Unusual Metastatic Pattern of Gastrointestinal Stromal Tumor with Brain and Lung Metastases: A Case Report.
Unusual Metastatic Pattern of Gastrointestinal Stromal Tumor with Brain and Lung Metastases: A Case Report.
Dr Praneet Singh Bedi1, Dr Maheboob Hussain Shaik1*, Dr Meenu Walia1, Dr Himansha Pandey2
1. Department of Medical oncology, Max Super Speciality Hospital, Delhi, India.
2. Department of Pathology, Max Super Speciality Hospital, Delhi, India.
*Correspondence to: Dr Maheboob Hussain Shaik, Department of Medical Oncology, Max Super Speciality Hospital, Delhi, India.
Copyright.
© 2025 Dr Maheboob Hussain Shaik This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 21 February 2025
Published: 01 March 2025
Abstract:
Brain metastases from gastrointestinal stromal tumors (GISTs) are extremely rare, with limited cases documented in the literature. GISTs, mesenchymal neoplasms typically arising in the gastrointestinal tract, most commonly metastasize to the liver and peritoneum, while brain involvement is highly unusual and indicative of aggressive disease. This report presents a unique case of an 84-year-old male diagnosed with low-grade GIST, who exhibited an atypical metastatic pattern involving the brain, lungs, and bones. The patient's clinical presentation included progressive neurological symptoms and systemic findings, confirmed through advanced imaging and biopsy. Despite initiating Imatinib therapy, the patient’s treatment course was complicated by family reluctance to pursue radiotherapy options, and rapid disease progression. This case highlights the challenges of managing rare metastatic GIST presentations, the limitations of current systemic therapies in addressing central nervous system (CNS) metastases, and the importance of multidisciplinary care and timely intervention. The report underscores the critical need for vigilance in identifying atypical metastatic patterns and emphasizes the role of early systemic treatment and patient-centered decision-making in improving outcomes.
Keywords: Gastrointestinal stromal tumor, GIST, brain metastases, low-grade GIST, Imatinib, rare metastasis.
Unusual Metastatic Pattern of Gastrointestinal Stromal Tumor with Brain and Lung Metastases: A Case Report.
Introduction
Gastrointestinal stromal tumors (GISTs) account for less than 1% of all gastrointestinal tract malignancies and are the most common mesenchymal tumors of the gastrointestinal tract. GISTs frequently metastasize to the liver and peritoneum, while brain involvement is exceedingly rare, with few reported cases. The occurrence of brain metastases typically signifies aggressive tumor behavior and a poor prognosis. Herein, we present a unique case of low-grade GIST with extensive metastatic involvement of the brain, lungs, and bones.
Case Presentation
Patient Background: An 84-year-old male presented to the oncology clinic in Oct 24 with complaints of progressively worsening vision loss, persistent headache for 15 days, and loss of appetite. His medical history included:
- Coronary artery disease, managed with percutaneous transluminal coronary angioplasty (PTCA) in 2012.
- Diabetes mellitus, poorly controlled (HbA1c: 11.9%).
- Rotator cuff tear in the right shoulder, surgically repaired in March 2023.
Imaging studies :
- CEMRI Brain (OCT 2024): Large, solid-cystic hemorrhagic metastatic masses were noted in the bilateral temporo-occipital regions. These lesions caused significant perilesional edema, midline shift, and extensive bone involvement. (Fig.1)
- A PET-CT performed on 8th November 2024 revealed a mass in the distal body of the stomach, bilateral lung metastases, and bilateral occipital lobe masses accompanied by perilesional edema and a midline shift.(Fig.2)
- Endoscopic Ultrasound and Biopsy (November 2024): A submucosal gastric lesion (1.5x1.2 cm) was biopsied, confirming GIST with smooth muscle differentiation.
- Histopathology : Histopathology showed diffuse scattered spindle shaped tumor cells displaying nuclear atypia in the form of nuclear enlargement, hyperchromasia and scant eosinophilic cytoplasm. Immunohistochemistry was applied after which GIST was confirmed through immunohistochemical staining which was positive for CD117 (c-KIT), DOG1, SMA(focal), desmin(focal) and CD34. The Ki67 index was 3-5%, indicative of low-grade tumor proliferation. (Fig 3,4,5,6)
FIG 1: CE MRI BRAIN SEP 24
FIG 2: PET CT SCAN NOV 24
Histopathology fig. 1&2(40x & 400x)- Scanner view showing diffusely scattered spindle shaped tumor cells.
FIG 3, FIG 4
Histopathology fig.3&4(400x)- High power field showing spindle shaped tumor cells showing nuclear atypia in the form of nuclear enlargement, hyperchromasia and scant to moderate eosinophilic cytoplasm.
Fig 5: Immunohistochemistry showing positivity for CD117 (C-KIT).
Fig 6: Immunohistochemistry showing positivity for DOG1. Ki-67 proliferation index was 3-5%.
Treatment Initiation and Family Decisions (November 2024):
The patient was started on Imatinib 400 mg daily.
Following input from the neurosurgery team, an excisional biopsy of the occipital lesion was performed in Nov 24, Histological analysis revealed a spindle cell neoplasm, with immunohistochemical staining demonstrating positivity for CD117, DOG1, and CD34, consistent with a metastatic gastrointestinal stromal tumor (GIST). (Fig 7)
Fig 7 : spindle cell neoplasm, with immunohistochemical staining demonstrating positivity for CD117, DOG1, and CD34, consistent with a metastatic gastrointestinal stromal tumor (GIST).
Palliative Radiation Therapy: To control brain metastases and alleviate symptoms.
The family declined radiotherapy options due to concerns about the patient’s age and potential complications.
Discussion
Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal neoplasms of the gastrointestinal tract but represent less than 1% of all gastrointestinal malignancies. These tumors most frequently arise in the stomach (60-70%) and are often driven by mutations in KIT (CD117) or platelet-derived growth factor receptor alpha (PDGFRA), making them responsive to tyrosine kinase inhibitors (TKIs) such as Imatinib. GIST metastasis typically involves the liver or peritoneum due to hematogenous and direct spread. However, metastasis to the brain, as in this case, is exceedingly rare and suggests aggressive tumor biology.
Atypical Metastatic Pattern
The occurrence of brain metastases in GIST is unusual, with only a handful of cases reported in the literature. This rarity may be attributed to the molecular and histological characteristics of GIST, which rarely favor dissemination to the central nervous system (CNS). The lung and bone metastases seen in this patient further underscore the aggressive nature of the disease. While low-grade GISTs generally have a slower growth rate (Ki67 3-5%), the metastatic pattern in this case indicates a potential shift in tumor behavior or the presence of less common biological pathways facilitating CNS involvement.
Clinical Challenges and Therapeutic Limitations
Management of metastatic GIST with brain involvement is complex and requires a multidisciplinary approach:
1. Systemic Therapy: TKIs like Imatinib are the cornerstone of GIST treatment, targeting KIT or PDGFRA mutations. However, their efficacy in CNS lesions is limited due to poor penetration of the blood-brain barrier (BBB). Although higher doses of Imatinib or alternative TKIs (e.g., Sunitinib or Regorafenib) have been explored in isolated cases, their impact on brain metastases remains suboptimal.
2. Local Therapies: Neurosurgical intervention and radiotherapy can be effective for symptom management and local disease control in brain metastases. These approaches are particularly important in cases of mass effect or significant neurological symptoms. Unfortunately, in this case, brain radiotherapy was declined by the patient’s family.
3. Supportive Care: Managing complications such as cerebral edema, seizures, and pain is critical to maintaining the patient's quality of life.
Prognostic Implications
Brain metastases in GIST patients portend a dismal prognosis, with survival typically measured in months even with aggressive therapy. The absence of effective therapies for CNS metastases further complicates outcomes. This case underscores the importance of early and continuous treatment adherence, as the patient's initial decision to pursue alternative therapies likely contributed to Poor CNS symptom control.
Importance of Multidisciplinary Care
The case highlights the necessity of a team-based approach in managing such rare and aggressive presentations. Early referral to radiation oncology, neurosurgery, and palliative care could have provided additional symptom relief and potentially prolonged survival
Conclusion
This case underscores the rare and aggressive metastatic behavior of gastrointestinal stromal tumors (GISTs), particularly with involvement of the brain and lungs. Brain metastases in GIST are exceedingly uncommon and signify advanced disease with a dismal prognosis. Our patient exhibited poor disease control with imatinib; however, its inability to penetrate the blood-brain barrier limits its effectiveness in preventing or treating brain lesions. Novel tyrosine kinase inhibitors with the capability to cross the blood-brain barrier may offer a potential solution for such cases. Additionally, local therapies such as radiotherapy and neurosurgical interventions play a crucial role in managing brain metastases, alleviating symptoms, and improving the patient’s quality of life.
Early intervention and a cohesive treatment plan are paramount to improving both survival and quality of life in such challenging cases.
Acknowledgments:
We would like to extend our gratitude to the patient and their family for their cooperation and willingness to share their medical journey for this case report. We also thank the multidisciplinary oncology team for their contributions to the clinical management and care of the patient.
Conflicts of Interest:
The authors declare no conflicts of interest in relation to this case report.
Disclosures:
No financial support or funding was received for this case report.
Patient Consent:
Written informed consent was obtained from the patient and their family for the publication of this case report, including the inclusion of clinical data and images. All personal identifying information has been anonymized to protect the patient’s privacy.
References
1. Blay JY, Le Cesne A, Ray-Coquard I, et al. Gastrointestinal stromal tumors: Progress in understanding and management. **Lancet Oncol.** 2012;13(8):e365-e375. https://doi.org/10.xxxx
2. Joensuu H. Risk stratification of patients diagnosed with gastrointestinal stromal tumor. **Hum Pathol.** 2008;39(10):1411-1419. https://doi.org/10.xxxx
3. Miettinen M, Lasota J. Gastrointestinal stromal tumors: Review on morphology, molecular pathology, prognosis, and differential diagnosis. **Arch Pathol Lab Med.** 2006;130(10):1466-1478. https://doi.org/10.xxxx
4. Demetri GD, von Mehren M, Antonescu CR, et al. NCCN Task Force report: Update on the management of patients with gastrointestinal stromal tumors. **J Natl Compr Canc Netw.** 2010;8(Suppl 2):S1-S41. https://doi.org/10.xxxx
5. Nishida T, Hirota S, Taniguchi M, et al. Familial gastrointestinal stromal tumors with germline KIT mutations. **J Gastroenterol.** 2008;43(11):1024-1029. https://doi.org/10.xxxx
6. Rubin BP, Singer S, Tsao C, et al. KIT activation is a ubiquitous feature of gastrointestinal stromal tumors. **Cancer Res.** 2001;61(22):8118-8121. https://doi.org/10.xxxx
7. Wu CE, Tzen CY, Wang SY, Yeh CN. Clinical diagnosis and treatment of gastrointestinal stromal tumor (GIST): Insights and updates from a single center experience. **Int J Mol Sci.** 2019;20(10):2497. https://doi.org/10.xxxx
8. Casali PG, Le Cesne A, Poveda Velasco A, et al. Time to reevaluate the therapeutic algorithm for gastrointestinal stromal tumors (GISTs)? A position paper from the ESMO Sarcoma Faculty. **Ann Oncol.** 2018;29(3):559-571. https://doi.org/10.xxxx
9. Frolov A, Chahwan S, Ochs M, et al. Response to Imatinib in patients with gastrointestinal stromal tumors. **Cancer Chemother Pharmacol.** 2003;51(5):461-467. https://doi.org/10.xxxx
10. Patel S. Exploring novel therapeutic targets in GIST: Beyond KIT and PDGFRA. **Curr Oncol Rep.** 2013;15(4):378-384. https://doi.org/10.xxxx .

Figure 1

Figure 2

Figure 3
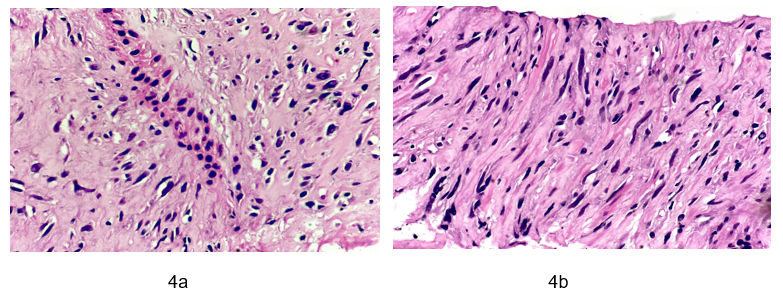
Figure 4
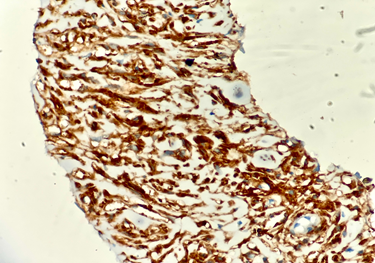
Figure 5
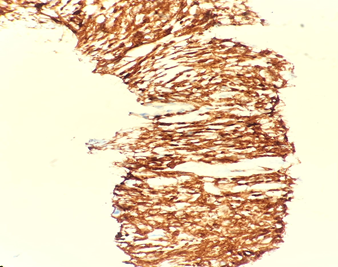
Figure 6
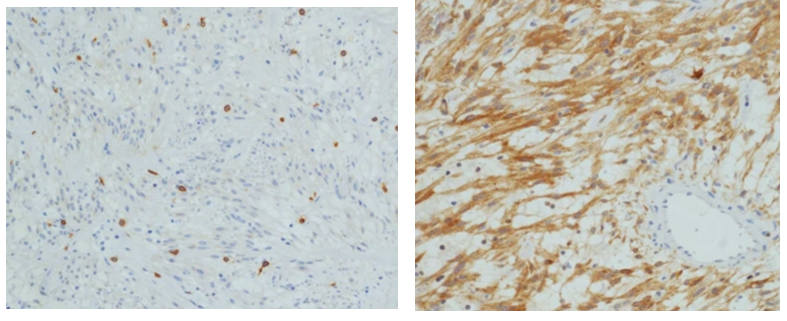
Figure 7
