Lower Limb Deformity in Growing Children: A Review
Lower Limb Deformity in Growing Children: A Review
Kassem El Houcheimi*
*Correspondence to: Kassem El Houcheimi, FACS, MBA, Orthopedic surgeon, Clemenceau Medical Center Dubai.
Copyright
© 2024 Kassem El Houcheimi. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 10 June 2024
Published: 01 July 2024
Lower Limb Deformity in Growing Children: A Review
Background
Lower extremity deformities in children represent a broad group of problems that may be idiopathic or related to an underlying problem. Clubfoot and other foot deformities are mostly lower extremity deformities and are discussed in more detail in separate chapters. Here, unequal limb length, bowed limb, and crooked limb will be examined as examples of longitudinal, rotational, or angular limb deformities. Although it is reasonable to expect a person's legs to be straight and the same length, small differences between legs or right angles are found in more than half of the population. Alignment deformities can be angular or rotational.
While children have a varus (kneetoknee) position in the frontal plane before the age of 2, as they grow, this position gradually turns into a valgus (knee-to-bone) position. Generally, in children aged 7 years, 5, 6 degree valgus occurs in the final femoral - tibial relationship. Most rotation deformities are symmetrical and are considered normal changes that generally improve with age. The best way to think about femur rotation is to imagine the extended femur resting on a flat surface. If the posterior femoral condyle is straight, the femoral neck will rotate from the center and the femoral head will stop at the center (Figure 1).
Figure 1: An example of the femoral shaft at approximately 20 degrees is shown. In this image (and images 2 and 3), the surface gives the impression that the femur of a person lying on their back is "under the spear". (That is, the image is viewed from a point on the ilium, at the level of the femur, from the distal end to the knee). The femoral condyle (blue pattern) on the head and neck surface (yellow) remains in place and points to the acetabulum (red).
Figure 2: Extreme anteversion of the femur is shown here. When the feet point straight forward, this causes the head to point toward the edge of the acetabulum.
Figure 3: Excessive femoral anteversion can be compensated for by foot rotation. This lifts the posterior femoral condyle away from its resting plane, as shown. Therefore, children with weak femur often walk with a pigeon-toed stance. °. When the femur is bent forward, internal rotation of the limb will direct the femoral head toward the center of the acetabulum (Figure 3).
Normal intrauterine tamponade usually causes internal tibial torsion, which in turn causes minor external tibial torsion during development. The disease caused by the deformity itself is called "children's tibial varus" or Blount's disease. (The word "varus" comes from the Latin word meaning "to bend", but refers to the curvature or angulation of a bone or joint in which the distal portion is more medial than the Tibia varus, a condition in which the foot is wider than the tibia, as tested in obese children, early travelers, and Hispanics and African Americans. It is also generally associated with pigeon-toed characteristics. It is less common, but can also occur in children under 10. This condition is called juvenile Blount disease. Juvenile Blount disease is usually a more serious condition. It is also often associated with a femoral deformity and is usually unilateral. At a minimum, a birth history, family history, developmental history, gait analysis, neurological examination, limb measurements, and contour rotations should be included. No symptoms. When parents express concern about the way their child walks, they are often the first to report a difference. Some people state that they get tired quickly while walking due to the increased effort due to the difference, while others complain of back pain.
Measurements can be made in the supine or standing position from the superior iliac crest to the medial malleolus using a tape measure or block test. Move your legs up to the level of the iliac crest and then measure the size of the block to determine the difference. The reason for the length difference. It develops soon after most children start walking. Although most children are asymptomatic, parents often report that their child frequently falls or trips. . However, genu varum does not seem to indicate Blount disease in children younger than 18 months unless the overall deformity is severe or very close to the tibial angle comfort. The most accurate method is longitudinal (hip to ankle) radiography, radiography scan, or computed tomography (CT). your ruler. CT scans can be used in a similar way but can also evaluate limb stiffness and movement. There are also new imaging techniques using low-energy imaging that can provide body length measurements with less energy than XR (EOS imaging). Bone age should also be evaluated to determine the prognosis for growth.
Figure 4: Bottom X-rays are X-rays obtained by placing a probe and moving the beam to the right over each image. The screening usually includes both legs of the film.
Scooped
Radiological evaluation is generally not needed when evaluating patients with pigeon toes. The "foot progression angle" (FPA) must be taken into account: this is the angle formed by the length of the foot and the line of the walking path ("straight ahead" when the patient walks). A negative FPA indicates the inner bushing, a positive FPA indicates the outer bushing. The amount is usually between -5 degrees and +20 degrees, but will vary with age. Once an FPA abnormality is found, the next step is to determine the location of the deformity, such as the hip, tibia, or foot. Both legs rotate inward and outward (Figure 5 left and middle). Greater internal rotation (usually greater than 70 degrees) and decreased external rotation (usually less than 20 degrees) usually indicates strong femoral anteversion or femoral internal rotation. Angle (Figure 5, right) and transankle axis to assess tibial torsion. Foot angle is the angle formed by the axis centering the foot and the axis centering the thigh. The transankle axis is the angle formed by the malleolus axis of the ankle and the coronal plane of the tibia. Similar to FPA, internal rotation is listed as a negative value and external rotation is listed as a positive value. Babies often have weak right foot angles and ankle axis, and these angles gradually change to more fair or better with age.
Figure 5: Left) external hip rotation; middle) internal rotation of the hip; ) angle. People with bunions may have a hill or curve on the outside of their foot instead of a straight edge, a sign of possible metatarsal adduction. Additionally, this often occurs with the medial plantar fold. You can check the heel bisector, which is the axis where the heel connects to the level of the toes. If the line comes out from the second and third toes, this is considered normal because the line comes out further from the toes and this is a sign of forefoot adduction. The examiner must determine whether the deformity is rigid or flexible (passively correctable to moderate or extreme). . (Even if testing is performed, it is generally not recommended to take radiography before this age.)
In order to cut tibial varus, the metaphyseal-diaphyseal angle of the tibia must be measured in each radiograph (Figure 6). Angles below 10 degrees are considered normal and disappear over time. Any angle greater than 10 degrees is considered abnormal and should be carefully monitored with examination and radiographs.
Figure 6: The metaphyseal-diaphyseal angle is a bit of a bad name because it is the angle between the metaphyseal slope and the line perpendicular to the diaphysis, not the diaphysis itself. To visualize this, draw a line along the length of the tibia (green) and a second line along its metaphyseal slope (blue). Then draw another line (red) perpendicular to the horizontal line. This angle is defined by the intersection of three (red) lines with the (blue) line along the metaphyseal slope.
In more severe cases, metaphyseal lesions of the tibia may be seen with a negative impression of the outer trunk ( Figure 7). In addition, orthostatic radiographic films can be used to measure the deformity angle and determine the mechanical axis of the lower extremity.
Figure 7: Infant tibia varus, proximal metaphyseal beak
- Differential Diagnosis
- Leg Length Difference
- Leg length variation may be caused by the following factors or a combination of them:
- ✠Injuries: Long bones made of unequal length Most common One of the reasons. Diaphyseal fractures in growing children often cause the leg to grow faster and become longer than the leg. In addition, bones healing in a short position or fractures that have healed with bone growth can also cause lower back pain. Dysplasia: hemihypertrophy, proximal femoral partial defect, hip dysplasia, fibular and tibial hemimelia, unilateral clubfoot, neurofibromatosis, various exostoses, idiopathic or neuromuscular scoliosis. Packaging is due to endolocalization but there may also be some genetic factors, meaning these are usually passed down in families. These may be caused by the following or a combination of these:
- Metatarsal adduction: Often seen in infants. Oblique foot, congenital hallux varus and clubfoot should also be excluded. . Persistent O-legs over 18 months are considered pathological and may be caused by or related to one of the following conditions:
- Tibial varum (Blount) in juveniles: Pathological genu varum in children over 10 years of age. Tibial varus in infants is more unilateral, usually bilateral (Figure 8). Osteogenesis imperfecta, various exostoses, Maffucci syndrome, Ollier disease, congenital pseudoarthrosis (anterolateral curvature) of the tibia.
Figure 8: Adolescent tibia vara
Figure 9: Severe bowing of the tibia (and femur) due to rickets. Rickets usually occur because of a lack of vitamin D or calcium, and results in weak bones in children. Adults can experience a similar condition, which is known as osteomalacia
Treatment Options and Outcomes
If there is a disorder/dysplasia or metabolic bone disease, it may be beneficial to see a geneticist for diagnosis (although genetic testing is rare for some physical disorders such as fibular hemiplegia deformity).
Leg Length Difference
Treatment of leg length difference in pediatric patients depends on the cause and the desired bone growth difference. If the leg difference is due to scoliosis, disease or a condition such as hip dysplasia, the problem must be addressed first before a solution can be made if the leg difference has occurred. Leg length difference of 2 cm or less (depending on future growth) is best treated with observation with insoles if necessary. Treatments such as epiphyseal fixation (surgical removal of the epiphyseal plates to prevent growth). Sometimes long surgeries can be combined with short surgeries on the "long" leg. Long-term surgery may be considered for a difference of 4 cm or less after a decision-making process that is shared with the family and includes risks and benefits.
Most children with bowed feet can be treated through self-monitoring and are expected to correct on their own by age 2 to 3. Mild bowing that persists beyond this age can be treated with a knee-ankle-foot orthosis (KAFO), but the results of this approach are mixed. For more severe arches or those that have persisted for more than 4 years, surgical intervention should be considered. Surgical options include tibial-fibular osteotomy, lateral hemi-epiphysiodesis with growth, or medial epiphyseal release (rod resection). Most of these surgeries are performed together.
Conclusion
In most cases, cords can be treated non-surgically with the comfort and education of the parents. As they grow older, most children will become pig-toed. These children should not be restricted and should participate in similar activities with their peers. Even rare cases of severe femoral anteversion or internal tibial torsion that do not resolve by age 8 cause aesthetic and functional impairment and may require consideration of repair osteotomy.
Reference
1. Chantrain A. Knee joint in soccer players: osteoarthritis and axis deviation. Med Sci Sports Exerc. 1985;17:434–9.
2. Brouwer GM, Van Tol AW, Bergink AP, et al. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis Rheum. 2007;56:1204–11.
3. Sharma L, Song J, Felson DT, et al. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286:188–95.
4. Wu DD, Burr DB, Boyd RD, Radin EL. Bone and cartilage changes following experimental varus or valgus tibial angulation. J Orthop Res. 1990;8:572–85.
5. Bradway JK, Klassen RA, Peterson HA. Blount disease: a review of the English literature. J Pediatr Orthop. 1987;7:472–80.
6. Lun V, Meeuwisse H, Stergiou P, Stefanyshyn D. Relation between running injury and static lower limb alignment inrecreational runners. Brit J Sports Med. 2004;38:576–80.
7. Messier SP, Davis SE, Curl WW, Lowery RB, Pack RJ. Etiologic factors associated with patelofemoral pain in runners. Med Sci Sports Exerc. 1991;23:1008–15.
8. Taunton JE, Ryan MB, Clement DB, Mc Kenzie DC, Lloyd Smith DR, Zumbo BD. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med. 2002;36:95–101.
9. van Mechelen W. Running injuries. A review of the epidemiological literature. Sports Med. 1992;14:320–35.
10. Wen DY, Puffer JC, Schmalzried TP. Injuries in runners: a prospective study of alignment. Clin J Sport Med. 1998;8:187–94.
11. Arazi M, O?ün TC, Memik R. Normal development of the tibiofemoral angle in children: a clinical study of 590 normal subjects from 3 to 17 years of age. J Pediatr Orthop. 2001;21:264–7.
12. Gordon CM, Feldman HA, Sinclair L, et al. Prevalence of vitamin D deficiency among healthy infants and toddlers. Arch Pediatr Adolesc Med. 2008;162:505–12.
13. Christie DP. The spectrum of radiographic bone changes in children with fluorosis. Radiology. 1980;136:85–90.
14. Bajpai A, Bardia A, Mantan M, et al. Non–azotemic refractory rickets in Indian children. Indian Pediatr. 2005;42:23–30.
15. Kwee TC, Beemer F A, Beek FJ, et al. Knee radiography in the diagnosis of skeletal dysplasias. Pediatr Radiol. 2006;36:8–15.
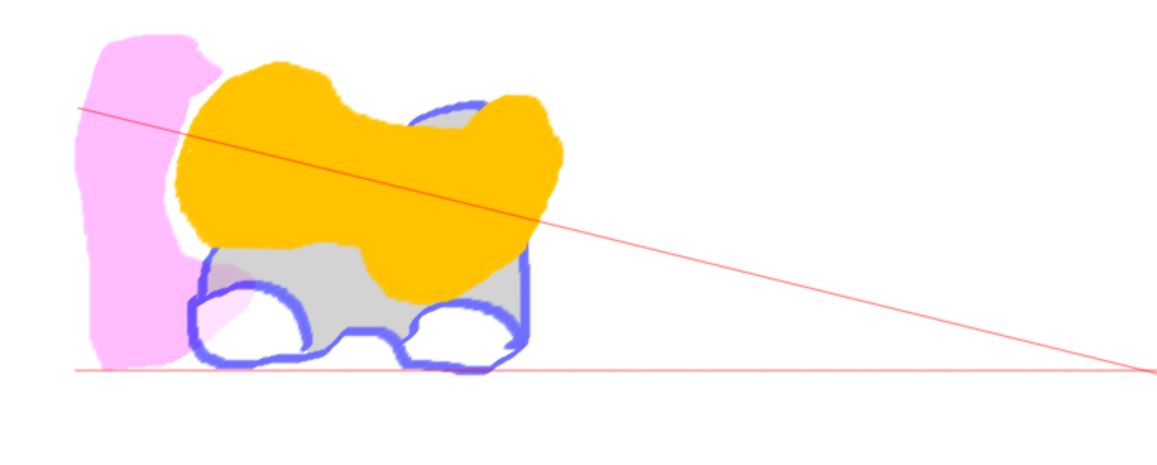
Figure 1
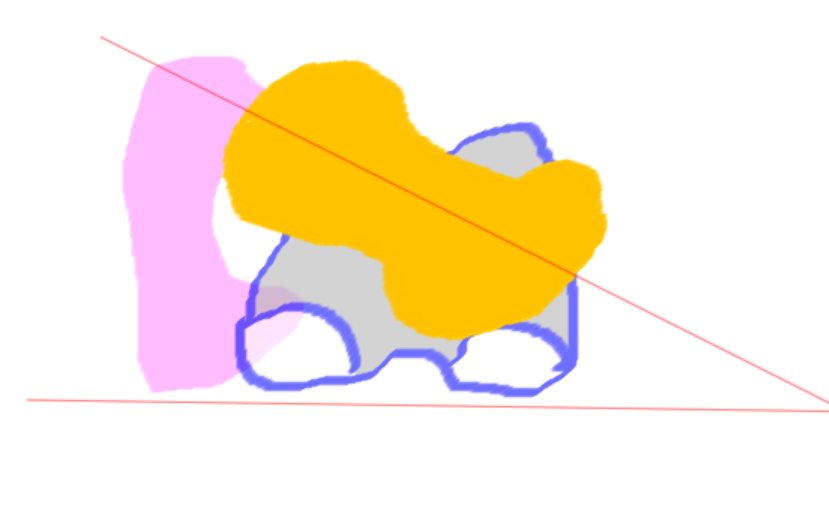
Figure 2

Figure 3
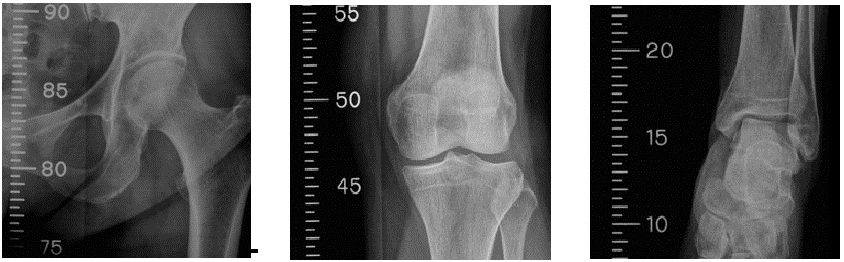
Figure 4
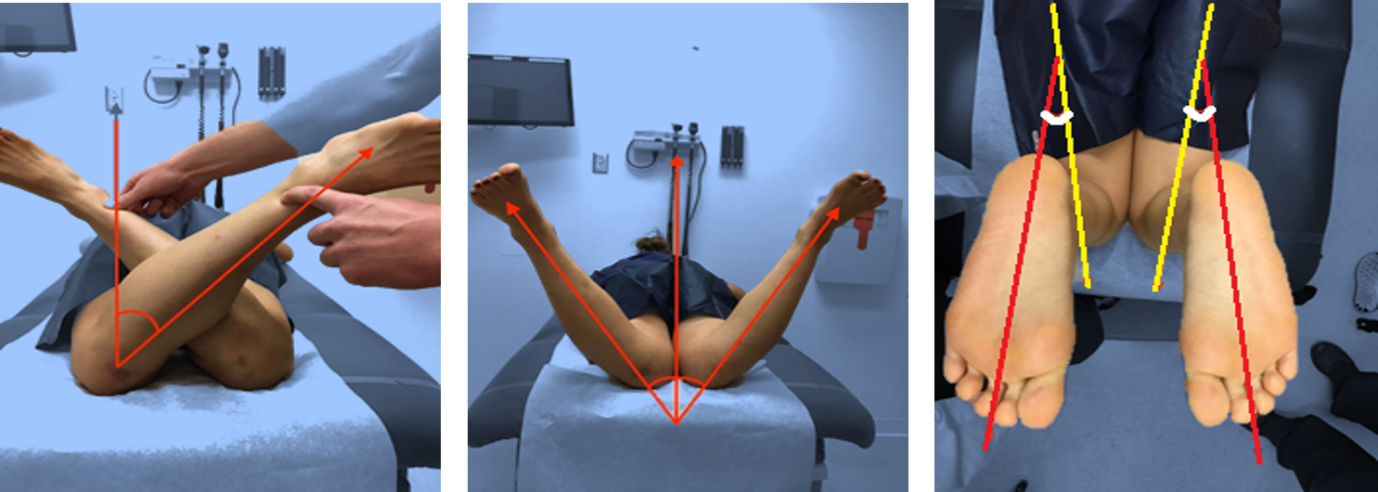
Figure 5
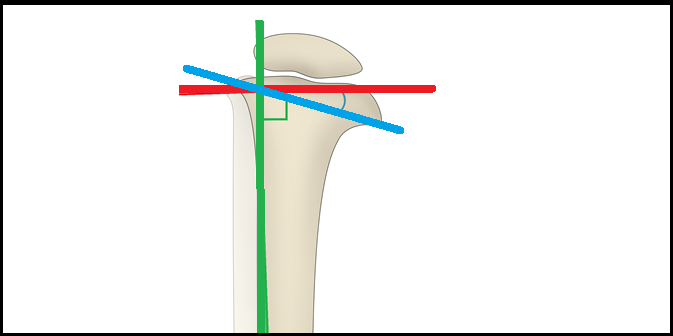
Figure 6
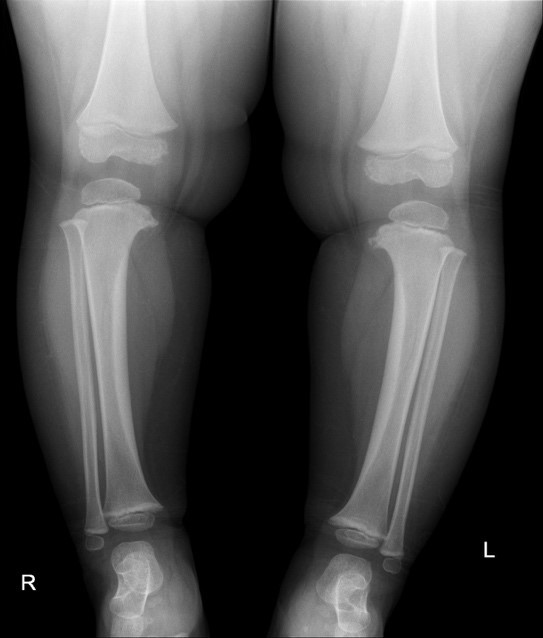
Figure 7

Figure 8

Figure 9
