Diagnostic and Therapeutic Alternatives for Genu Varum in Children
Diagnostic and Therapeutic Alternatives for Genu Varum in Children
Kassem El Houcheimi*
*Correspondence to: Kassem El Houcheimi, United Arab Emirates.
Copyright
© 2024: Kassem El Houcheimi. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 03 March 2024
Published: 20 March 2024
Abstract
Genu valgum is a common orthopedic problem in children. Most conditions are physical changes that can be reduced naturally. However, pathological diseases occur due to local processes and processes in the body, which are often ineffective and often require treatment. A good understanding of the history of tibiofemoral development in children can help distinguish between these two types. In this review, methods for evaluating and diagnosing genu valgum are presented and treatment options are discussed.
Diagnostic and Therapeutic Alternatives for Genu Varum in Children
Introduction
Knee valgus, or varus knee, is a condition that affects the lower legs of children and adolescents and often requires evaluation by an orthopedic surgeon. The physiological form, as in knee varus, is the most common. However, pathological conditions exist, appear to progress, and may require treatment (Table 1). Obviously it is very important to distinguish between these places. In this review, we will document methods for the evaluation, diagnosis and treatment of genu valgus in children.
Physiologic Genu Valgum
Angular misalignment is easy to assess if you are familiar with the development of the tibiofemoral angle. Salenius and Vankka [1] showed in a radiographic study that the tibiofemoral angle in children is characterized by maximum flexion (genu varum angle 10 to 15 degrees). It improves between 20 and 22 months and increases to the highest valgus angle (10 to 15 degrees) from 3 years of age. Physiological knee valgus (7 to 8 degrees) in normal children gradually resolved over the next few years (Figure 1). Staheli et al [2,3] reported a similar growth pattern using clinical assessment techniques. In most children with genu valgum, the tibiofemoral angle is two standard deviations above or below the mean. They can be treated by observing the parents and confirming that the "deformity" is a normal change and not a disease. Torsional misalignment can have similar effects. Children with excessive femoral anteversion and compensatory lateral tibial torsion may have a valgus knee deformity without frontal plane deformity. In this case, knee valgus occurs depending on the negative rotation plane.
Pathologic Genu Valgum
Pathological genu valgum is less than normal genu valgum. But there are many reasons for this. Both the region and the system in the body can cause deformities in all bones, in a specific area or more of the bones. By definition, children with pathological genu valgum have tibiofemoral angles greater than two standard deviations Fig 01. The deformity is usually unilateral and usually requires correction.
Fig. 1 Graph illustrating the development of the tibiofemoral angle in children during growth, based on measurements from 1,480 examinations of 979 children. Of the lighter lines, the middle one represents the mean value at a given point in time, and the other two represent the deviation from the mean. The darker line represents the general trend. (Adapted with permission from Salenius P, Vankka E: The development of the tibiofemoral angle in children. J Bone Joint Surg Am 1975;57:259-261.)
Table 1 Classification of Genu Valgum
Physiologic
- Knock-knees
- Apparent genu valgum (fat thighs, rotational deformity)
Pathologic
- Idiopathic
- Unresolved physiologic valgus Lateral femoral hypoplasia
Posttraumatic
- Malunion
- Physeal arrest
- Metaphyseal tibial fracture
Metabolic
- Rickets
- Renal osteodystrophy
Neuromuscular
- Cerebral palsy
- Paralytic conditions (e.g., poliomyelitis)
Infectious (e.g., osteomyelitis) Generalized disorders
- Juvenile arthritis
- Osteochondrodysplasia
- Osteogenesis imperfecta
Idiopathic
Idiopathic genu valgus occurs when anatomical changes cannot be resolved, resulting in high or negative risk. Children with this diagnosis are often obese and have flat feet characterized by loose ligaments. (Fig. 2).
Fig. 2 Idiopathic genu valgum in an obese teenager in whom physiologic valgus failed to resolve. Note the asymmetric involvement (greater on the left) and the hypoplasia of the lateral femoral condyle, suggesting excessive lateral loading.
Posttraumatic
Trauma is probably the most common cause of pathological genu valgum. Damage to the proximal femur or tibia can cause valgus deformity due to reduction or epiphyseal damage and subsequent growth arrest. Salter Harris type III, IV and V fractures in the proximal tibia, as in other parts of the immature bone, are the most dangerous for this. In contrast, some authors have shown that fracture pattern in the distal femur does not predict future developmental problems. . Additionally, the geometry of this epiphysis may affect the ability to achieve adequate anatomical reduction. It is worth noting that hidden epiphyseal injury of the knee may be accompanied by more pronounced fractures in the metaphyseal and diaphyseal region of the tibia and femur, leading to the development of angular deformity. Family members help. Hresko and Kasser6 recommend that all patients with lower extremity injuries receive a comprehensive evaluation as well as a knee electrocardiogram. Another cause of knee valgus is tibial valgus that occurs after proximal tibial metaphyseal fracture (Figure 3). Many reports on this problem have been published since Cozen7 first described it in 1953. The exact cause of the abnormality is still unknown, but several theories have been proposed. Cozen believes that this problem is caused by asymmetric stimulation of the proximal tibial epiphyseal plate. Salter and Best10 consider malunion to be the most important factor in the pathogenesis of valgus angulation. Houghton and Rooker11 attempted to cause tibial valgus in rabbits by dividing the anserine and medial periosteum and assumed the binding effect of the negative lateral periosteum as the mechanism. Weber12 surgeon investigated two cases of posterior valgus and found that the foot of the anserine was impinged on the fractured bone and thought that the medial tissue was the cause of the deformity. Recently, Jordan et al.13 reported 7 patients with this deformity, reviewed the main theories regarding the etiology of this problem, and concluded that the most important mechanism was itching in the middle of the tibia due to bone hyperemia. This is a common assumption and is supported by the results of two cases. Green14 reported a case of post-traumatic tibial valgus in which the presence of an asymmetric growth arrest line supported a mechanism for medial proximal tibial overgrowth. Zionts et al.15 reported a case of tibial valgus in which bone scan showed strong radionuclide in the medial 

half of the proximal tibial growth plate.
Fig. 3 Serial radiographs showing genu valgum due to inadequate initial reduction of a proximal metaphyseal tibial fracture in a 7-year-old child. A, Inadequate reduction. B, Malunion at the time of cast removal. C, Resultant valgus at 1-year follow-up.
Metabolic
Metabolic causes of pathological genu valgum include various types of rickets and renal osteodystrophy. Although these diseases have similar metabolic effects on the body, vitamin D-resistant rickets and vitamin D-deficient rickets are often associated with varus deformity of the knee, whereas renal osteodystrophy is often associated with valgus deformity. It is thought to be related to the body's mechanical loading pattern, which is determined by the relationship between the knees as metabolic processes manifest themselves. Therefore, metabolic diseases are often detected when the child begins to wake up. At this age, physiological tibiofemoral alignment is prone to deterioration of varus alignment according to the Heuter-Volkman law, which states that epiphyseal growth is inversely proportional to the stress applied to its longitudinal axis. Renal osteodystrophy can cause genu valgum for similar reasons, as children are usually older when metabolic effects occur. Most tibiofemoral valgus alignments have already occurred, and the subsequent mechanical forces acting on the epiphyseal plate predispose to the development of valgus deformity (Figure 4). Oppenheim et al.18 described changes in the lateral tibia of the proximal tibia in children with renal osteodystrophy that are similar to the changes that occur in the proximal medial tibia in Blount disease.
Fig. 4 Clinical appearance (A) and standing anteroposterior radiograph (B) of a 12-yearold child with chronic renal failure. Note the distal femoral physeal irregularities. Genu valgum is the most common skeletal manifestation of renal osteodystrophy
Neuromuscular
Children with neuromuscular disorders may develop knee valgus. Ambulatory children with cerebral palsy and other neuromuscular diseases often have foot valgus and/or excessive tibial torsion, causing the foot to rotate outside the knee (Figure 5). Due to this defect, there is valgus and external rotation of the knee in ground reaction while standing. These abnormalities, along with growth and weight gain, can lead to the development of valgus deformity in the foot, ankle and knee joints. It is thought to be caused by iliotibial band contracture20 and the effect of abnormal deviation (valgus thrust) with Trendelenburg walking or other walking support.

Fig. 5 Ambulatory 11-year-old child with neuromuscular disorder. External rotation of the foot is due to pes valgus and external tibial torsion. As a consequence, the ground reaction force passes lateral to the normal weight-bearing line, potentiating deformity in the foot and ankle and creating a valgus moment at the knee, which in time can lead to progressive deformity there as well.
Infectious
Osteomyelitis can cause genu valgus directly by destroying the growth plate or indirectly by inducing reactive hyperemia and asymmetric growth stimulation. The latter is a reflection of the process by which genu valgus develops in children with arthritis, in which congestion resulting from chronic synovitis asymmetrically irritates the epiphyses around the knee.21
Generalized Disorders
Genu valgum also occurs in children with hereditary skeletal disorders, such as multiple epiphyseal dysplasia and pseudoachondroplasia, and in other generalized disorders characterized by severe osteopenia, such as osteogenesis imperfecta.
Evaluation
Evaluation of genu valgum should include a complete medical history, including reproductive history, complete developmental sequence, family history, and nutritional history. Parents' concerns often relate to beauty, insecurity, and future career opportunities. Children with physiological ectropion usually have a normal pregnancy and birth history and reach maturity at the appropriate time. However, family history may reveal that other siblings or family members have similar concerns and symptoms. Growth patterns and nutritional history are usually normal. Children with genu valgum often have a history of growth deformity and, depending on the cause, a history of trauma, illness, malnutrition, or disease in the body. The physical examination should include accurate measurement of the patient's height to determine percent growth. The location of the deformity should be noted and the severity of the angulation should be noted by goniometry of the tibiofemoral angle or by measuring the distance between the medial malleolus and the patient's back and knees as suggested by Howorth. 4 Heath and Staheli3 described a photographic technique using points between the waist, patella, and ankle to determine the knee angle, with the axis close to the tibiofemoral angle. The procedure is simple and repeatable, providing objective visual information about the deformity that other treatments cannot provide. Rotational motion (especially femoral anteversion and lateral tibial torsion) and ligament laxity should be evaluated because these conditions have the potential to increase the likelihood of misalignment. Ligamentous laxity is the medical definition of joint hyperextension. Assessment of rotation is best done when the patient is active, with the hips extended and the knees flexed. In this position, hip rotation and foot elevation angle can be easily measured as estimates of femoral anteversion and tibial torsion, respectively. Children with physiological genu valgum are usually under 7 years of age, have equal involvement of the lower back muscles, and have a normal posture. Tibiofemoral angle is less than 15 degrees and the distance to the ankle is less than 8 cm. In this case, additional examinations and radiography are usually not required. However, if there is suspicion of pathological genu valgum, radiological examination is required. Greene22 and Staheli23 recommend these if the deformity is severe or asymmetrical, other musculoskeletal abnormalities are present, height is less than the 25th percentile, or the family history is good. In general, radiographic evaluation should be performed in children who are short, have asymmetrical joints, or have a tibiofemoral angle greater than 15 to 20 degrees. Weight-bearing anteroposterior radiography of the lower extremity (including the hip, knee, and ankle) can evaluate alignment and evaluate bony or epiphyseal abnormalities. If deformity is suspected or surgery is considered, lateral radiographs are useful in assessing the sagittal plane. Tomography helps determine the presence of epiphyseal strips. In children with idiopathic genu valgum, flattening of the lateral femoral condyle may occur. Patients with post-traumatic genu valgus may present with poor healing and signs of epiphyseal asymmetry or growth arrest. Children with rickets or renal osteodystrophy may have large and irregular epiphyses, and the proximal part of the tibia may be altered. Osteopenia often occurs in children with genu valgus due to chronic medical conditions. People with osteochondrodystrophy may have epiphyseal or metaphyseal growth disorders and changes in ossification in various regions. These findings are usually identified on vertical radiographs and can be further characterized by focusing on various radiographic targets if necessary. In general, measurement of the tibiofemoral angle (anatomical axis) will reflect the degree of valgus deformity and can be used to monitor progress. However, as noted by Davids et al, 17 this angle primarily measures the relative position of the diaphyseal bone and may not reflect the location or severity of the deformity, especially when longer bones are more involved. Therefore, measuring the orientation of the hip, knee and ankle joints relative to the weight-bearing axis (correction axis alignment) is considered a better way of character deformity (Figure 6).17,22-24.
Fig. 6 A, Mechanical-axis and joint-orientation angles that define normal frontal plane alignment. A line drawn from the center of the femoral head to the center of the ankle defines the mechanical axis. The line normally passes 1 cm medial to the center of the knee. These relationships can be used to characterize the source and severity of valgus malalignment, as advocated by Paley et al.28 B, A mechanicalaxis line passing through the lateral half of the knee joint defines valgus malalignment. C, Valgus deformity in the tibia is characterized by a medial proximal tibial angle (MPTA) greater than 90 degrees. D, Valgus deformity in the femur is characterized by a lateral distal femoral angle (LDFA) less than 85 degrees. E, Combined deformity. (Parts B-E adapted with permission from Paley D, Herzenberg JE, Tetsworth K, et al: Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am 1994;25:428.)
Treatment
By definition, children with knee valgus do not need treatment. Stents are impractical, poorly tolerated, and completely unnecessary in benign natural history. Physical damage. Instead, the child should be evaluated in detail and the parents should be immediately informed about the child's diagnosis, that the "problem" needs to be solved, and that nonoperative treatment is not appropriate. Even with an excellent history, surgery may be performed in some cases of valgus knee. Children under the age of 10 with a tibiofemoral angle greater than 15 to 20 degrees and/or a height difference of more than 8 cm, 1-4,22,23 children with short stature or asymmetric involvement and children with asymmetric involvement 4 Progressive malformations Radiographic examination and clinical examination should be performed to determine activity. If the tibiofemoral angle continues to exceed 15 degrees after age 10 or the average heel distance exceeds 10 cm, self-treatment is unlikely and surgical treatment may be necessary. Mechanical axis alignment and dual orientation. Treatment of knee valgus can be achieved by partial epiphysiodesis, 25 hemi-epiphyseal anastomosis, 4,21,26,27 or osteotomy.
Partial Epiphysiodesis
Partial epiphysiodesis recommended by Bowen et al.25 is the simplest procedure. It can be done through a standard incision that exposes the growth plate or percutaneously under fluoroscopic guidance. However, the aim is to create a bridge over the epiphysis against the angle at which the deformity around the apex can be corrected. The prerequisite for repair is further growth of the contralateral epiphyseal plate. Therefore, the ability to predict growth and its impact on angular deformity is critical to success. Bowen et al25 developed a method to determine changes in angle along the growth line using the Green-Anderson growth curve to help determine the timing of surgery. They reported good results in 10 of 12 patients treated with partial epiphysodesis using this method of prediction.
Hemiepiphyseal Stapling
Partial epiphysiodesis is the best option when growth is predictable. However, the process is irreversible and poor timing of surgery will lead to under- or over-correction of the deformity in cases where growth may be atypical. Therefore, epiphyseal anastomosis may be a better option in cases where bone growth cannot be seen, such as renal osteodystrophy, rickets, and other metabolic diseases that cause skeletal deterioration. This process, first described by Blount and Clarke in 1949, aims to mechanize longitudinal growth by creating a scaffolding around the epiphysis. If overcorrection is present and nail strip formation does not occur and staples can be removed without causing a growth plate, the effects are theoretically reversed by removing the staples. Regrowth is often accompanied by the phenomenon of regrowth next to the previously stapled epiphyseal plate. Although this can be partially compensated for by premature closure of the ipsilateral epiphysis, if staple removal is necessary, overcorrection of approximately 5 degrees is recommended to achieve the desired results. Adolescents who have osteoporosis by age 11 and boys who have osteoporosis by age 12 are generally the best candidates for surgery. Epiphyseal anastomosis is not recommended for children under the age of 10 due to lack of developmental delay and concerns about premature closure of the epiphysis. It is one of the best surgical options under these conditions: Angular deformity is caused by chronic pain and the growth process of the limbs.
Osteotomy
Osteotomy is probably the most common treatment for angular deformity. Although osteotomies can be performed at any age, they are usually not performed until the patient is almost fully grown. As with other methods of treating valgus deformity, the goal of osteotomy is to restore the body's physiologic mechanical axis alignment. If the bony deformity is generalized, treatment may be performed at multiple sites in the leg, perhaps even at a single bone. In most cases, repair can be accomplished with a dome osteotomy, tapered osteotomy, closed wedge osteotomy, or open bone osteotomy. Accompanying sagittal and/or transverse deformities should be identified and treated. The details of revision osteotomy are beyond the scope of this discussion. The main idea is that the correction should be as close to the center of rotation of the deformity angle as possible, so as not to show changes in the bones. Osteotomy of the distal femur or proximal tibia at this level is generally not possible for inexperienced individuals. Therefore, osteotomy should be performed at different levels of deformity. Therefore, it is designed not only to adjust the angle, but also to pay for translation so that the legs can be adjusted correctly. Treatment after osteotomy should be continued with stable treatment supported by a cast or other fixation until complete healing is achieved. Alternatively, principles of interventional osteogenesis can be used to correct angular deformity. As noted by Steel et al, neurovascular complications after osteotomy may be more common than thought. These include compartment syndrome, ischemia due to traction or compression of the anterior tibial nerve, and neuropraxia due to traction of the peroneal nerve. When the deformity is specific, risk can be reduced by avoiding valgus-varus realignment, routine prophylactic anterior chamber fasciotomy, drainage of the surgical wound, and careful postoperative monitoring of neurovascular conditions.
Relative Merits of Surgical Procedures
Both epiphyseal anastomosis and partial epiphyseal fixation occur less frequently than osteotomy. In addition, since knee valgus deformity usually occurs in the paraepiphyseal region of the distal femur or proximal tibia, treatment is performed at the appropriate level according to the rotational position of the deformity and mechanical axis alignment is restored. Posttraumatic genu valgus after proximal tibial metaphyseal fracture usually heals spontaneously within 2 to 4 years29 and early osteotomy should be avoided. Surgical treatment is effective depending on the severity and shape of the deformity. Genu valgum, associated with long-term metabolic syndrome, is a complex deformity that often requires osteotomy. The patient's metabolic system must be stable as a prerequisite for surgical treatment. 16,17
Conclusion
Genu valgum is a common condition in children. Physiological differences predominate and do not require treatment. Pathological genu valgum is rare, usually complete, and usually requires treatment. In order to distinguish between these two types, it is necessary to understand the history of tibiofemoral angle development. Nonoperative treatment of knee valgus, whether physiological or pathological, is not appropriate. The former is unnecessary and the latter is useless. In children under 10 years of age, if the tibiofemoral angle is greater than 15 degrees or the distance to the ankle is greater than 10 centimeters, self-correction is unlikely and will most likely need to be treated surgically. The goal of treatment is to fully restore the mechanical axis, which can be achieved by epiphyseal anastomosis, partial epiphyseal fixation, or osteotomy, depending on the cause, location, and severity of the deformity.
References
1. Salenius P, Vankka E: The development of the tibiofemoral angle in children. J Bone Joint Surg Am 1975;57:259-261.
2. Engel GM, Staheli LT: The natural history of torsion and other factors influencing gait in childhood: A study of the angle of gait, tibial torsion, knee angle, hip rotation, and development of the arch in normal children. Clin Orthop 1974;99:12-17.
3. Heath CH, Staheli LT: Normal limits of knee angle in white children: Genu varum and genu valgum. J Pediatr Orthop 1993;13:259-262.
4. Howorth B: Knock knees: With special reference to the stapling operation. Clin Orthop 1971;77:233-246.
5. Riseborough EJ, Barrett IR, Shapiro F: Growth disturbances following distal femoral physeal fracture-separations. J Bone Joint Surg Am 1983;65:885-893.
6. Hresko MT, Kasser JR: Physeal arrest about the knee associated with nonphyseal fractures in the lower extremity. J Bone Joint Surg Am 1989;71:698-703.
7. Cozen L: Fracture of the proximal portion of the tibia in children followed by valgus deformity. Surg Gynecol Obstet 1953;97:183-188.
8. Jackson DW, Cozen L: Genu valgum as a complication of proximal tibial metaphyseal fractures in children. J Bone Joint Surg Am 1971;53:1571-1578.
9. Taylor SL: Tibial overgrowth: A cause of genu valgum. J Bone Joint Surg Am 1963;45:659.
10. Salter RB, Best T: Pathogenesis and prevention of valgus deformity following fractures of the proximal metaphysial region of the tibia in children. J Bone Joint Surg Br 1972;54:767.
11. Houghton GR, Rooker GD: The role of the periosteum in the growth of long bones: An experimental study in the rabbit. J Bone Joint Surg Br 1979;61:218- 220.
12. Weber BG: Fibrous interposition causing valgus deformity after fracture of the upper tibial metaphysis in children. J Bone Joint Surg Br 1977;59:290-292.
13. Jordan SE, Alonso JE, Cook FF: The etiology of valgus angulation after metaphyseal fractures of the tibia in children. J Pediatr Orthop 1987;7:450- 457.
14. Green NE: Tibia valga caused by asymmetrical overgrowth following a nondisplaced fracture of the proximal tibial metaphysis. J Pediatr Orthop 1983; 3:235-237.
15. Zionts LE, Harcke HT, Brooks KM, et al: Posttraumatic tibia valga: A case demonstrating asymmetric activity at the proximal growth plate on technetium bone scan. J Pediatr Orthop 1987; 7:458-462.
16. Kling TF Jr, Hensinger RN: Angular and torsional deformities of the lower limbs in children. Clin Orthop 1983; 176:136-147.
17. Davids JR, Fisher R, Lum G, et al: Angular deformity of the lower extremity in children with renal osteodystrophy. J Pediatr Orthop 1992;12:291-299.
18. Oppenheim WL, Shayestehfar S, Salusky IB: Tibial physeal changes in renal osteodystrophy: Lateral Blount’s disease. J Pediatr Orthop 1992;12:774-779.
19. Gage JR: Gait analysis: An essential tool in the treatment of cerebral palsy. Clin Orthop 1993;288:126-134.
20. Irwin CE: The iliotibial band: Its role in producing deformity in poliomyelitis. J Bone Joint Surg Am 1949; 21:141-146.
21. Rydholm U, Brattström H, Bylander B, et al: Stapling of the knee in juvenile chronic arthritis. J Pediatr Orthop 1987; 7:63-68.
22. Greene WB: Genu varum and genu valgum in children. Instr Course Lect 1994; 43:151-159.
23. Staheli LT: The lower limb, in Morrissy R (ed): Lovell and Winter’s Pediatric Orthopaedics, 3rd ed. Philadelphia: JB Lippincott, 1990, pp 741- 766.
24. Paley D, Tetsworth KD: Deformity correction by the Ilizarov technique, in Chapman MW, Madison M (eds): Operative Orthopaedics, 2nd ed. Philadelphia: JB Lippincott, 1993, vol 1, pp 883-948.
25. Bowen JR, Torres RR, Forlin E: Partial epiphysiodesis to address genu varum or genu valgum. J Pediatr Orthop 1992; 12:359-364.
26. Blount WP, Clarke GR: Control of bone growth by epiphyseal stapling: A preliminary report. J Bone Joint Surg Am 1949;31:464-478.
27. Zuege RC, Kempken TG, Blount WP: Epiphyseal stapling for angular deformity at the knee. J Bone Joint Surg Am 1979;61:320-329.
28. Paley D, Herzenberg JE, Tetsworth K, et al: Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am 1994;25:425-465.
29. Steel HH, Sandrow RE, Sullivan PD: Complications of tibial osteotomy in children for genu varum or valgum: Evidence that neurological changes are due to ischemia. J Bone Joint Surg Am 1971;53:1629-1635.
30. Zionts LE, MacEwen GD: Spontaneous improvement of post-traumatic tibia valga. J Bone Joint Surg Am 1986; 68:680- 687.
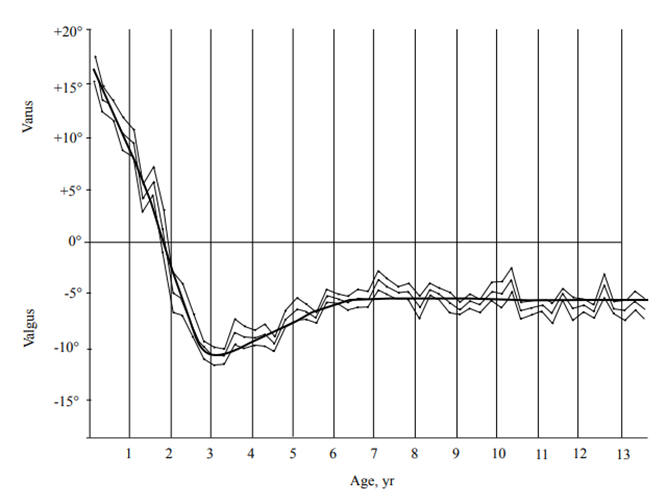
Figure 1

Figure 2
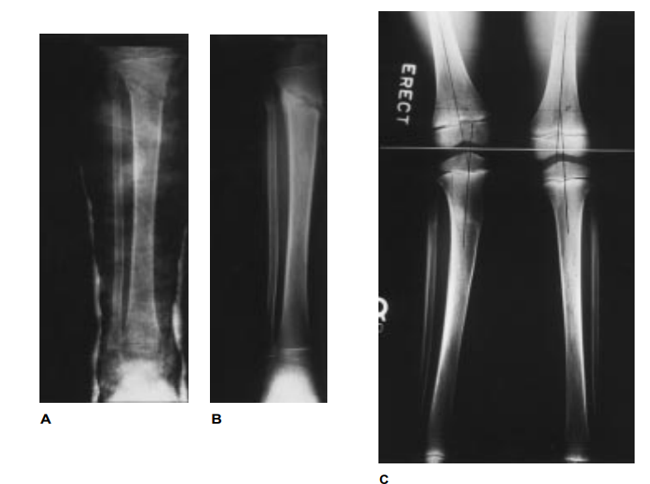
Figure 3
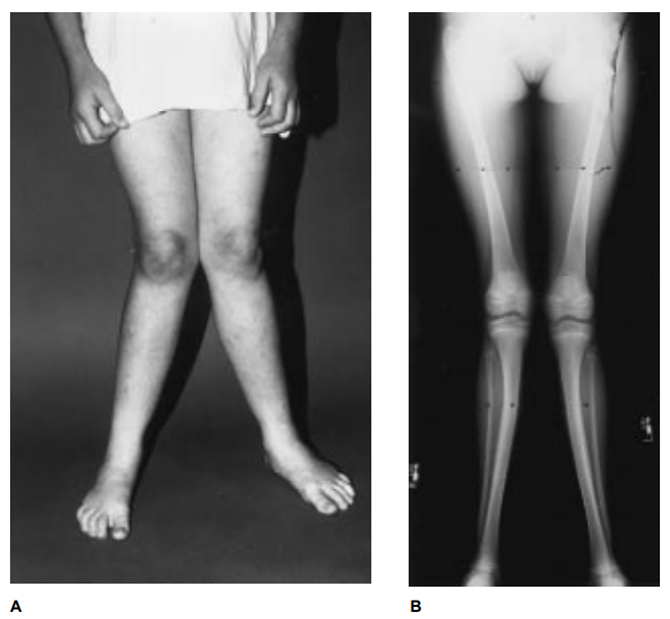
Figure 4

Figure 5
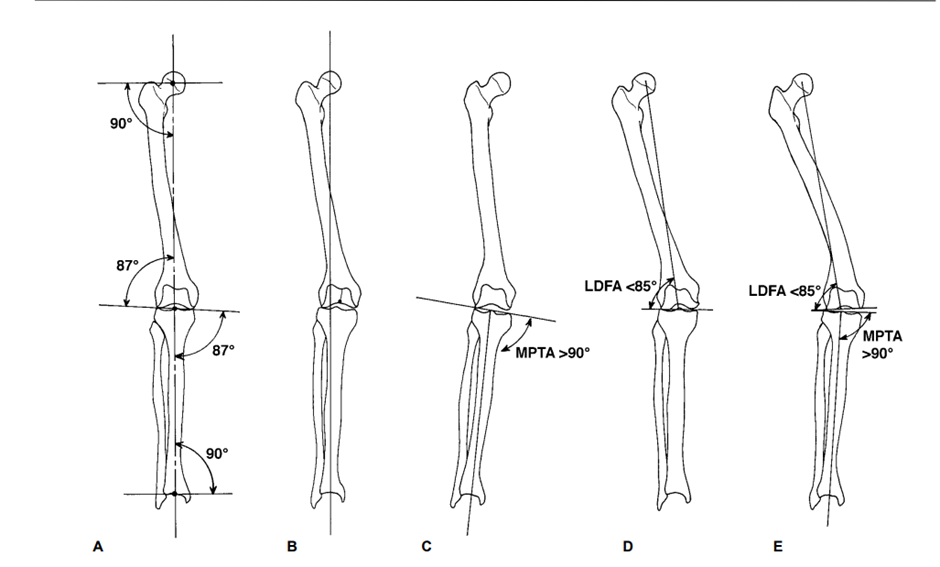
Figure 6
