Intramyometrial Pregnancy: A Rare Variant of Ectopic
Intramyometrial Pregnancy: A Rare Variant of Ectopic
Salma A. Gerais 1*, Mohamed A. Ahmed 2, Samar Ahmed 3, Abdelmagid Gaboura 4.
(1) Registrar of Obstetrics & Gynaecology, Our Lady of Lourdes Hospital, Drogheda, Ireland.
(2) Consultant of Obstetrics & Gynaecology, Department of Obstetrics and Gynaecology, University of Khartoum, Sudan.
(3) Registrar of Obstetrics & Gynaecology, Sligo University Hospital, Sligo, Ireland.
(4) Specialist Registrar of Obstetrics & Gynaecology, University Hospital Crosshouse, Crosshouse, Scotland, UK.
*Correspondence to: Salma A. Gerais MD, MRCOG, MRCPI. Registrar of Obstetrics & Gynaecology, Our Lady of Lourdes Hospital, Drogheda Ireland.
Copyright
© 2024 Salma A. Gerais. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 02 November 2024
Published: 09 December 2024
Intramyometrial Pregnancy: A Rare Variant of Ectopic
Background
An intramyometrial pregnancy (IMP) is an extremely rare form of ectopic pregnancy, accounting for less than 1% of all ectopic gestations [1]. It is situated within the uterine wall, surrounded by the myometrium and is completely separated from both the uterine cavity and the fallopian tubes [2]. It rarely progresses beyond 12 weeks of gestation, as the growth of the pregnancy leads to thinning of the overlying myometrium, increasing the risk of uterine rupture which accounts for 2.5% of maternal mortality [3].The pathophysiology remains unclear in the literature. Ong et al. proposed that intramyometrial ectopic pregnancy occurs due to increased lytic activity of the syncytial trophoblast combined with defective decidualization, allowing the conceptus to invade the myometrium. In a normal pregnancy, the decidua basalis attracts the trophoblast, leading to both intravascular and interstitial invasion of the inner myometrium but without the migration of the conceptus into the myometrium [4]. A systematic review conducted by Carnot N. Ntafam identified a history of curettage as the most commonly reported risk factor, observed in 30 patients (36.58%). This was followed by a history of salpingectomy, assisted reproduction with embryo transfer and previous cesarean section in 10 (12.19%), 10 (12.19%), and 9 (10.97%) patients respectively [5]. Ultrasonography was performed in 80 cases (97.56%). 66 cases reported ultrasound findings.. Of these, ultrasound findings were diagnostic or suggestive of intramyometrial pregnancy in 29 cases. Additional diagnostic methods included MRI, laparoscopy (both diagnostic and surgical) and diagnostic hysteroscopy, which were performed on 18 patients (21.95%), 36 patients (43.9%) and 22 patients (26.83%) respectively [5]. Histopathology following surgery remains the gold standard for confirming the diagnosis. Management options include conservative approaches (3.65%), medical treatment with methotrexate or potassium chloride (23.17%) and surgical interventions [5]. The mortality rate associated with intramyometrial pregnancy is approximately 2.5% [6].
Case Presentation
A 16-year-old lady, para 0+2 presented to the emergency department complaining of active vaginal bleeding after medical treatment of missed miscarriage. She had history of two recurrent miscarriages treated by surgical evacuation. Her pregnancy was spontaneous. Her medical history was unremarkable. Clinically she was vitally stable, soft abdomen, no tenderness no palpable masses. Speculum examination was suggestive of normal-looking cervix with bleeding from the os, uniformly enlarged 8 weeks size uterus freely mobile, no cervical movement tenderness, and no adnexal masses. An ultrasound demonstrated a gestational sac about 2.2 cm in diameter. It showed also a yolk sac and a fetal pole of 8 mm without cardiac cavity. Surgical suction and evacuation was performed under ultrasound guidance. During the evacuation, the gestational sac was noted to be below the suction tube, the procedure was aborted. The intrauterine products were sent for histology which showed fragments of endometrium, blood clots and fibrosed chorionic villi, no evidence of malignancy. Upon reassessment, she was still complaining of the vaginal bleeding. Beta human chorionic gonadotropin was 1450. A Trans abdominal & trans vaginal ultrasound scan showed empty cavity with thick endometrium, a gestational sac below the line of endometrium with a yolk sac and fetal pole without cardiac activity, embedded in the myometrium (Fig.1&2&3&4) .The use of 3-D ultrasound helped in confirming the diagnosis of intramyometrial pregnancy, providing highly informative and detailed imaging to support accurate clinical assessment (Fig.5&6). In view of her parity and future fertility medical treatment was discussed with and accepted by the patient. Methotrexate was administered with a single dose of 50mg given intramuscularly on day 7, the drop was less than 15%. The patient received a second dose of methotrexate .The patient was displaced due to war circumstances. She then continued to have serial pregnancy tests, not able to have quantitative B-HCG test. Her pregnancy test became negative eventually then her menstrual cycle resumed back with regular intervals.
FIG.1
FIG.2
FIG.3
FIG.4
FIG.5
FIG.6
Discussion
Intramyometrial pregnancy is a rare form of conception where the gestational sac is embedded within the myometrium. Intramyometrial pregnancies are thought to occur through myometrial invasion via microscopic tracts formed by prior uterine trauma such as from surgical procedures, curettage, hysteroscopy or cesarean sections. Additionally, some cases have been linked to in vitro fertilization and embryo transfer [7]. Common symptoms include vaginal spotting, vaginal bleeding and prolonged menstrual cycles. Until the early 1990’s, laparotomy combined with hysterectomy was the preferred treatment in most cases [7&8]. With advancement in ultrasonography, intramyometrial pregnancies can now be diagnosed before the rupture of the gestational sac [7]. A variety of conservative management options have since reduced the need for unnecessary hysterectomies. The use of methotrexate for treating extrauterine pregnancies has been widely advocated [9]. In cases where no fetal tissue is found in a histological specimen, a repeat ultrasound assessment is often warranted.
Conclusion
Intramyometrial pregnancy is indeed a rare and challenging form of ectopic pregnancy where the gestational sac implants within the myometrium, rather than the endometrial cavity. Early detection by ultrasound and Medical management with Methotrexate are crucial for optimizing outcomes and preserving fertility.
References
1. Ong C, Su LL, Chia D, Choolani M, Biswas A. Sonographic diagnosis and successful medical management of an intramural ectopic pregnancy. Journal of Clinical Ultrasound. Published online 2010:NA-NA. doi:https://doi.org/10.1002/jcu.20703
2. Telner DE, Jakubovicz D. Approach to diagnosis and management of abnormal uterine bleeding. Can Fam Physician. 2007;53(1):58-64.
3. Kirk E, Bottomley C, Bourne T. Diagnosing ectopic pregnancy and current concepts in the management of pregnancy of unknown location Hum Reprod Update. 2014;20:250–61
4.Pijenborg R, Vercruysee L, Brosens I. Deep placentation Best Pract Res Clin Obstet Gynecol. 2011;25:273–85
5. Carnot N. Ntafam, ItunuOluwa Sanusi-Musa b , Robert D. Harris c.Intramural ectopic pregnancy: An individual patient data systematic review. European Journal of Obstetrics & Gynecology and Reproductive Biology: X Volume 21, March 2024, 100272
6. Chida H, Kikuchi A, Murai M, et al. Intramural Pregnancy Implanted Into a Myometrial Defect Caused by Curettage: Diagnosis With Transvaginal Sonography and Preconception and Postconception Magnetic Resonance Imaging. Journal of Ultrasound in Medicine. 2016;35(9):2066-2067. doi:https://doi.org/10.7863/ultra.15.11071
7. Tina Verghese 1, Karim Wahba 1, Ahmar Shah 1, An interesting case of intramyometrial pregnancy, BMJ Case Rep. 2012 Mar 9
8. Falfoul A, Jadoui A, Bellasfar M, et al. Grossesse intramurale: un cas [Intramural pregnancy: a case report]. J Gynecol Obstet Biol Reprod (Paris). 1992;21(6):641-643.
9. Palti Z, Rosenn B, Goshen R, Ben-Chitrit A, Yagel S. Successful treatment of a viable cervical pregnancy with methotrexate. Am J Obstet Gynecol. 1989;161(5):1147-1148. doi:10.1016/0002-9378(89)90653-4

Figure 1

Figure 2

Figure 3
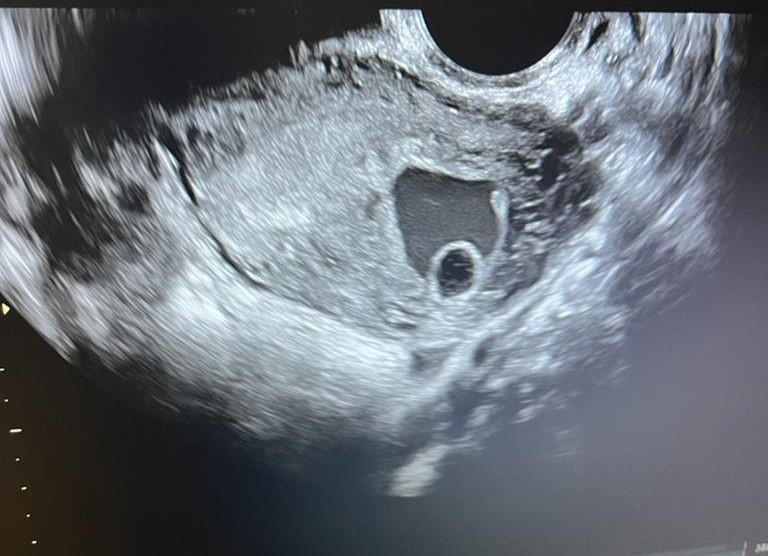
Figure 4

Figure 5

Figure 6
