This case study contributes to the limited body of knowledge by exploring uterus-preserving management in critically ill patients, offering insights into alternative strategies to manage this condition.
Leiomyomas are the most common benign tumors of the uterus and are frequently associated with symptoms such as menorrhagia, dysmenorrhea, lower abdominal pain, and impaired fertility (Wallach & Vlahos, 2004). Conservative treatment options, such as high-intensity focused ultrasound (HIFU) and UAE, have emerged as alternatives to surgery. UAE, in particular, induces hemorrhagic infarction of fibroids while preserving endometrial and myometrial perfusion (Hovsepian et al., 2004). However, rare complications, such as pyomyoma, can arise, presenting as intramyometrial abscesses that may progress to bloodstream infections, sepsis, or even death (Shukla et al., 2012).
Pyomyoma remains a rare entity, with fewer than 100 cases reported, including 10 following UAE (Iwahashi et al., 2016). Symptoms such as pain, fever, and elevated inflammatory markers are often mistaken for post-embolization syndrome, delaying critical intervention (Greenspoon et al., 1990). Imaging modalities such as CT and MRI can help identify pyomyoma, particularly in cases where gas inclusions are noted. While gas is commonly observed following UAE, localized gas collection within a necrotic fibroid, along with clinical signs of infection, strongly indicates pyomyoma (Verma et al., 2010).
Historically, hysterectomy has been the definitive treatment for pyomyoma (Iwahashi et al., 2016). Nevertheless, uterus-preserving methods have shown promise in certain cases. For instance, Magro and Gafson (2014) reported successful transabdominal drainage without hysterectomy in a postpartum pyomyoma case, while Pinton et al. (2016) and Bagga et al. (2017) managed similar cases conservatively through laparotomy and myomectomy. In post-UAE cases, Pinto et al. (2012) utilized laparoscopic drainage, and Yu et al. (2019) demonstrated the feasibility of hysteroscopic treatment in a non-septic patient. More recently, Busshoff et al. (2022) showed the successful use of a hysteroscopically assisted transcervical resection in a critically ill patient with sepsis, showing the importance of individualized treatment protocols and pre-interventional risk assessment. This study aimed to provide an in-depth understanding of pyomyoma as a rare but life-threatening complication following UAE. Despite its rarity, with fewer than 100 cases documented since 1871 and only 10 following UAE, the condition is associated with high mortality rates if left untreated (Iwahashi et al., 2016). The significance of this work lies in bridging gaps in the literature regarding minimally invasive techniques, such as hysteroscopic management, particularly in critically ill patients. Findings showed the importance of early diagnosis, advanced imaging for detecting necrotic changes, and the development of pre- and post-procedural protocols to mitigate risks. This case report will provide valuable insights for clinicians managing pyomyoma, contributing to improved patient outcomes and guiding future research efforts.
Case Presentation
The patient is a 33-year-old female, Para 1, with a history of one prior cesarean section performed five years ago without complications. She was diagnosed with uterine fibroids in July 2023 during a routine gynecological examination, following complaints of menorrhagia and pelvic discomfort. Based on the size and symptomatic nature of the fibroids, she was referred to a multidisciplinary team (MDT) for further evaluation. After discussion, UAE was recommended as a minimally invasive option to preserve the uterus while addressing her symptoms. The procedure was performed on January 29, 2024. She has no history of allergies, smoking, alcohol consumption, or substance abuse. Her medical history is otherwise unremarkable, with no chronic conditions such as hypertension or diabetes. Her surgical history is limited to the cesarean section. She reported no significant family history of gynecological or infectious diseases, malignancies, or autoimmune conditions.
The patient presented to the emergency department on March 12, 2024 with a one-day history of fever and chills, and ongoing lower abdominal pain for 3 days. The pain was described as persistent, sharp, and localized predominantly in the lower abdomen, accompanied by a sensation of pressure. She also reported copious, offensive, brownish vaginal discharge, which developed on the same day as her fever. Additional symptoms included nausea and multiple episodes of non-bilious vomiting, which aggravated her overall discomfort.
The patient symptoms began three days prior to her presentation. She experienced lower abdominal pain, which progressively intensified over time. The pain was constant, sharp in nature, and localized, without radiation. She also reported high-grade fever, which she measured at home as 39.5°C, associated with chills and rigors. This was accompanied by generalized malaise and weakness.
The vaginal discharge, which was brownish and offensive, became profuse on the day of her presentation. She also reported persistent nausea throughout the day, leading to multiple episodes of vomiting, which were described as non-bilious and not associated with any specific food intake.
She had no urinary symptoms, including dysuria, hematuria, urinary frequency, or urgency. There were no bowel symptoms such as diarrhea, constipation, or blood in the stool. Additionally, she denied recent travel, exposure to infectious diseases, or new sexual partners. There was no history of recent upper respiratory symptoms or prior pelvic infections.
The patient has a history of a cesarean section performed five years ago, which was uncomplicated. In July 2023, she was diagnosed with uterine fibroids during a routine gynecological evaluation after reporting symptoms of heavy menstrual bleeding and pelvic pressure. The fibroids were deemed symptomatic and significant in size, leading to a recommendation for uterine artery embolization (UAE) as a minimally invasive, uterus-preserving treatment which was performed uneventfully on January 29,2024.
The patient has no history of chronic medical conditions such as diabetes, hypertension, cardiovascular disease, or autoimmune disorders. Additionally, she denies any prior history of pelvic inflammatory disease, tubal surgeries, sexually transmitted infections, or recurrent pelvic infections. Her surgical history is limited to the cesarean section. There is also no significant family history of gynecological or infectious diseases.
She denies the use of any other regular medications, including over-the-counter drugs or herbal remedies. She has no known allergies to drugs, food, or environmental agents.
Upon presentation to the emergency department, the patient exhibited clinical signs consistent with systemic infection. Her temperature was elevated at 38.7°C. She was hypotensive, with a blood pressure of 102/49 mmHg, and tachycardic, with a pulse rate of 126 beats per minute. Her respiratory rate was slightly elevated at 22 breaths per minute, but oxygen saturation remained within the normal range at 96% on room air.
On abdominal examination, the abdomen was soft, with mild tenderness localized to the lower quadrants, particularly over the suprapubic region. There was no evidence of rebound tenderness or guarding, and bowel sounds were normal upon auscultation. A palpable uterine fundus was noted, measuring approximately 16–18 cm, consistent with uterine enlargement. During the pelvic examination, speculum inspection revealed normal external genitalia, but there was profuse brownish vaginal discharge with a distinctly offensive odor. The discharge was thick and non-bloody. The cervix appeared intact, with no visible ulceration or erosion. Bimanual examination did not elicit cervical motion tenderness, and no adnexal masses or significant tenderness were noted.
Neurological and respiratory examinations were unremarkable, and no abnormalities were detected on inspection of the extremities. The findings strongly suggested an intrauterine or pelvic infection, likely related to her history of uterine artery embolization and necrotic fibroids. Immediate resuscitative measures were initiated, including fluid replacement and administration of broad-spectrum antibiotics, while further diagnostic workup was undertaken to confirm the underlying cause.
Initial laboratory findings revealed significant abnormalities consistent with severe systemic infection and inflammation. The patient was noted to have anemia, with a hemoglobin level of 8.8 g/dL. White blood cell (WBC) count was markedly elevated at 27.8 × 10?/L, with a neutrophil percentage of 94%, indicating a pronounced neutrophilic response typical of bacterial sepsis. Lymphopenia was also evident, with lymphocytes constituting only 3.2%.
Her C-reactive protein (CRP) level was markedly elevated at 197, indicating a significant inflammatory response. Blood cultures showed no growth after 5 days. Vaginal swabs revealed heavy growth of mixed flora, including isolates of Escherichia coli, consistent with the offensive vaginal discharge observed during the clinical examination. Aspiration of vaginal fluid cultured multiple organisms, including Escherichia coli, Prevotella bivia, Peptostreptococcus anaerobius, and Bacteroides stercoris, further confirming the diagnosis of a mixed bacterial infection. Sensitivity testing results were pending at the time of reporting.
Ultrasound imaging revealed an enlarged and heterogeneous uterus with a non-vascular hypoechoic area and a hyper-echoic wall, suggestive of a necrotic fibroid or intrauterine fluid accumulation (Figure 1). These findings indicated advanced pathology within the uterine cavity.

Figure 1 Pelvic Trans abdominal ultrasound scan
Further evaluation with MRI of the pelvis confirmed a grossly abnormal uterus containing a fluid-fluid and fluid-air level measuring 10 × 9 × 6 cm. Restricted diffusion was observed in the most posterior portion of the endometrial fluid collection, strongly indicating the presence of pus. An adjacent vaginal collection, measuring 10 × 9 × 8 cm, was also identified, but it did not show restricted diffusion, likely representing the prolapsed and necrotic portion of the fibroid (Figure 2 and 3 ). These findings were highly indicative of pyomyoma, necessitating immediate surgical intervention.

Figure 2 Pelvic MRI Sagittal view

Figure 3 Pelvic MRI Axial view
The patient clinical presentation, laboratory findings, and imaging results led to the consideration of several differential diagnoses. The most likely diagnosis was pyomyoma, given the imaging evidence of necrotic fibroids with gas-producing organisms and the patient systemic signs of sepsis, such as fever, leukocytosis, and hypotension. Endometritis with an intrauterine collection was also considered, as it can present with similar symptoms; however, the absence of diffuse endometrial thickening on imaging and the localized nature of the gas-producing collection favored pyomyoma. Pelvic inflammatory disease (PID) was considered less likely because the imaging findings showed isolated uterine involvement without any adnexal pathology, which is typically associated with PID. The combination of clinical and imaging evidence strongly supported pyomyoma as the primary diagnosis, necessitating immediate intervention.
Based on the clinical, laboratory, and imaging findings, the patient was diagnosed with pyomyoma, a necrotic and infected uterine fibroid complicated by sepsis, which developed following uterine artery embolization. This rare but severe complication required prompt and aggressive management to prevent further systemic deterioration.
The patient was initially managed in the emergency department with aggressive resuscitation. She was started on intravenous (IV) fluids, including normal saline and Ringer lactate, to address hypotension and dehydration. Broad-spectrum antibiotics were initiated empirically in consultation with the microbiology team. The initial regimen included IV Augmentin (1.2 g every 8 hours), Amikacin (15 mg/kg once daily), and IV Metronidazole (500 mg every 8 hours) to cover a wide range of potential bacterial pathogens. Antiemetics such as IV ondansetron (4 mg every 8 hours) and pain management with paracetamol (1 g every 6 hours as needed) were also administered to control symptoms.

Figure 4 Infected necrotic uterine Fibroid
After initial stabilization, surgical intervention was planned. On March 13, 2024, the patient underwent an examination under anesthesia (EUA) and surgical removal of the prolapsed degenerative fibroid under ultrasound guidance. The procedure was performed under general anesthesia. Intraoperative findings included a necrotic fibroid protruding into the vagina, filling the cervical canal, and producing copious amounts of purulent discharge. The fibroid was removed using ovum forceps, and the uterine cavity was irrigated thoroughly with 2 liters of warm saline to ensure complete removal of debris and infected material. Samples of the fibroid tissue and purulent discharge were sent for histopathological examination and microbial cultures. (Figure 4 )
Postoperatively, the patient remained hemodynamically stable and was transferred to the general ward for further care. Antibiotics were tailored based on the culture and sensitivity results, which revealed polymicrobial infection susceptible to carbapenems. The antibiotic regimen was adjusted to IV Meropenem (1 g every 8 hours), and the patient completed a 10-day course to ensure eradication of the infection. Additional supportive care included oral iron supplementation to address anemia and close monitoring of vital signs, inflammatory markers, and hematological parameters.
The patient recovered well postoperatively, with significant improvement in clinical and laboratory parameters. Her hemoglobin levels rose from 8.8 g/dL to 11.5 g/dL, and her CRP and WBC count normalized. She was discharged in stable condition with detailed instructions for home care, including adherence to oral iron supplements and hydration. A follow-up plan was established, including a repeat pelvic ultrasound scheduled in three months to monitor for any residual pathology or recurrence.
At her follow-up clinic visit, the patient reported no further symptoms. She remained afebrile, and there were no signs of recurrence of infection or fibroid-related complications. The patient expressed satisfaction with the care provided and was counseled on long-term monitoring to prevent recurrence of similar complications.
Discussion
Pyomyoma, or suppurative leiomyoma, is a rare but severe complication of uterine leiomyomas, often manifesting as an intramyometrial abscess secondary to infection of a necrotic fibroid. This condition is particularly concerning following uterine artery embolization (UAE), a minimally invasive procedure aimed at preserving the uterus while managing symptomatic fibroids. The patient presented with acute abdominal pain, fever, and offensive vaginal discharge, which are hallmark symptoms of pyomyoma. These symptoms align with findings by Iwahashi et al. (2016), who showed that the clinical presentation often mimics post-embolization syndrome, thereby delaying diagnosis. Advanced imaging techniques played a pivotal role in this case, with MRI revealing necrotic fibroids containing fluid-air levels and adjacent vaginal collections. This correlates with findings by Verma et al. (2010), who described localized gas collections within necrotic fibroids as a diagnostic clue for pyomyoma post-UAE. Blood and vaginal cultures confirming polymicrobial bacteremia further substantiated the diagnosis.
Notably, elevated inflammatory markers, severe anemia, and leukocytosis observed in this patient were consistent with systemic inflammatory response syndrome (SIRS), which has been shown in similar cases, such as those described by Pinto et al. (2012) and Yu et al. (2019). These parameters, combined with imaging findings, were critical in differentiating pyomyoma from conditions such as pelvic inflammatory disease or endometritis.
Aggressive management was key in this case, starting with broad-spectrum antibiotics to address sepsis, followed by surgical removal of the necrotic fibroid. The uterus-preserving surgical approach aligns with the growing body of literature advocating fertility-preserving strategies. For example, Magro and Gafson (2014) successfully managed postpartum pyomyoma with transabdominal drainage, and Pinto et al. (2012) utilized laparoscopic drainage in post-UAE cases. Similarly, this patient surgical intervention involved transcervical removal of the prolapsed fibroid and thorough uterine irrigation, demonstrating the feasibility of such approaches even in critically ill patients.
Tailored antibiotic therapy based on culture sensitivity was a crucial step in ensuring complete resolution of the infection. This mirrors the approach reported by Busshoff et al. (2022), who showed the importance of individualized treatment protocols for pyomyoma in septic patients.
The presented case showed the importance of multidisciplinary care in managing complex UAE-related complications. While UAE is generally considered safe, rare complications like pyomyoma necessitate heightened awareness among healthcare providers. This aligns with the findings of Greenspoon et al. (1990), who documented the significant morbidity and mortality associated with untreated pyomyoma.
A comparison with studies by Shukla et al. (2012) and Wallach and Vlahos (2004), which explored conservative treatments for fibroids, showed the need for robust pre-procedural counseling and risk assessment. Although uterus-preserving methods like UAE offer substantial benefits, they require careful patient selection to minimize complications.
The patient successful recovery, demonstrated by the resolution of symptoms, normalization of inflammatory markers, and absence of recurrence on follow-up imaging, echoes the outcomes reported by Yu et al. (2019) and Pinto et al. (2012). These studies showed that early diagnosis, timely intervention, and adherence to evidence-based protocols are pivotal in managing this rare complication.
Conclusion
This case report showed the significant risks and severe complications associated with pyomyoma following uterine artery embolization (UAE). The patient progression from mild post-procedural symptoms to severe systemic infection and sepsis underscores the critical need for timely diagnosis and intervention. The case also demonstrates the potential for UAE-related complications to escalate rapidly if left unaddressed, showed the importance of awareness and multidisciplinary management. Key Points and Findings are:
- Pyomyoma following UAE can rapidly progress from nonspecific symptoms like mild fever and pelvic discomfort to severe complications, including sepsis and systemic deterioration.
- Early diagnosis and timely surgical intervention are critical in managing pyomyoma effectively, especially in septic patients. Imaging modalities such as MRI are indispensable for accurate diagnosis.
- Uterus-preserving approaches, such as transcervical resection and targeted antibiotic therapy, can be successful in managing pyomyoma, even in critically ill patients, provided the intervention is timely.
- Multidisciplinary care is essential for managing UAE complications, involving radiologists, gynecologists, microbiologists, and critical care teams to address both the infectious and systemic components of the condition.
Implications for Clinical Practice and Further Research
Clinicians should maintain a high index of suspicion for pyomyoma in patients presenting with nonspecific post-UAE symptoms such as fever, pelvic pain, and abnormal discharge. Prompt diagnostic testing, including imaging and culture studies, is essential for early detection. Empirical broad-spectrum antibiotics should be initiated immediately in suspected cases, with adjustments made based on culture results.
Educating patients about potential complications of UAE is crucial, including the importance of follow-up care and recognizing warning signs such as fever or worsening pelvic symptoms. Pre-procedural counseling should address individual risk factors and showed the need for adherence to post-procedural monitoring.
Further research is needed to identify predictors of pyomyoma following UAE to better stratify patient risk and prevent complications. Studies exploring minimally invasive, uterus-preserving management strategies for pyomyoma could offer valuable insights into improving outcomes for women seeking fertility-preserving options. Additionally, research into the development of rapid diagnostic tests and optimization of antibiotic regimens would enhance clinical management of pyomyoma and related complications.
Ethical Considerations
Ethical considerations were integral to the management and reporting of this case. Informed consent was obtained from the patient for all diagnostic and therapeutic interventions, as well as for the publication of this case report. The patient was provided with comprehensive information about her condition, the proposed treatments, potential risks, benefits, and expected outcomes to ensure fully informed decision-making.
Confidentiality was strictly maintained throughout the process, with all personal and identifiable information removed from the case report to protect the patient privacy. The patient autonomy was respected by involving her in every stage of the decision-making process, ensuring she was supported and had adequate information to make informed choices about her care. This case report was reviewed and approved by the hospital ethics committee to ensure compliance with established ethical standards and guidelines.
Acknowledgments
The authors would like to thank the medical team involved in the diagnosis and management of this case for their invaluable contributions and dedication to patient care.
Author Contributions
All authors contributed equally to the diagnosis, management, analysis, and reporting of this case. The writing and final review of this manuscript were collaboratively undertaken by the authors.
Conflicts of Interest
The authors declare no conflicts of interest related to this case report.
Funding Sources
This case report did not receive any specific grant or funding from public, commercial, or non-profit organizations. The work was conducted as part of routine clinical practice and was not supported by external funding.
References
1. Bagga, R., Rai, R., Kalra, J., Saha, P. K., & Singh, T. (2017). An unusual cause of postabortal fever requiring prompt surgical intervention: A pyomyoma and its imaging features. Oman Medical Journal, 32(1), 73–76.
2. Busshoff, J., Thangarajah, F., & Morgenstern, B. (2022). Uterus-preserving management of pyomyoma: Case report of a rare complication after uterine artery embolization. Case Reports in Women Health, 34, e00405.
3. Busshoff, J., Thangarajah, F., & Morgenstern, B. (2022). Uterus-preserving management of pyomyoma: Case report of a rare complication after uterine artery embolization. Case Reports in Women Health, 34, e00405. https://doi.org/10.1016/j.crwh.2022.e00405
4. Greenspoon, J. S., Ault, M., James, B. A., & Kaplan, L. (1990). Pyomyoma associated with polymicrobial bacteremia and fatal septic shock: Case report and review of the literature. Obstetrics and Gynecology Survey, 45(9), 563–569.
5. Hovsepian, D. M., Siskin, G. P., & Bonn, J. (2004). Quality improvement guidelines for uterine artery embolization for symptomatic leiomyomata. Journal of Vascular and Interventional Radiology, 15(5), 535–542.
6. Iwahashi, N., Mabuchi, Y., Shiro, M., Yagi, S., Minami, S., & Ino, K. (2016). Large uterine pyomyoma in a perimenopausal female: A case report and review of 50 reported cases in the literature. Molecular and Clinical Oncology, 5(3), 527–531.
7. Magro, M., & Gafson, I. (2014). Postpartum pyomyoma: A rare complication of leiomyoma. Journal of Obstetrics and Gynaecology, 34(3), 202–203.
8. Pinto, E., Trovão, A., Leitão, S., Pina, C., Mak, F., & Lanhoso, A. (2012). Conservative laparoscopic approach to a perforated pyomyoma after uterine artery embolization. Journal of Minimally Invasive Gynecology, 19(6), 775–779.
9. Verma, S. K., Gonsalves, C. F., Baltarowich, O. H., Mitche, D. G., Lev-Toaff, A. S., & Bergin, D. (2010). Spectrum of imaging findings on MRI and CT after uterine artery embolization. Abdominal Imaging, 35(2), 118–128.
10. Wallach, E., & Vlahos, N. (2004). Uterine myomas: An overview of development, clinical features, and management. Obstetrics & Gynecology, 104(2), 393–406.
11. Yu, Q., Gabriel, G., Hoffman, M., Sanampudi, S., Jassim, T., & Raissi, D. (2019). Uterine-sparing management of pyomyoma after uterine fibroid embolization. Radiology Case Reports, 14(9), 1031–1035.

Figure 1
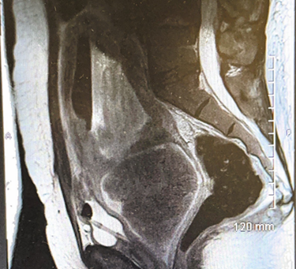
Figure 2
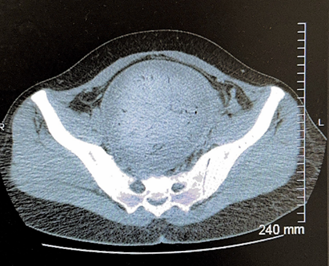
Figure 3

Figure 4
