Post Traumatic Desmoplastic Fibromas after Subgalial Haematoma – A Case Report
Post Traumatic Desmoplastic Fibromas after Subgalial Haematoma – A Case Report
1.Dr. Abdul Rahim H. Zwayed*,2. Dr Balola M. Godat, 3.Dr Yaqoob H Al Saadi,4. Dr Wajih K. Eshak, 5.Dr. Mowafaq J. Qassim, 6.Dr. Asma Said Al Shezawi , 7.Dr. Ganji Shiva Lingam
1, 2, 3, Department of Neurosurgery.
4, 5: Anesthesia.
6: Radiology.
7: Paediatrics.
*Correspondence to: Dr. Abdul-Rahim H. Zwayed (Ph.D.) Department of Neurosurgery.
Copyright
© 2024 Dr. Abdul-Rahim H. Zwayed, This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 25 Nov 2024
Published: 18 Dec 2024
Abstract
Desmoplastic fibroma (DF) is a rare, benign yet locally aggressive tumor of the bone. In this case report, we present a desmoplastic fibroma originating from the left frontal bone. There was a history of blunt trauma to the head about one year ago then followed by slowly growing intra osseous tumor, operation and histopathology prove to be a desmoplastic fibroma.
This is an exceptionally rare presentation of this pathology, and the associated imaging and pathologic slides are highly educational. We discuss the relevance to the literature and how to manage these patients clinically.
Keywords: Desmoplastic Fibroma; subgalial haematoma.
Post Traumatic Desmoplastic Fibromas after Subgalial Haematoma – A Case Report
Introduction
Desmoplastic fibromas are benign bone tumors that can be locally aggressive (9). It traditionally presents as an intra-osseous lesion with a high recurrence rate and infiltrative growth pattern,
They typically present in long bones and along the mandible (2). Cranial desmoplastic fibromas are exceedingly rare. The tumor is histologically and biologically similar to fibro-mitosis or desmoids (3). In the English literature, only 19 desmoplastic fibromas have been reported for cranial bones (14). Only two of these cases were in children and only one deemed congenital (5).
In this case report, we present a desmoplastic fibroma originating from the left frontal bone. There was a history of blunt trauma to the head about one year ago then followed by slowly growing intra osseous tumor, operation and histopathology prove to be a desmoplastic fibroma.
We review previously published cases and highlight the uniqueness of a desmoplastic fibroma originating within the cranium. The aim of this report is to discuss the clinical, radiological, and histological characteristics for optimal treatment of this rare skull tumor.
Case Report
A 10 years old girl with history of head injury one year ago as fall at home with subgalial swelling was brought to the pediatric office due to swelling on the left side of her head. The swelling had slowly been enlarging for the last 3 months. The mother of child reported that history of trauma and no deficits in neurologic exam were noted.
On local exam of the region, the lesion was non-painful, non-tender, firm, and consisted of about 8x7 cm swelling in the right frontal region.
Laboratory studies were all within normal limits.
Fig 1:A and B : Right frontal hard swelling
Fig 2 A and B : Head CT: Showed: expansile lytic lesion seen in the right frontal bone ,This lesion shows ground glass appearance .The diploic space is widened with displacement of the outer table .It measures 50x28 mm and no fracture seen. It causes mass effect on the frontal lobe. There is no periosteal reaction
Diagnosis at time of presentation was as: osteoma or eosinophilic granuloma. The mass was in the intra-diploic space of the right frontal bone.
Both the outer and inner tables of the calvarium were thinned. This indicates that the mass originated from inside the bone rather from the dura.
Fig :3 At time of operation with excision of the bony mass.
The child underwent surgery to remove the mass. A right frontal craniotomy was performed with excision of tumor involving the bone. The mass was approximately 50x30x5 mm in diameter and involved the outer cortex. The excision did not involve the inner cortex. The mass was completely excised with gross total resection. Haemostasis was achieved with cautery and bone wax (Figure 3).Histopathological examination of the lesion: showed multiple fragments of lesional tissue comprising of irregular branching bony trabeculae without conspicuous osteoblast riming against a fibrous stroma. Intervening fibrous stroma containing bland spindles cells without prominent cytological atypia and very rare mitosis there is a focal area showing haemorrhagic infarct and cystic space containing RBCs surrounding by hypercellular fibrous stroma containing bland spindle cells and siderophages. There is no evidence of increased mitosis, necrosis or malignancy.
Fortunately, this patient had gross total resection and remained without tumor recurrences out to a year follow up.
Impression: Desmoplastic fibroma of the cranium
Discussion
The World Health Organization defines interradicular position at presentation. A sunray radio the histological criteria for desmoplastic fibroma as that of graphic presentation, mimicking osteogenic sarcoma may a benign tumor of low to variable cellularity, whose cells be especially significant because, although it has been can be ovoid or elongated with uniform nuclei that lack any- previously described in benign intraosseous tumors, it may pleomorphism and mitotic activity supported by a wrongly lead to a diagnosis of malignancy.
In general, the radiographic features of DF are nonspecific. These include a unilocular Immunohistochemistry. Immunohistochemical stains
or multilocular, well-demarcated or irregular radiolucency may not be always helpful in distinguishing this neoplasm (7,10) with variably expressed marginal sclerosis from other spindle cell tumors and tumor-like lesions that the tumors caused cortical expansion, cortical perforation, fracture, involve the oral and maxillofacial bones. .
Further, the matrix of collagenized, variably hyalinized fibrous conn- rapid growth and bone destruction often seen in association with active tissue. The etiology of DF remains unknown, however to its clear separation of intraosseous tumors from normal trauma and endocrine and genetic factors have all been bone marrow, MRI is most valuable in surgical planning, suggested as possible etiologic agents. While most while CT is considered superior to MRI in demonstrating (2,5,6,10,11) investigators believe that DF represents the osseous the cortical breakthrough seen in 29% of patients. counterpart of soft tissue fibromatosis, others have classified it as a variant of nonossifying fibroma of bone histopathology.
Desmoplastic fibroma is an extremely rare neoplasm. It constitutes 3% of benign bone tumors and 0.06% of cranial bone tumors (7). They usually present in patients younger than 30 years old (8) The radiographic appearance can mimic many much more common bone neoplasms. The lesion is typically iso or hypodense (12). 29% have cortical breakthrough with destruction of the outer table and intradiploic space (10). Therefore, these lesions can mimic other lytic pathologies than can invade the scalp or dura (11). Typically, they present as a lump on the head and occasional with hearing loss if temporal bone is involved (4).
Differential is broad and can include eosinophilic granulomas, cavernous hemangiomas, fibrous dysplasia, fibrosarcoma, chondromyxoid fibromas (13).Other types of pathologies that present similarly on radiographic imaging include giant cell tumors, simple bone cysts, aneurysmal bone cysts, chondrosarcoma, meningioma, and metastasis (16). Therefore, getting adequate tissue for histopathology is essential. It is histologically similar to desmoid tumors (1). It is composed of fibroblasts and myofibroblasts with bland ovoid and spindle-shaped nuclei mixed in a collagenous matrix (15). Although benign, they are fast growing tumors and rarely have been reported to metastasize (17)
They can be locally aggressive with a high rate of recurrence if gross total resection in not obtained (8). Current literature suggests high recurrence after biopsy, about 50% after curettage, about 20% after subtotal resection, and 0% after gross total resection (11). Adjuvant chemotherapy and radiotherapy is not currently recommended.
In this report and review, we presented a rare case of desmoplastic fibroma of 10 year-old girl after history of trauma as subgalial haematoma.
Surgical management by wide resection and immediate reconstruction done. The tendency for local recurrence in these cases usually rare.
The obligation for surgical excision with the goal of achieving resection margins that are clear of the tumor.
Conclusion
Desmoplastic fibroma (DF) is a rare, benign yet locally aggressive tumor of the bone. In this case report, we present a desmoplastic fibroma originating from the left frontal bone. There was a history of blunt trauma to the head about one year ago then followed by slowly growing intra osseous tumor.
Diagnosis usually achieved by neurologic examinations and computerized tomography and complete by operation and histopathology which prove the diagnosis.
The clinical symptomatology is usually as painless swelling and it can mimic any soft or hard tissue swelling.
In this case of a 10 years old girl who has been treated by wide resection and immediate reconstruction with a pelvic bone graft. The tendency for local recurrence with desmoplastic fibromas of the bone highlights the obligation for surgical excision with the goal of achieving resection margins that are clear of the tumor. Radiation therapy is reserved as an adjuvant treatment in patients for whom negative resection margins cannot be obtained despite repeated attempts at surgical excision
Reference
1. Bahri I, Kallel R, Gouiaa N, (2011) Desmoplastic fibroma of the skull in an infant. Neurochirurgie 57:39–41.10.1016/j.neuchi.2010.07.003
2.Bohm P, Krober S, Greschniok A, (1996) Desmoplastic fibroma of the bone: A report of two patients, review of the literature, and therapeutic implications. Cancer 78:1011–1023.
3. Celli P, Cervoni L, Trillo G (1997) Desmoplastic fibroma of the skull: Case report and review of the literature. Neurochirurgie 43:260–264.
4. Cho BH, Tye GW, Fuller CE, (2013) Desmoplastic fibroma of the pediatric cranium: case report and review of the literature. Childs Nervous Syst 29:2311–2315. 10.1007/s00381-013-2210-9.
5. Crim JR, Gold RH, Mirra JM, (1989) Desmoplastic fibroma of bone: radiographic analysis. Radiology: 72:827–832.10.1148.
6.Deniz K, Ceylan D (2008) Desmoplastic fibroma of the skull. Acta Neurochirurgie: 150:285–290.10.1007/s00701-007-1399-3.
7. Dutt SN, Mirza S, Irving RM, (2000) Desmoplastic fibroma of the temporal bone. J Laryngol Otol 114:314–317.10.1258/0022215001905463
8. Gardini G, Minghetti G, Ferracini R (1978) Desmoplastic fibroma of frontal bone. Report of a case (author’s transl). Pathologica 70:575–579.
9. Goldberg AN, Janecka IP, Sekhar LN (1995) Desmoplastic fibroma of the skull: a case report. Otolaryngol Head Neck Surg 112:589–591 .
10. Hauben EI, Jundt G, Cleton-Jansen et al. (2005) Desmoplastic fibroma of bone: an immunohistochemical study including beta-catenin expression and mutational analysis for beta-catenin.
Hum Pathol 36:1025–1030.10.1016/j.humpath.2005.07.004
11. Hufnagel TJ, Artiles C, Piepmeier J, (1987) Desmoplastic fibroma of parietal bone simulating eosinophilic granuloma. Case report. J Neurosurg 67:449–451. 10.3171/jns.1987.67.3.0449
12. Lath R, Ranjan A, Ratnam BG, (2006) Desmoplastic fibroma of the frontal bone. Neurol India 54:314–315.10.4103/0028-3886.27166
13. Nedopil A, Raab P, Rudert M (2013) Desmoplastic fibroma: a case report with three years of clinical and radiographic observation and review of the literature. Open Orthop J 8:40–46.10.2174/1874325001307010040
14. Pensak ML, Nestok BR, Van Loveren H,(1997) Desmoplastic fibroma of the temporal bone. Am J Otol 18:627–631.
15. Rabin D, Ang LC, Megyesi J, (2003) Desmoplastic fibroma of the cranium: case report and review of the literature. Neurosurgery 52:950–954.10.1227/01.NEU.0000053025.36216.3C
16. Rastogi S, Varshney MK, Trikha V, (2008) Desmoplastic fibroma: a report of three cases at unusual locations. Joint Bone Spine 75:222–225.10.1016/j.jbspin.2007.04.020
17. Wolfe SQ, Cervantes L, Olavarria G, et al. (2005) Desmoplastic fibroma of the pediatric skull: Report of three cases. J Neurosurg 103:362–365.10.3171/ped.2005.103.4.0362
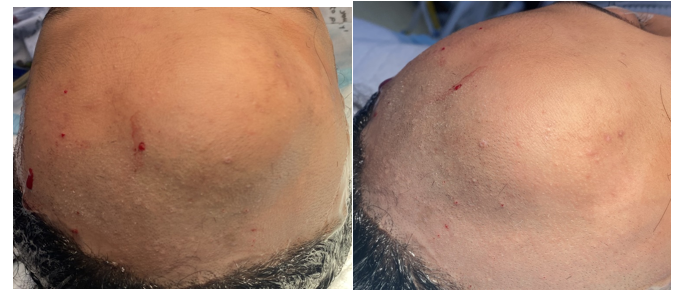
Figure 1
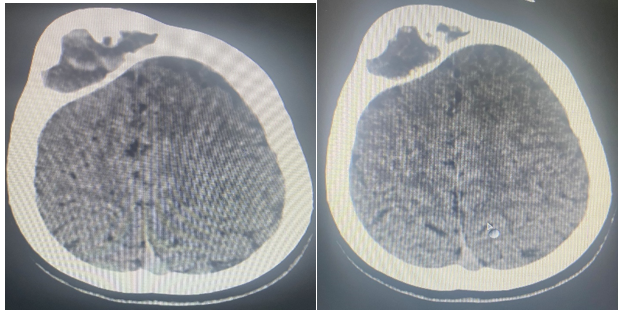
Figure 2
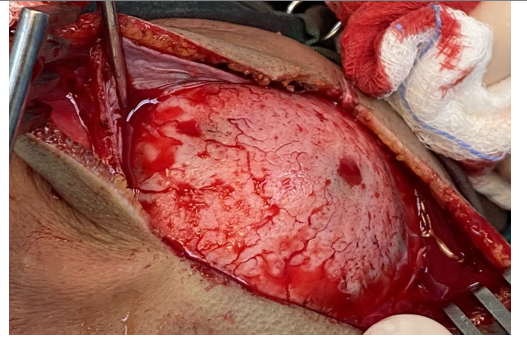
Figure 3
