Persistent Trophoblastic Tissue with Elevated hCG Post-Termination: A Case Report
Persistent Trophoblastic Tissue with Elevated hCG Post-Termination: A Case Report
Samar Ahmed 1*, Dr Nirmala Kondaveeti2, Dr Dur e Najaf Yaqub3, Dr Waqar Arshad4
1. Registrar of Obstetrics & Gynaecology, Sligo University Hospital, Sligo, Ireland.
2. Consultant Obstetrics and Gynecology, Sligo University Hospital.
3. Senior House Officer, Obstetrics and Gynecology, Sligo University Hospital.
4. GP trainee, Sligo University Hospital.
*Correspondence to: Samar Ahmed. Gerais Registrar of Obstetrics & Gynaecology, Sligo University Hospital, Sligo, Ireland.
Copyright
© 2024 Samar Ahmed. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 04 December 2024
Published: 09 December 2024
Abstract
This case report describes a 37-year-old multiparous woman with a history of multiple cesarean sections and spontaneous miscarriages who presented with persistently elevated human chorionic gonadotropin (hCG) levels post-medical termination of pregnancy. Following an extensive diagnostic and therapeutic pathway, including methotrexate (MTX), laparoscopy, and hysteroscopy, she was diagnosed with placental trophoblastic disease. This report highlights the challenges of diagnosing and managing gestational trophoblastic disease (GTD) and the importance of multidisciplinary coordination.
Keywords: Persistent β-hCG, placental trophoblastic disease, methotrexate, salpingectomy, laparoscopy, gestational trophoblastic disease
Persistent Trophoblastic Tissue with Elevated hCG Post-Termination: A Case Report
Case Presentation
Patient History: 37 year old, Resus positive, menarche at 15 yrs of age, BMMI of 30 kg/m2
Obstetric History: G6P2+3, with two previous cesarean sections, the last child born 2 years and 6 months prior, two first-trimester miscarriages managed with ERPCs in 2018, and one termination in her early 20s.
Clinical Course
The patient was referred by her general practitioner to the Fetal assessment Unit (FAU) on 11th July 2024. She was pregnant, with her last menstrual period (LMP) on 28th May 2024, and had undergone a medical termination at six weeks on 8th July 2024 with mifepristone and repeated misoprostol doses but experienced no bleeding or pain.
Ultrasound Findings: Uterine lining measuring 5.3 mm, right adnexal mass (8x6x6 mm), and no free fluid. (Fig 1)
Figure 1: USG on first visit 11/07/24
Physical Examination: Abdomen soft and non-tender, cervical os closed, mild brownish discharge, mild right-sided tenderness.
Management and follow up: Admission was offered but refused by the patient. Serum β-hCG was requested and found to be 2504 IU/L. So she was given 85 mg intramuscularly on 12th July 2024 for elevated β-hCG (2732 IU/L). Despite treatment, β-hCG levels continued to rise, reaching 5257 IU/L on 16th July 2024. Hence, a decision was made to opt fo surgical intervention. Laparoscopy with left salpingectomy, ERPC, and Mirena coil insertion was done on 17th July 2024. Intraoperative findings included a mildly dilated and hyperemic left tube, normal right tube, and no products of conception in uterine curettage. Following this, an initial reduction of serum β-hCG was seen post-laparoscopy (2765 IU/L on 17th July) with a slow decline over the following weeks.
However, despite a second dose of MTX administered on 2nd August 2024, β-hCG levels continued to elevate subsequently. A gradual decline was seen initially, but plateaued at around 305 IU/L by 28th August 2024. Due to this increasing trend, a referral to GTD (Gestational Trophoblastic Disease) Center was made. The GTD center recommended MRI pelvis, which showed heterogeneous endometrial material (ET 2.1 cm). This was followed by a CT Thorax, Abdomen, Pelvis (TAP) which revealed no additional pathology, but vascular lesion within the endometrial cavity was noted.
Further Surgical Intervention:
Hysteroscopy and D&C was performed on 14th October 2024, with pre-procedure β-hCG at 1768 IU/L (Fig 2). Histopathology confirmed placental trophoblastic disease (PTD).
Figure 2: Hysteroscopy 14/10/24
Follow-Up
Post-Hysteroscopy β-hCG dropped to 10 IU/L by 23rd October 2024 and was later undetectable. An MRI brain has been scheduled as per GTD center recommendation to rule out metastatic disease.
Discussion
This case illustrates the complexities of managing persistent trophoblastic tissue post-termination, especially with elevated β-hCG levels resistant to standard medical and surgical interventions. Key challenges included the atypical β-hCG response post-methotrexate and the need for comprehensive imaging to exclude alternative causes of hCG elevation. As early detection and earlier management improves patient outcomes in the longer run (Ngan 2021), expedited intervention and referral was made in the face of rinsing β-hCG levels. Evidence suggests that advanced investigations (MRI, PET, CT) and referral to specialized centers with better familiarity with the condition has shown to improve prognosis for this comparatively rare disease (Christianne 2021).
Conclusion
In cases of elevated β-hCG post-termination, prompt multidisciplinary intervention is essential to address potential GTD, as illustrated by this patient's outcome. Close monitoring and individualized management helped achieve biochemical resolution, underscoring the need for GTD center collaboration in complex cases.
References
1. Ngan HYS, Seckl MJ, Berkowitz RS, et al. Diagnosis and management of gestational trophoblastic disease: 2021 update. Int J Gynecol Obstet. 2021; 155(Suppl. 1): 86–93. https://doi.org/10.1002/ijgo.13877
2. Christianne Lok, Minke Frijstein, Nienke van Trommel, Clinical presentation and diagnosis of Gestational Trophoblastic Disease, Best Practice & Research Clinical Obstetrics & Gynaecology, Volume 74, 2021, https://doi.org/10.1016/j.bpobgyn.2020.12.001.
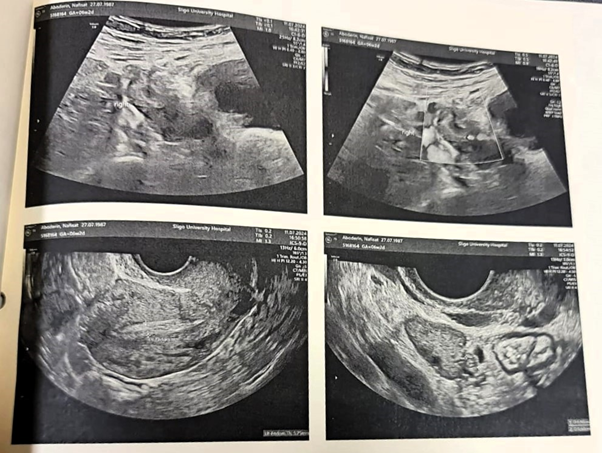
Figure 1
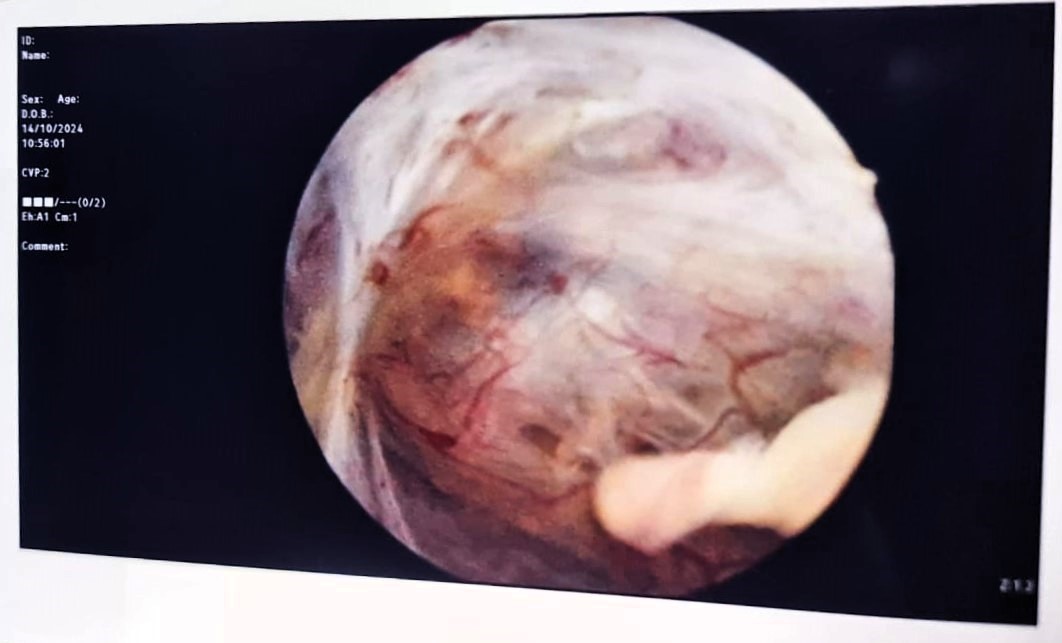
Figure 2
