A Case Report on Non-Hodgkin Lymphoma with Spleenomegaly and Pancytopenia: Challenges in Management and Role of Emergency Splenectomy
A Case Report on Non-Hodgkin Lymphoma with Spleenomegaly and Pancytopenia: Challenges in Management and Role of Emergency Splenectomy
Dr.Divyesh.Pathak1, Dr.Niraj.Bhatt2, Dr.Tejas.Pandya3*, Dr.Priyansh.Jain4, Dr.Chinmay.Prajapati5
1, 4. Surgical oncologist ;Dept of surgical oncology; Shri J.B.Mody Cancer Centre, Ankleshwar
2. Medical oncologist Dept of medical oncology; Shri J.B.Mody Cancer Centre, Ankleshwar
3, 5. Radiation oncologist Dept of radiation oncology; Shri J.B.Mody Cancer Centre, Ankleshwar
*Correspondence to: Dr Tejas.Pandya, Radiation oncologist; Dept of Radiation oncology; Shri J.B.Mody Cancer Centre, Ankleshwar.
Copyright.
© 2025 Dr Tejas.Pandya This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 06 February 2025
Published: 19 February 2025
DOI: https://doi.org/10.5281/zenodo.14903678
Abstract
The 47-year-old female presented with progressive left-sided abdominal fullness, splenomegaly, and pancytopenia, and was diagnosed with Splenic Marginal Zone Lymphoma (SMZL) through histopathological findings of lymphoid cell infiltration in the spleen and hilar lymph nodes, supported by positive immunohistochemistry and flow cytometry. Despite initial treatment with six doses of Rituximab monotherapy, the patient did not respond, prompting a timely shift to a more systemic management approach with the R-CVP regimen, tailored to her age and thrombocytopenia. When symptoms persisted, an emergency splenectomy was skillfully performed to provide symptomatic relief and enhance survival, with surgical risks meticulously managed.This timely and decisive intervention proved crucial, and the patient has since shown remarkable improvement. At her follow-up visit post-surgery, she is tolerating treatment well and is in good health, demonstrating the success of the comprehensive and adaptive care provided.
A Case Report on Non-Hodgkin Lymphoma with Spleenomegaly and Pancytopenia: Challenges in Management and Role of Emergency Splenectomy
Introduction
Splenic marginal zone lymphoma (SMZL) is a rare indolent B-cell non-Hodgkin lymphoma, comprising less than 2% of all lymphomas. It originates in the marginal zone of the spleen and often involves bone marrow and peripheral blood. SMZL predominantly affects older adults, typically presenting with splenomegaly and varying degrees of cytopenias, including pancytopenia—a result of hypersplenism, bone marrow infiltration, or both [1]
The pathogenesis of SMZL is linked to recurrent mutations, including NOTCH2, KLF2, and TP53, disrupting key signaling pathways. Chronic antigen stimulation, such as hepatitis C virus (HCV) infection, suggests a possible antigen-driven mechanism in some cases [2]. Immunophenotypically, SMZL cells express CD19, CD20, and CD79a, with absence of CD5, CD10, and CD23, aiding differentiation from other lymphomas [3]Treatment is symptom- and burden-dependent. Asymptomatic cases may be monitored without intervention, while symptomatic SMZL warrants therapy. Rituximab, a CD20 monoclonal antibody, is the cornerstone of treatment, either as monotherapy or combined with chemotherapy in advanced disease [2].
Table 1: showing the changes in pancytopenia indicating parameters
|
Parameter Reading(reveling Pancytopenia )from presentation to the therapy |
||||||||||||||
|
Events |
1st R-cycle |
2nd R-cycle |
3rd R-cycle |
4th R-cycle |
5th R-cycle |
6th R-cycle |
post 6th R-cycle |
1st R-CVP Cycle |
2nd R-CVP Cycle |
3rd R-CVP Cycle |
4th R-CVP Cycle |
5th R-CVP Cycle |
6th R-CVP Cycle |
|
|
Hb (g%) |
9 |
10.1 |
11.5 |
9.4 |
9.6 |
10.5 |
9.5 |
8.9 |
9.7 |
9.6 |
9.2 |
10.6 |
8.6 |
|
|
Platelets/ul |
43000 |
61000 |
63000 |
76000 |
63000 |
81000 |
71000 |
70000 |
97000 |
103000 |
84000 |
98000 |
66000 |
|
|
WBC/ uL |
2470 |
2980 |
5160 |
2970 |
2760 |
3720 |
1980 |
1920 |
2010 |
1740 |
1790 |
2730 |
1200 |
|
|
Neutro% |
23 |
36 |
60 |
44 |
46 |
52 |
49 |
41 |
53 |
51 |
54 |
73 |
51 |
|
|
Lympho% |
73 |
59 |
35 |
50 |
48 |
43 |
40 |
54 |
42 |
44 |
39 |
23 |
43 |
|
|
Eosino% |
1 |
1 |
1 |
1 |
1 |
1 |
1 |
0 |
1 |
1 |
2 |
1 |
1 |
|
|
Mono% |
3 |
4 |
4 |
5 |
5 |
4 |
5 |
5 |
4 |
4 |
5 |
3 |
5 |
|
Case Report
A 47 year old presented in OPD with complaints of abdominal pain and discomfort slowlyprogressiveleft- sided abdominal fullnesssince a year now. Patient admitted with the history of blood transfusion 1 year ago .There was no history of fever, weight loss, night sweats, vomiting, gastrointestinal or muco-cutaneous bleeding, or recurrent infections. The patient has no history of co morbid conditions, jaundice, or tuberculosis. She denies any history of smoking or alcohol use, although she reports a previous tobacco addiction, which she ceased one year ago. She was afebrile and physical examination revealed no palpable peripheral lymphadenopathy.
Patient had Past surgical history of Tubal ligation 15 years ago. She is currently in menopause, reports of last menses 15-05-2023 . The patient exhibited a distended abdomen with a firm, palpable spleen extending below the umbilicus. Head and neck examination revealed moderate anemia, no jaundice and a clear oropharynx. Completehaemogramrevealed pancytopenia (hemoglobin9.1g/dl, platelet count 43000,and total leukocyte count 2470, with 23% neutrophils, 73% lymphocytes, 03% monocytes and 1% eosinophils). Reticulocyte count was 2.5%. Peripheral smear showed microcytichypochromic redbloodcells and no abnormal lymphoid cells were seen.
Fig 1: showing evident of gross splenomegaly
Direct Coombs test was done to rule out auto-immune hemolyticanemia’s and it was negative. LDH was found to be slightly increased 468 IU/L(225 - 450IU/L ).Coagulationprofile(APTT,PT,thrombintime, fibrinogen level), hemoglobin HPLC, renal and liver function tests, electrolytes and serum LDH level were normal.HBsAgwas negativeandanti-HIVandanti-HCVwerenon-reactive.There was no ascites or hepatomegaly. 2D-ECHO examination shows Heart to be normal and lung examination- PA Chest scan were also normal. Abdominal ultrasonography and plain computed tomography scanning evident of gross splenomegaly with absence a mass lesion (Fig.1 )that later progresses to few nodular lesions in splenic hilum without any feature of portalhypertension or any abnormal lesions in other organs at the time of CT examination. Liver and renal functions were within normal limits. Liver cirrhosis and idiopathic portal hypertension were ruled out.
To investigate provisional diagnosis of Splenicnon-Hodgkin lymphoma, patient underwent splenic biopsy for histopathological examination. The splenic biopsy exanimation results showed the spleenic measure 37x18x10 cm weighing more than 1 kg with surface appearing reddish.
Multiple lymph nodes were identified, largest measuring 4.0 cm. The Lymph nodes dissected from hilum (04/04) show effacement of the architecture & its involvement by neoplastic lymphoid cells. Lymphoid cells encroach the nodule of pancreatic parenchyma at the hilum. Hilar vessels (margin) are free of infiltration, supporting the prognosis by indication lymphoproliferative disease involving the spleen and hilar lymph nodes. In view of presence of villous lymphocytes with clinically splenomegaly and flow cytometry findings Marginal Zone Lymphoma is most likely.
A working diagnosis of NHL with a differential of SMZL lymphoma was made. Immunohistochemistry(IHC) was done to confirm further,suggested a non-Hodgkin lymphoma with positive CD19, CD20, Kappa, CD11c, and CD180 tumor cells. The overall features were consistent with diagnosis of SMZL Therefore, the patient was diagnosed as Splenic marginal zone lymphoma (SMZL). As per NCCN guideline the patient was treated with CD20-targeting mAbs (also called anti-CD20 mAbs) Rituximab single regimen to work against the protein CD20 found on the surface of B cells and MZL. The drug attaches to the CD20 protein causing direct cell death. It also alerts the immune system to the cancer. This triggers normal immune cells to kill the cancer cells.The patient initially received rituximab monotherapy, but due to lack of response, transitioned to R-CVP chemotherapy. However, the disease progressed, necessitating a splenectomy to remove a 4.585 kg(Fig.2) splenic tumor.
Fig 2: Spleen weighing 4.585Kg post- spleenectomy
This intervention aimed to alleviate symptoms and improve overall survival, while carefully managing associated risks.
Discussion
Splenic marginal zone lymphoma (SMZL) is a rare, indolent B-cell lymphoma, accounting for less than 1% of all non-Hodgkin lymphomas (NHLs) [4]. It typically presents with moderate to severe splenomegaly, and while bone marrow involvement is common, peripheral lymphadenopathy is uncommon [5]. The definitive diagnosis of SMZL is established through histological examination of the spleen tissue. SMZL accounts for approximately 8-14% of splenectomies performed for lymphoproliferative disorders [6]. The male-to-female ratio is 1:1.8, with a median age of diagnosis around 68 years (range, 22-79 years) [7]. In all cases, the spleen is affected, and while the splenic hilar lymph nodes are commonly involved, peripheral lymphadenopathy is typically absent. Non-Hodgkin lymphoma (NHL) involves the spleen in approximately 40% of cases [8]. The standard first-line treatment is the systemic chemotherapy regimen R-CHOP [10]. Splenectomy is frequently performed for splenic NHL due to its low morbidity and mortality risk, ability to prevent hematological complications, and 80-90% response rate, with a median survival of 93 months as per retrospective studies[8,9]. While splenectomy may delay the initiation of other treatments, it is associated with a 77% five-year survival rate [8].Currently, Rituximab monotherapy (375 mg/m² weekly for 4 doses) is the preferred first-line treatment for symptomatic patients, with splenectomy reserved for those who do not respond to Rituximab [4,10,11].
In alignment with NCCN guidelines, the patient was initially administered a single-agent regimen of rituximab monotherapy, utilizing a weekly dosage of 550 mg for a total of six doses. Upon assessment of the patient's response to this therapeutic approach, it was determined that the desired clinical outcome had not been achieved.
To address the evolving clinical scenario, a strategic shift to a more intensive systemic chemotherapy regimen was implemented. Consequently, the patient was administered six cycles of R-CVP chemotherapy, a regimen consisting of rituximab (550 mg), cyclophosphamide (600 mg), vincristine (1 mg), and prednisolone (20 mg). This therapeutic approach was selected in accordance with NCCN guidelines. Despite the implementation of this intensified treatment strategy, the patient's condition did not exhibit a favorable response and splenic tumor kept on increasing. As a result, an urgent intervention became imperative to manage the patient's deteriorating clinical status.Splenectomy to opt for significant symptomatic relief, high response rates, and can improve survival outcomes in selected patients. A splenectomy procedure was conducted on the patient, resulting in the excision of a substantial splenic tumor weighing 4.585 kilograms. Given the nature and extent of the disease, splenectomy was deemed the optimal therapeutic strategy at this stage.
Conclusion
This case highlights the rare presentation of marginal splenic involvement in B-cell lymphoma, characterized by progressive splenomegaly and cytopenias. Thanks to timely and proactive intervention, initial treatment with rituximab monotherapy transitioned to a more focused systemic management approach with R-CVP chemotherapy. Following an emergency splenectomy was performed, effectively alleviating symptoms and significantly enhancing the patient's prognosis. The patient has since recovered well and, at the follow-up visit post-surgery, is tolerating treatment excellently and is found to be in good health.
References
1. Matutes E, Parry-Jones N, Brito-Babapulle V, Wotherspoon A, Morilla R, Catovsky D. The pathology and clinical features of splenic marginal zone lymphoma. Br J Haematol. 2008; 144(1):29–36.British Journal of Haematology. Available at: Blood Journal by American Society of Hematology
2. Arcaini L, Rossi D, Paulli M. Splenic marginal zone lymphoma: From genetics to management. Blood. 2016;127(17):2072–81.Blood. 2016;127(17):2072–81. Further details are available at: Hematological.
3. Piris MA, Campo E, Swerdlow SH. Splenic B-cell marginal zone lymphoma. In: WHO Classification of Tumors of Hematopoietic and Lymphoid Tissues. Revised 4th ed. Lyon: IARC; 2017. Available at: latest WHO classification resources or visit Springer Link for related publications: Springer Link
4. National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology. B-Cell Lymphomas, Version 5.2019 – September 23, 2019. www. NCCN.org.
5. Jamal I, Nirala S, Tutor P. Splenic marginal zone lymphoma: A rare case report on splenic marginal zone lymphoma. IOSR-JDMS. 2016;15(9):38-40.
6. Mishra MN, Pandey R, Dinda A, Nityanand S. A peculiar case of splenic marginal zone lymphoma and review of literature. Iran J Immunol. 2013;10(3):186-89.
7. Franco V, Florena AM, Iannitto E. Splenic marginal zone lymphoma. Blood. 2003;101(7):2464-72.
8. Bairey O., Shvidel L., Perry C., Dann E.J., Ruchlemer R., Tadmor T. Characteristics of primary splenic diffuse large B-cell lymphoma and role of splenectomy in improving survival. Cancer. 2015;121:2909–2916. doi: 10.1002/cncr.29487. [DOI] [PubMed] [Google Scholar]
9. Milosevic R, Todorovich M, Balint B, Jevtic M, Krstic M, Ristanovic E, et al.Splenectomywithchaemotherapyvssurgeryaloneasinitialtreatmentofsplenicmarginalzonelymphoma.WorldJGastroenterol.2009;15(32):4009-15.
10. Saboo S.S., Krajewski K.M., Regan N.O. Spleen in haematological malignancies: spectrum of imaging findings. Br. J. Radiol. 2012;85:81–92. doi: 10.1259/bjr/31542964. [DOI] [PMC free article] [PubMed] [Google Scholar]
11. Else M, Marin-Niebla A, de la Cruz F, Batty P, Rios E, Dearden CE, et al. Rituximab,used aloneorincombination, is superior too ther treatment modalities in splenicmarginal zone lymphoma. Br J Haematol. 2012;159(3):322-28.
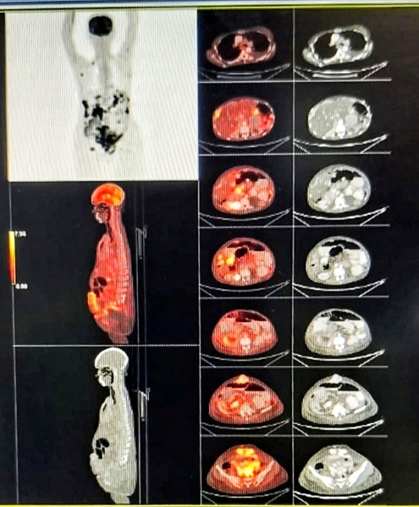
Figure 1

Figure 2
