Evaluation of the Efficacy with the early use of Topical Capsaicin and Alpha Lipoic Acid as Treatment for Chemotherapy-Induced Neuropathy.
Evaluation of the Efficacy with the early use of Topical Capsaicin and Alpha Lipoic Acid as Treatment for Chemotherapy-Induced Neuropathy.
Lucia Richter¹*, Wendy Rojas², Carmen Pinto³, Gilda Barrera?, Erika Sanjinez?
1) Clinical Oncologist, Caja Petrolera de Salud
(2) Anesthesiologist, Aliviar - Specialized Center for Comprehensive Pain Treatment
(3) Specialist in Biostatistics Applied to Clinical Research, Aliviar - Specialized Center for Comprehensive Pain Treatment
(4) Clinical Oncologist, Caja Petrolera de Salud
(5) Internal Medicine Specialist, Caja Petrolera de Salud
*Correspondence to: Lucia Richter, Clinical Oncologist, Caja Petrolera de Salud.
Copyright.
© 2025 Lucia Richter This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 19 January 2025
Published: 31 January 2025
Abstract
Background: Esophageal cancer, a leading cause of global cancer-related deaths, requires standard chemotherapy treatment. While studies show comparable efficacy in older adults, they face increased chemotherapy toxicity risks. The issue is similar with radiotherapy. However, clinical trials predominantly involve younger individuals, leaving an optimal treatment regimen for older esophageal cancer patients undefined.
Methods: The study included 97 esophageal cancer patients aged ≥65. All received 50.4 GY external beam radiation over 5 weeks. Of these, 53 patients had 5-Fluorouracil/Cisplatin (first and last week of radiation), while 54 had Paclitaxel/Carboplatin AUC 2 (weekly) with radiation. A standardized follow-up schedule included assessments at 3, 6, 12-, 24-, 36-, and 60-months post-treatment.
Results: A total 97 patients were enrolled in this study between July 2015 to May 2020. In both the groups, majority of the subjects were between 65 to 69 years. The rate of febrile neutropenia was higher in 5FU/Cisplatin arm (80% vs 56.8%). Cardiovascular toxicities were less commonly seen in both groups with no significant difference in grade of toxicity. Among gastrointestinal toxicities, nausea/ vomiting was common in both groups but grade 2 or higher was common in 5fu/ Cisplatin arm. Diarrhea was also commonly noted in 5FU/Cisplatin arm. Most common neurological toxicity was peripheral sensory neuropathy that was common in paclitaxel/carboplatin arm. There was no significant difference between the two groups with regards to overall survival and disease-free survival at 3 year and at 5 year of follow up
Conclusions: Concurrent chemoradiotherapy with 5FU/Cisplatin is equally effective to paclitaxel/carboplatin in terms of treatment response, OS, or DFS in elderly patients with oesophageal squamous cell cancer.
Keywords: Oesophageal cancer, concurrent chemoradiotherapy, 5-Fluorouracil/Cisplatin, Paclitaxel/Carboplatin, efficacy, toxicity.
Evaluation of the Efficacy with the early use of Topical Capsaicin and Alpha Lipoic Acid as Treatment for Chemotherapy-Induced Neuropathy.
Background
Chemotherapy-induced peripheral neuropathy (CIPN) presents a significant challenge due to the neurotoxic potential of chemotherapy agents. Various factors, including increased cancer incidence paired with improved survival rates, have contributed to the rising prevalence of CIPN. It can occur acutely during chemotherapy and, if severe, may require a reduction in the chemotherapy dose or even treatment discontinuation. This is referred to as dose-limiting toxicity, which can significantly impact treatment efficacy and patient survival (Colvin, 2019a).
In most cases, CIPN symptoms improve once chemotherapy is completed, but in some cases, symptoms persist for months or even years (Gordon-Williams & Farquhar-Smith, 2020). Approximately 30% of patients continue to experience symptoms one year or more after treatment. This phenomenon is known as "carryover." The prevalence of CIPN is around 68% one month after completing chemotherapy, decreasing to 60% at three months and 30% at six months or later (Colvin, 2019a).
The incidence of CIPN varies depending on the chemotherapy agent, dose, duration of exposure, and assessment method. Agents with the highest incidence include platinum derivatives, taxanes, vinca alkaloids, and bortezomib (Mols et al., 2014).
While different agents exhibit variable characteristics, the symptoms are predominantly sensory, making CIPN the most common toxicity. Symptoms are classified as “positive” or “negative.” Negative symptoms include numbness, loss of vibration sense, proprioception, and deep tendon reflexes. Positive symptoms include paresthesia, dysesthesia, cold hypersensitivity, and mechanical hypersensitivity. Neuropathic pain often follows sensory symptoms.
Motor symptoms, though less common, may include weakness, atrophy, and diminished reflexes. These symptoms are dose-dependent, worsening with continued treatment and the combination of antineoplastic agents (Desforges et al., 2022).
The pathophysiology of CIPN is complex, involving multiple factors and processes that vary with different chemotherapy agents. Patients with diabetes or pre-existing peripheral neuropathy are at higher risk of developing CIPN (Kerckhove et al., 2017).
Key mechanisms responsible for CIPN include mitochondrial toxicity and oxidative stress, DNA damage, disruption of axonal transport, loss of intraepidermal nerve fibers (IENF), remodeling of peripheral nerve channels, and alterations in mitogen-activated protein kinase (MAPK) pathways, among others (Kerckhove et al., 2017).
Taxanes and vinca alkaloids act on microtubules, causing dysfunction. Loss of functional microtubules disrupts the transport of cellular products essential for axonal function and structure. Platinum agents alter DNA structure and appear to induce neuronal toxicity primarily through the dorsal root ganglia. Oxaliplatin specifically induces acute neuropathy via alterations in voltage-gated sodium channels (Kerckhove et al., 2017).
Preventing and treating CIPN is highly challenging due to the diverse underlying mechanisms. Although many hypotheses have been proposed, no mechanism-based treatment has led to viable interventions. Currently, no preventive therapy has shown significant clinical efficacy for CIPN pain. According to ASCO and ESMO guidelines, no pharmacological agents are recommended or effective for preventing CIPN (Jordan et al., 2020; Loprinzi et al., 2020).
Following general recommendations for managing neuropathic pain might be logical, but evidence for agents like gabapentinoids and amitriptyline is weak. Based on the scarcity of consistent and high-quality evidence, no agents are recommended for CIPN prevention. However, moderate evidence supports duloxetine treatment, which improves pain scores, function, and quality of life, with few severe side effects reported (Hershman, n.d.).
Capsaicin, a TRPV1 receptor agonist, reduces chronic neuropathic pain by desensitizing nerves to pain signals (Cabezón-Gutiérrez et al., 2020). Various studies have demonstrated good pain relief in several types of neuropathic pain, including herpes zoster, HIV, and diabetes mellitus. Topical formulations of capsaicin, including low-concentration creams for daily use and patches, are widely available (Bhaskar et al., n.d.). However, in our region, capsaicin patches are unavailable, and the topical application of 8% capsaicin causes severe hyperalgesia, limiting its use.
Another medication recently studied for pain management is alpha-lipoic acid (ALA), which possesses chemoprotective properties and can prevent peripheral nerve damage. ALA is a physiological antioxidant that has been extensively studied as a treatment for diabetic neuropathy. It has demonstrated efficacy in treating distal sensorimotor neuropathy, modulating peripheral neuropathy, and reducing pain in diabetic patients. Its neuroprotective mechanism involves reducing oxidative stress caused by free radicals. Thus, the systemic oxidation of platinum derivatives resulting from chemotherapy may be modulated by ALA’s antioxidant effects. Indeed, it was found effective in a small open-label pilot study when administered alongside oxaliplatin (Guo et al., 2014).
Given the scarcity of effective pharmacological or non-pharmacological agents for CIPN and the reliance on protocols designed for managing other neuropathic pain types, such as diabetic peripheral neuropathy, this study evaluates the effectiveness and potential synergistic effect of capsaicin, alpha-lipoic acid, and duloxetine in CIPN.
Objective
To evaluate the effectiveness of treatment with capsaicin and alpha-lipoic acid, combined with duloxetine, for the early management of chemotherapy-induced neuropathy.
Methodological Design
We conducted a prospective descriptive study with convenience sampling at the Aliviar Clinic in Santa Cruz, Bolivia, and the Santa Cruz de la Sierra affiliate of the Caja Petrolera de Salud, from October 2023 to October 2024.
Inclusion Criteria:
All patients with a recent cancer diagnosis, regardless of disease stage, who were candidates for chemotherapy with taxanes, platinum salts, and/or vinca alkaloids, and who had not received any prior treatment.
The follow-up lasted 12 months and was divided into four evaluations using consistent instruments. The first evaluation was conducted at the time of peripheral neuropathy diagnosis. Each patient underwent two assessments before each chemotherapy cycle using two validated tools for diagnosing chemotherapy-induced neuropathy (DN4 and CTCAE v5.0). Additional evaluations were performed at 3, 6, and 12 months, completing the follow-up process.
Exclusion Criteria:
Patients diagnosed with diabetes-induced neuropathy were excluded.
Treatment Protocol:
- If DN4 >3 and/or Grade 1 on the CTCAE Scale:
- Duloxetine 30 mg orally + B-complex + Alpha-lipoic acid 600 mg/day
- 5% lidocaine gel applied to hands and feet, followed by:
- 0.075% capsaicin cream applied to hands and feet
- For patients unresponsive to the baseline regimen (VAS >4):
- Ketamine 10 mg + 5 ml lidocaine IV in 500 ml of 0.9% saline over 3 hours
Diagnoses, evaluations, treatment, and follow-ups were conducted by the same medical team over the 12-month study period.
Statistical Analysis:
All statistical analyses were conducted using SPSS 27.0, with graphs generated in Excel. Descriptive statistics were used to determine ranges, means, and standard deviations.
Results
A total of 29 patients with a cancer diagnosis, regardless of stage, who had not started chemotherapy and were scheduled to receive either monotherapy or polychemotherapy with platinum salts, taxanes, or vinca alkaloids, were included in the study. The follow-up period lasted 12 months. Neuropathy assessments were conducted using the DN4 and CTCAE v5.0 tests prior to each chemotherapy cycle, as previously described.
Age at Diagnosis: The mean age at diagnosis was 57 years.
Risk Factors: 34% of patients had at least one risk factor for developing neuropathy, the most common being alcohol consumption (4 patients).
Exclusions: Patients with type 2 diabetes mellitus (T2DM) and diabetic neuropathy were excluded. The most common primary tumor was breast cancer (6 patients), followed by head and neck cancer (5 patients), lung cancer (3 patients), prostate cancer (2 patients), and one case each of stomach, pancreas, cervix, gallbladder, and testicular cancer. The majority of patients (41%) presented at stage IV. The average number of chemotherapy cycles per patient was 7.
Chemotherapy Agents Used: 37% (11 patients) received docetaxel, 27.5% (8 patients) received cisplatin, 24.1% (7 patients) received paclitaxel, 20.6% (6 patients) received carboplatin, 2 patients received oxaliplatin, 2 patients received doxorubicin,1 patient received nab-paclitaxel.
Combination Therapies: Only 2 patients received monotherapy with docetaxel. The most commonly used combination regimens were: Carboplatin + paclitaxel (17.2%) and DCF (docetaxel, and cisplatin) regimen (17.2%, 5 patients).
Table 1 presents detailed patient characteristics and treatment distributions.
|
Age |
57 años (33-78) |
|
Risk Factor |
34% |
|
Primary Tumor |
Breast 6pctes (20.6%) Head and neck 5pctes (17.2%) Lung 3pctes (10.3 %) Próstate 2pctes (6.8%) Cervix 1pcte (3.44) Colon 1pcte Páncreas 1pcte Ovaries 1pcte Gastric 1pcte Rectal 1pcte Gallblader 1pcte Testícle 1pcte
|
|
Stage |
I 0pctes II 4pctes III 8pctes IV 12pctes |
|
Chemotherapy |
Monotherapy 2pctes polichemotherapy 22pctes |
|
Type of Chemotherapy |
Carboplatine – Paclitaxel 5 pctes DCF 5 pctes AC 3 pctes TC 3 pctes Xelox 2 pctes Docetaxel 2 pctes CDDP – Gemcitabine 1 pcte CDDP – Etoposide 1 pcte PEB 1 pcte Nab Paclitaxel – gemcitabine 1 pcte
|
Table 1. Characteristics
Analysis of Variance (ANOVA):
ANOVA, a statistical method used to compare variances between group means, was employed to determine whether significant differences existed among the means of different groups.
Multiple Linear Regression:
A versatile statistical model, multiple linear regression was applied to assess the relationships between a continuous outcome variable and its predictors. These predictors could include continuous, categorical, or derived variables, supporting non-linear relationships.
Regarding the DN4 Test Results:The majority of patients presented with a DN4 score ≥4 by the second chemotherapy cycle (7 patients). By the third cycle, 5 patients had a score ≥4, and by the fourth cycle, 4 patients had initiated treatment.
Average DN4 Scores: Baseline: 4.73, 3 months after starting treatment: 2.47, 6 months after starting treatment: 2.20, 12 months after starting treatment: 1.05
These results indicate a clear linear regression in DN4 scores as treatment progressed, showing a consistent improvement in neuropathy symptoms over time. Figures 1, 2, and 3 (not included here) visually represent this regression and demonstrate the effectiveness of the treatment protocol in reducing DN4 scores across the observed timeframe.
Dependent Variables and Credible Intervals
|
Dependent Variable |
Mode |
Mean |
Variance |
Lower Limit |
Upper Limit |
|
DN4 |
4.73 |
4.73 |
0.000 |
4.70 |
4.76 |
|
3 months |
2.47 |
2.47 |
0.000 |
2.44 |
2.50 |
|
6 months |
2.02 |
2.02 |
0.000 |
1.99 |
2.05 |
|
12 months |
1.05 |
1.05 |
0.000 |
1.01 |
1.08 |
This table shows the progression of DN4 scores over the follow-up period. The decreasing mean scores from baseline to 12 months reflect a significant improvement in neuropathy symptoms with the proposed treatment. The narrow credible intervals indicate high precision and consistency in the results.
Fig1. Linear Regression for DN4 Scores in Neuropathy Treatment
The linear regression analysis performed for DN4 scores demonstrates a significant decline in neuropathy severity over the course of the treatment. This analysis provides a statistical confirmation of the observed trend, highlighting the effectiveness of the treatment protocol.
Key Observations from Linear Regression: Initial DN4 Score (Baseline): The mean score was 4.73, reflecting severe neuropathic symptoms.
Post-Treatment Scores: At 3 months: 2.47, At 6 months: 2.20, At 12 months: 1.05
The consistent reduction indicates significant symptom improvement. The regression analysis confirms a steady downward slope, indicating that the longer the treatment duration, the greater the improvement in neuropathic symptoms. This regression provides robust evidence for the efficacy of combining topical capsaicin, alpha-lipoic acid, and duloxetine in reducing chemotherapy-induced neuropathy symptoms.
Fig 2. Lineal Regression at 3 months follow up
Fig3. Lineal Regression at 6 months follow up
Fig4. Lineal Regression at 12 months follow up
Regarding the CTCAE v5.0 Test Results: The mean CTCAE v5.0 score was 1.5 at baseline, decreasing to 0.92 at 3 months, 0.41 at 6 months, and 0.15 at 12 months of follow-up (Table 3).
|
Dependent Variable |
Posterior |
95% Intervalo creíble |
|||
|
Mode |
Mean |
Variance |
Lower limit |
Upper limit |
|
|
CTAE at treatment start |
1,53 |
1,53 |
,000 |
1,52 |
1,55 |
|
CTEA at 3 months |
,92 |
,92 |
,000 |
,90 |
,93 |
|
CTEA at 6 months |
,41 |
,41 |
,000 |
,40 |
,42 |
|
CTEA at 12 months 12 |
,15 |
,15 |
,000 |
,14 |
,16 |
Table 2. CTCAE v5.0
Regarding Symptomatology: The most common symptoms observed were paresthesias in the palms and soles, associated with hyperalgesia, followed by a sensation of heat (Fig. 5).
Symptom Distribution: 5 patients experienced paresthesias associated with allodynia and a sensation of heat in the palms and soles, 5 patients experienced paresthesias associated with hiperalgesia, 2 patients experienced paresthesias with hyperalgesia and heat, 1 patient presented only a negative symptom (cold). In 7 patients, the chemotherapy dose was reduced after the onset of initial symptoms. At 3 months, none of these 7 patients required further dose reductions.
Fig 5. Síntomas iniciales de neuropatía
Regarding Positive Symptoms: Paresthesia in the hands was not only the most common symptom at the onset of neuropathy but also showed a significant reduction with the initiation of treatment at 3, 6, and 12 months (Figures 6, 7, and 8).
Mortality Data: By the end of the study, 62% of the patients had passed away. None of the deaths were related to the proposed treatment for neuropathy. Only 1 patient passed away within the first 3 months.
Treatment Completion: 18 patients completed the treatment at 12 months, which marked the study closure. Patients who continued to experience neuropathy symptoms at the end of the study remained on treatment.
Fig 6, Fig 7, Fig 8
Treatment Adjustments In 3 patients, no improvement was observed with the proposed treatment protocol after initiation. In these cases, the second-line treatment for peripheral neuropathy, as per current guidelines, was implemented. This included: Second-line treatment: Ketamine 10 mg + 5 ml lidocaine IV in 500 ml of 0.9% saline over 3 hours. Additional intervention: A reduction in chemotherapy dosage. Following these adjustments, symptom improvement was observed in all three patients.
Discussion
Chemotherapy-induced peripheral neuropathy (CIPN) is a significant challenge due to the neurotoxic potential of chemotherapy agents commonly used in oncology. CIPN can occur acutely during chemotherapy, which aligns with our study, where 7 patients developed initial symptoms of peripheral neuropathy and required treatment initiation. This is critically important because, in metastatic disease, chemotherapy may be prolonged, and for patients receiving adjuvant therapy, the average number of cycles is 6. CIPN is a dose-limiting toxicity, meaning that oncologists often need to reduce the treatment dose or even discontinue chemotherapy if supportive treatment is ineffective, with corresponding implications (Colvin, 2019a). In our study, 7 patients required dose reductions at the onset of neuropathic symptoms. However, after starting the proposed treatment regimen, symptom improvement was observed, and by the third cycle, standard doses could be resumed.
The neuropathy was evaluated using the DN4 (Douleur Neuropathique in 4 Questions) and CTCAE v.5. DN4 is a screening tool for neuropathic pain validated in various neurological conditions, including diabetic neuropathy and chemotherapy-induced neuropathy (Maihöfner et al., n.d.). It consists of interview questions and physical tests performed on the patient (Annex 1). Recently, several detection tools have been developed to differentiate neuropathic pain from nociceptive pain. The DN4 score enables this evaluation and is an easy-to-administer, short-duration screening tool, making it feasible for routine consultations (Spallone et al., 2012). One of the reasons we selected DN4 for this study is its inclusion of three clinical examination items among the available screening tools. The DN4 score increases not only with the severity of neuropathic symptoms but also with the degree of neuropathic deficit and nerve conduction abnormalities. These factors underscore the absolute relevance of DN4 for evaluating nerve function.
The CTCAE v5.0 terminology developed by the National Cancer Institute (NCI) is a descriptive system used for reporting adverse events (AEs). Each adverse event has its own grading scale. The grade indicates the severity of the AE, ranging from 1 (mild) to 5 (severe) (Cancer Institute, 2017).
We included patients receiving chemotherapy agents most commonly associated with peripheral neuropathy. Bortezomib was excluded, as our service does not handle onco-hematological patients.
Platinum-Based Compounds: These agents cause neuronal damage at the mitochondrial level, oxidative stress, and ion channel dysfunction. These effects are directly linked to electrophysiological abnormalities in peripheral nerves. Cisplatin inhibits mitochondrial DNA replication and transcription. Studies have shown that cisplatin induces pro-apoptotic changes in the sciatic nerves of treated mice (Kerckhove et al., 2017). Oxaliplatin: Ion channels are a toxic target for platinum-based compounds, particularly oxaliplatin. A single administration of oxaliplatin in mice induced neuronal hyperexcitability by reducing the expression of potassium channels (TREK1 and TRAAK) and increasing HCN channels in dorsal root ganglion (DRG) neurons. Oxaliplatin exhibits significant neurotoxicity, qualitatively and quantitatively distinct from other neurotoxic agents. It is responsible for acute neuropathic alterations such as paresthesia and dysesthesia in the hands, feet, and perioral area triggered by cold stimuli, occurring hours or days after chemotherapy infusion (Balayssac et al., 2011).
At the beginning of chemotherapy cycles, this acute neuropathy generally resolves within a week and disappears before the next cycle. However, repeated cycles increase the risk of developing chronic chemotherapy-induced peripheral neuropathy (CIPN). In our study, the average number of chemotherapy cycles was 7, consistent with literature findings that patients receiving these agents commonly experience this adverse effect (Balayssac et al., 2011).
Although symptoms tend to decrease over time, long-term clinical studies suggest that neuropathy persists in some patients. At 24 months, 37.5% of patients experience grade 1 symptoms, 29.2% grade 2, and 0.7% grade 3. At 48 months, 11.9% present grade 1, 2.8% grade 2, and 0.7% grade 3 symptoms. In our study, one patient who received oxaliplatin developed initial neuropathy symptoms during the 4th treatment cycle, requiring a dose reduction and initiation of the proposed regimen. Although symptoms were controlled, allowing resumption of the standard dose, this patient exhibited grade 1 paresthesias in the lower and upper limbs at 12 months of follow-up, consistent with findings from Balayssac et al. (2011).
Oxidative stress is one of the mechanisms implicated in taxane-induced peripheral neuropathy, affecting neuronal and non-neuronal cells in the peripheral nervous system (PNS). This process includes macrophage activation in the dorsal root ganglion and peripheral nerves, as well as microglial activation in the spinal cord (Ledeboer et al., 2007).
Among patients treated with adjuvant paclitaxel, 80–97% experienced neuropathy symptoms, with the onset of CIPN ranging from 1 to 101 weeks. In this study, patients receiving paclitaxel began to exhibit neuropathy symptoms by the third cycle. Symptoms were more frequent in those receiving a regimen every 21 days compared to a weekly schedule.
A higher percentage of neuropathy was observed in patients receiving paclitaxel compared to docetaxel, aligning with findings in the literature. Thorton et al. (2008) reported that patients who received taxanes experienced lasting emotional distress and impaired mental quality of life (QoL) years after chemotherapy. While our study did not evaluate the long-term emotional impact, this could be a potential area of future research for the patients included in this study.
The predominant symptoms observed were paresthesias in the palms and soles, associated with hyperalgesia or allodynia. Peripheral axons, particularly the longest ones, are more vulnerable, and sensory symptoms typically begin in the lower extremities, followed by the upper extremities. These symptoms often spread distally in a symmetrical "stocking-and-glove" distribution. However, in our study, this pattern was not reflected, as most patients experienced symptoms simultaneously in their hands and feet. Some studies have reported that this simultaneous presentation can occur in up to 68% of cases (Maihöfner et al., n.d.).
Peripheral symptom combinations are more commonly seen in patients receiving polychemotherapy regimens (Balayssac et al., 2011). This aligns with our findings, where only two patients received monotherapy regimens. Interestingly, cold-related symptoms were rare in our study, with only one patient reporting them (hypoalgesia).
Currently, no preventive therapy has shown significant clinical efficacy for chemotherapy-induced peripheral neuropathy (CIPN) pain. Following general recommendations for neuropathic pain management seems logical, but evidence for agents such as gabapentinoids and amitriptyline remains weak (Colvin, 2019b). Based on the lack of consistent and high-quality evidence, no agents are recommended for the prevention of CIPN. However, the best available data moderately support duloxetine for treatment (Hershman et al., 2014). In addition to improving pain scores, duloxetine has been shown to enhance function and quality of life, with few reports of severe side effects (Lavoie Smith et al., n.d.).
The use of 8% capsaicin has been associated with severe hyperalgesia, limiting its indication. However, studies on a 0.075% formulation have demonstrated its efficacy in treating dysesthetic pain, making it a therapeutic alternative for this type of pain. Capsaicin selectively stimulates unmyelinated C fibers, causing the release of substance P and possibly other neurotransmitters, ultimately depleting substance P. This process alters pain transmission to central systems, resulting in desensitization. Importantly, capsaicin does not cause significant systemic side effects.
The primary indication for topical capsaicin is as an adjuvant to antidepressants and anticonvulsants, as it appears insufficient as a standalone therapy (Vidal et al., 2004). In our study, we used the 0.075% concentration, based on Vidal et al.'s findings, which demonstrated good tolerability, especially regarding the itching that topical capsaicin can cause.
Alpha-lipoic acid (ALA) may reduce the risk of oxidative damage by acting as an antioxidant and regenerating other antioxidants, thereby decreasing oxidative stress, particularly in conditions involving central sensitization.
A possible pathophysiological relationship between cancer and lipid peroxidation has been described, suggesting that preventing this process through the use of antioxidants, such as ALA, could be essential in preventing different types of malignant tumors. Furthermore, antioxidants may induce apoptosis in some neoplastic cells and serve as adjuvants to chemotherapeutic agents (Durand & Mach, 2013).
Another drug included in the study was lidocaine, whose systemic clinical use has introduced a new modality for managing intractable neuropathic pain (Mao & Chen, n.d.). Additionally, lidocaine reduces the burning or itching sensation caused by capsaicin by providing a pre-application anesthetic effect, which justified its inclusion in a sequential regimen.
What Happens When Patients Do Not Respond to Treatment? In our study, three patients did not respond to early treatment initiation. When a patient does not respond to conventional therapies, hospitalization for continuous intravenous lidocaine infusion may be required.
Ketamine is another drug used in this scenario. Its analgesic effect is primarily attributed to its antagonism of N-methyl-D-aspartate (NMDA) excitatory receptors. Ketamine is an anesthetic used in cases of pain crises at low doses and can be administered intravenously, starting at 2.5–5 mg/kg/24 hours (CRUCIANI, n.d.). In the three patients who did not respond to the initial regimen, intravenous lidocaine and ketamine were used as second-line treatments. Significant symptom improvement was observed. Although this study was not designed to evaluate this protocol, it could generate hypotheses for future research. Intravenous infusions of lidocaine and ketamine have been proposed for refractory neuropathy unresponsive to standard treatment and are included in some neuropathic pain management guidelines.
Patients undergoing chemotherapy are often on multiple medications, increasing the risk of drug interactions. Our regimen, based on a combination of drugs, was designed to achieve a synergistic effect for enhanced analgesia with fewer side effects, acting through different mechanisms.
The addition of topical treatment offers several advantages are Absence of significant systemic side effects, lack of drug interactions and ease of application.
Conclusion
Although this study involved a limited number of patients, the positive results observed in the majority of cases using the proposed regimen for managing chemotherapy-induced peripheral neuropathy (CIPN), along with the absence of severe side effects or drug interactions, suggest that this regimen could be considered for managing this adverse event. This is particularly relevant in our setting, where capsaicin patches are unavailable.
References
1. Balayssac, D., Ferrier, J., Descoeur, J., Ling, B., Pezet, D., Eschalier, A., & Authier, N. (2011). Chemotherapy-induced peripheral neuropathies: From clinical relevance to preclinical evidence. In Expert Opinion on Drug Safety (Vol. 10, Issue 3, pp. 407–417). Informa Healthcare. https://doi.org/10.1517/14740338.2011.543417
2. Bhaskar, A., Nadstawek, J., Viel, E. J., Buonocore, M., López Millán, J. M., & Jaeger, H. (n.d.). Capsaicina al 8% para controlar el dolor neuropático periférico: una estrategia basada en casos clínicos.
3. Cabezón-Gutiérrez, L., Custodio-Cabello, S., Palka-Kotlowska, M., & Khosravi-Shahi, P. (2020). High-Dose 8% Capsaicin Patch in Treatment of Chemotherapy-Induced Peripheral Neuropathy. A Systematic Review. In Journal of Pain and Symptom Management (Vol. 60, Issue 5, pp. 1047-1054.e1). Elsevier Inc. https://doi.org/10.1016/j.jpainsymman.2020.06.026
4. Cancer Institute, N. (2017). Common Terminology Criteria for Adverse Events (CTCAE) Common Terminology Criteria for Adverse Events (CTCAE) v5.0. https://www.meddra.org/
5. Colvin, L. A. (2019a). Chemotherapy-induced peripheral neuropathy: Where are we now? In Pain (Vol. 160, Issue 1, pp. S1–S10). Lippincott Williams and Wilkins. https://doi.org/10.1097/j.pain.0000000000001540
6. Colvin, L. A. (2019b). Chemotherapy-induced peripheral neuropathy: Where are we now? In Pain (Vol. 160, Issue 1, pp. S1–S10). Lippincott Williams and Wilkins. https://doi.org/10.1097/j.pain.0000000000001540
7. CRUCIANI. (n.d.).
8. Desforges, A. D., Hebert, C. M., Spence, A. L., Reid, B., Dhaibar, H. A., Cruz-Topete, D., Cornett, E. M., Kaye, A. D., Urits, I., & Viswanath, O. (2022). Treatment and diagnosis of chemotherapy-induced peripheral neuropathy: An update. In Biomedicine and Pharmacotherapy (Vol. 147). Elsevier Masson s.r.l. https://doi.org/10.1016/j.biopha.2022.112671
9. Durand, M., & Mach, N. (2013). Alpha lipoic acid and its antioxidant against cancer and diseases of central sensitization. In Nutricion Hospitalaria (Vol. 28, Issue 4, pp. 1031–1038). Grupo Aula Medica S.A. https://doi.org/10.3305/nh.2013.28.4.6589
10. Gordon-Williams, R., & Farquhar-Smith, P. (2020). Recent advances in understanding chemotherapy-induced peripheral neuropathy. F1000Research, 9. https://doi.org/10.12688/f1000research.21625.1
11. Guo, Y., Jones, D., Palmer, J. L., Forman, A., Dakhil, S. R., Velasco, M. R., Weiss, M., Gilman, P., Mills, G. M., Noga, S. J., Eng, C., Overman, M. J., & Fisch, M. J. (2014). Oral alpha-lipoic acid to prevent chemotherapy-induced peripheral neuropathy: A randomized, double-blind, placebo-controlled trial. Supportive Care in Cancer, 22(5), 1223–1231. https://doi.org/10.1007/s00520-013-2075-1
12. Hershman, D. L., Lacchetti, C., Dworkin, R. H., Lavoie Smith, E. M., Bleeker, J., Cavaletti, G., Chauhan, C., Gavin, P., Lavino, A., Lustberg, M. B., Paice, J., Schneider, B., Smith, M. lou, Smith, T., Terstriep, S., Wagner-Johnston, N., Bak, K., & Loprinzi, C. L. (2014). Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: American society of clinical oncology clinical practice guideline. In Journal of Clinical Oncology (Vol. 32, Issue 18, pp. 1941–1967). American Society of Clinical Oncology. https://doi.org/10.1200/JCO.2013.54.0914
13. Jordan, B., Margulies, A., Cardoso, F., Cavaletti, G., Haugnes, H. S., Jahn, P., & le Rhun, E. (2020). Systemic anticancer therapy-induced peripheral and central neurotoxicity: ESMOeEONSeEANO Clinical Practice Guidelines for diagnosis, prevention, treatment and follow-up 5 behalf of the ESMO Guidelines Committee *, the EONS Education Working Group * and the EANO Guideline Committee. 10(9). https://doi.org/10.1016/j
14. Kerckhove, N., Collin, A., Condé, S., Chaleteix, C., Pezet, D., & Balayssac, D. (2017). Long-term effects, pathophysiological mechanisms, and risk factors of chemotherapy-induced peripheral neuropathies: A comprehensive literature review. In Frontiers in Pharmacology (Vol. 8, Issue FEB). Frontiers Media S.A. https://doi.org/10.3389/fphar.2017.00086
15. Lavoie Smith, E. M., Pang, H., Cirrincione, C., Fleishman, S., Paskett, E. D., Ahles, T., Bressler, L. R., Fadul, C. E., Knox, C., Le-Lindqwister, N., Gilman, P. B., & Shapiro, C. L. (n.d.). Effect of Duloxetine on Pain, Function, and Quality of Life Among Patients With Chemotherapy-Induced Painful Peripheral Neuropathy A Randomized Clinical Trial. www.jama.com.
16. Ledeboer, A., Jekich, B. M., Sloane, E. M., Mahoney, J. H., Langer, S. J., Milligan, E. D., Martin, D., Maier, S. F., Johnson, K. W., Leinwand, L. A., Chavez, R. A., & Watkins, L. R. (2007). Intrathecal Interleukin-10 Gene Therapy Attenuates Paclitaxel-Induced Mechanical Allodynia and Proinflammatory Cytokine Expression in Dorsal Root Ganglia in Rats. In Brain Behav Immun (Vol. 21, Issue 5).
17. Loprinzi, C. L., Lacchetti, C., Bleeker, J., Cavaletti, G., Chauhan, C., Hertz, D. L., Kelley, M. R., Lavino, A., Pharm, B., Lustberg, M. B., Paice, J. A., Schneider, B. P., Lavoie Smith, E. M., lou Smith, M., Smith, T. J., Wagner-Johnston, N., & Hershman, D. L. (2020). Prevention and Management of Chemotherapy-Induced Peripheral Neuropathy in Survivors of Adult Cancers: ASCO Guideline Update. In J Clin Oncol (Vol. 38). www.cancer.net
18. Maihöfner, C., Diel, I., Tesch, H., Quandel, T., & Baron, R. (n.d.). Chemotherapy-induced peripheral neuropathy (CIPN): current therapies and topical treatment option with high-concentration capsaicin. https://doi.org/10.1007/s00520-021-06042-x/Published
19. Mao, J., & Chen, L. L. (n.d.). Systemic lidocaine for neuropathic pain relief. www.elsevier.nl/locate/pain
20. Mols, F., Beijers, T., Vreugdenhil, G., & van de Poll-Franse, L. (2014). Chemotherapy-induced peripheral neuropathy and its association with quality of life: A systematic review. In Supportive Care in Cancer (Vol. 22, Issue 8, pp. 2261–2269). Springer Verlag. https://doi.org/10.1007/s00520-014-2255-7
21. Spallone, V., Morganti, R., D’Amato, C., Greco, C., Cacciotti, L., & Marfia, G. A. (2012). Validation of DN4 as a screening tool for neuropathic pain in painful diabetic polyneuropathy. Diabetic Medicine, 29(5), 578–585. https://doi.org/10.1111/j.1464-5491.2011.03500.x
22. Vidal, M. A., Calderón, E., Román, D., Pérez-Bustamante, F., & Torres, L. M. (2004). Capsaicina tópica en el tratamiento del dolor neuropático.

Figure 1
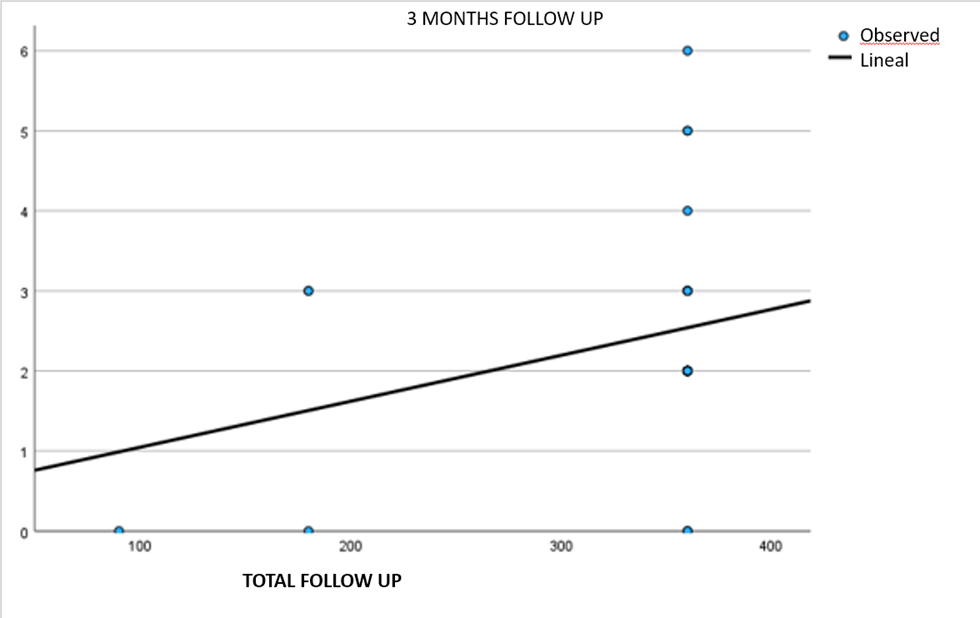
Figure 2
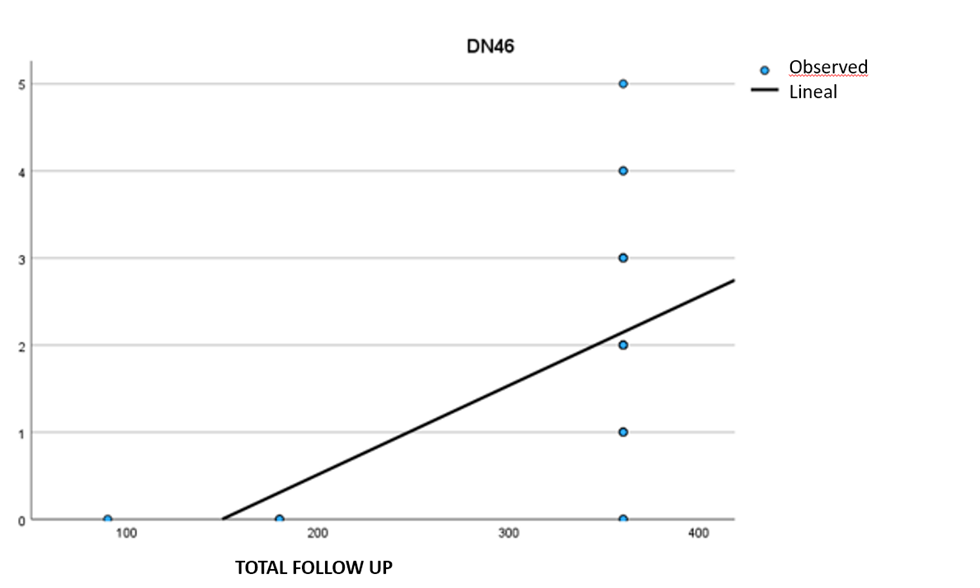
Figure 3

Figure 4

Figure 5

Figure 6

Figure 7

Figure 8
