Malingerer of Malignancy in an African Lady
Malingerer of Malignancy in an African Lady
Dr Pakhee Aggarwal *
*Correspondence to: Dr Pakhee Aggarwal, Department of Gynaecology Oncology & Robotic Surgery, Apollo Cancer Centres, Indraprastha Apollo Hospitals, Delhi, India.
Copyright
© 2024 Dr Pakhee Aggarwal. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 08 July 2024
Published: 25 July 2024
Abstract
Abdominal distension, ascites, raised tumour markers are taken as highly indicative of ovarian/peritoneal cancer in women above the age of 45 years. In patients with these features, in whom surgery is not immediately contemplated, biopsy is needed to prove the diagnosis and start chemotherapy. However, when repeated tests to confirm malignancy are inconclusive, and patient belongs to an endemic area, other diagnoses should be kept in mind, even if the patient is immunocompetent. This case highlights this aspect and led to the diagnosis of a non-malignant, curable disease in a lady of African descent who was being worked up for disseminated cancer, due to the high index of suspicion. She made excellent recovery, and six months after treatment is free of disease.
Keywords: peritoneal, disseminated, ovarian cancer, raised CA-125, tuberculosis
Malingerer of Malignancy in an African Lady
Introduction
Ovarian/peritoneal cancer is a disease of high morbidity & mortality. It is important to diagnose it conclusively before definitive treatment is started. Ovarian/peritoneal granulomatous disease, is uncommon in immune-competent persons, but may rarely be seen in endemic populations. The clinical, radiological and biochemical features of both may overlap. Only direct visualisation and biopsy can confirm the diagnosis. The below case highlights the importance of having a high index of suspicion to make the correct diagnosis, keeping the ethnicity in mind.
Case Report
Mrs. S, 46 years, African descent, came with complaints of abdominal distension for four months and elevated serum immunoglobulin (alpha-1 and gamma globulins raised with M-spike of 1.16g/dL). She had a history of therapeutic ascitic tapping done thrice in Mozambique. There were no constitutional symptoms of fever, weight loss or night sweats. Detailed evaluation and workup for suspected malignancy after presentation to our hospital revealed bulky ovaries with cystic lesions in the ovary, gross ascites, omental thickening and thickening of peritoneal reflections on PET-CT scan. (Fig 1)
Fig 1: PET-CT showing FDG-avid omental & peritoneal thickening
Her blood investigations were as follows: CA125 – 324U/mL (N <35U/mL), CEA – 0.3ng/mL (N< 4.7ng/mL), LDH – 215IU/L (N<247 IU/L), Serum IgG – 2898 mg/dL (N 650-1600 mg/dL), Serum IgA – 310 mg/dL (N 40-35- mg/dL), Serum IgM – 88 mg/dL (N 50-300 mg/dL), Serum albumin 3.9g/dL (N 3.5-5.2 g/dL), ESR 46mm/1st hr (N <12 mm/1st hr), CRP 177.4 mg/dL (N< 6mg/dL), TB Quantiferon 0.108 u/mL (<0.35 u/ml – MTB not likely).
She underwent ascitic tapping (therapeutic) to relieve her symptoms as well as to make a diagnosis of the underlying aetiology. Ascitic tap was negative for malignant cells, AFB staining and Gene Expert for Mycobacterium TB. ADA was 131 U/L (N <40U/L). Ascitic fluid glucose was 98mg/dL, protein 5.6g/L, white cells 1120 cells/mm3 (93% lymphocytes, 7% neutrophils), red cells 3520 cells/mm3 with a yellow turbid appearance.
Due to lack of conclusive tissue diagnosis of cancer, chemotherapy could not be started even though the clinical picture was highly suggestive. She underwent assessment laparoscopy (which in the presence of gross ascites is a challenge), to assess feasibility for debulking surgery and obtain tissue diagnosis. Intra-operatively there was large volume ascites (more than four litres was drained), innumerable nodular deposits (0.5cm size) over all intra-abdominal organs and peritoneal surfaces, clumping of the bowels and omentum. (Fig 2) Biopsies were taken from accessible organs (ovary, endometrium, omentum) and peritoneal reflections of various sites and sent for frozen section. None of the samples showed conclusive evidence of malignancy, however, biopsy from the ovary revealed a solitary epithelioid cell granuloma. Ascitic fluid picture was exudative with lymphocytosis. Final biopsy report of all sites showed several Langhan's type of giant cells within granulomas, with central caseous necrosis. Final diagnosis was granulomatous oophoritis & granulomatous inflammation. With this she was started on definitive treatment with four drug ATT regimen and made uneventful recovery. At six month follow up, her CA-125 is in the normal range and there is no evidence of ascites on ultrasound. Incidentally, her AFB culture at six weeks was negative.
Fig 2: Laparoscopy image with gross ascites, nodular deposits in omentum & peritoneum (laparotomy was avoided
Discussion
Peritoneal tuberculosis is a form of extra-pulmonary tuberculosis, which may be insidious in onset with non-specific symptoms. The common symptoms are abdominal pain, distention and constitutional symptoms like fever, night sweats and weight loss. Incidentally, these are also the symptoms of ovarian cancer. In both these conditions, ascites is of the exudative type. Imaging may show the presence of peritoneal carcinomatosis type picture, as in the present case. PET-CT is also not able to distinguish the avidity as being due to cancer or tuberculosis1. To clinch the microbiological diagnosis, either ZN staining of the ascitic fluid or culture for AFB should be positive. However, being pauci-bacillary in nature, this may not always be possible. A large volume of ascites needs to be centrifuged and cultured to have acceptable sensitivity for detection2. ADA is sensitive for peritoneal tuberculosis, and tends to be higher in TB than in malignancy. Absolute cut-offs have not been defined, but levels higher than 30 U/L have been shown in some studies to be sensitive for tuberculosis3. In the present case, ADA was raised, but no other features were supportive, so peritoneoscopy and biopsy, which is the gold standard to diagnose both cancer and tuberculosis was carried out.
Peritoneal tuberculosis is common in persons of African descent, as in this patient. Isolated peritoneal TB without pulmonary TB is very uncommon, and AFB staining and culture have sensitivities of 3% and 20% respectively4. Biopsy then becomes the gold standard to diagnose the disease. Assessment laparoscopy is also used in ovarian cancer to diagnose and determine resectability of disease. Thus, it was the logical next step in this patient.
The intra-operative picture was of diffuse sub-centimetre nodules over all peritoneal and organ surfaces, and can be seen in both peritoneal carcinomatosis and miliary peritoneal tuberculosis. The final diagnosis was secured by finding no malignant cells and instead finding typical granulomatous inflammation on the peritoneal nodules sent for frozen section analysis. Peritoneal TB may be wet type with massive ascites, fibrotic fixed type with matted bowel and omental masses, or dry type with dense adhesions. Wet type is the most common5 and this patient had a mixture of the wet and fibrotic type of disease.
In this, patient the ovarian biopsy was also positive for granulomas, indicating that it was a case of disseminated abdominopelvic TB which could have arisen from the ovary and spread like cancer. Usually involvement of genital organs in extra-pulmonary TB is by lympho-hematogenous spread. Miliary disease is seen in immune-deficiency states more commonly, but this patient was immune-competent, making the diagnosis challenging.
One may argue that empirical treatment of TB could have been started to assess response, but due to the confounding suspicion of multiple myeloma in the mix, it was deemed prudent to treat the definitive diagnosis, and malignancy was high up on the list. Treatment of peritoneal carcinomatosis with palliative chemotherapy is very different from antitubercular treatment with high chance of cure. Hence, appropriate decision making is crucial. Diagnosis was made on laparotomy in the bygone era6, but laparoscopy gives the minimally invasive advantage as extensive surgery in not indicated in either of the two conditions. CA-125 although not diagnostic of either condition, can be used as marker for follow up to assess response to therapy.
Conclusion
This case highlights the awareness of diagnoses which can mimic malignancy - clinically, biochemically and radiologically. The overlap of signs and symptoms between ovarian/ peritoneal tuberculosis and ovarian/ peritoneal cancer is high and only biopsy remains the gold standard to differentiate the two. A high index of suspicion and early recourse to laparoscopy and biopsy can help to diagnose this condition.
Acknowledgements: nil
Presentation at Meeting: nil
Source of Funding: nil
Conflict of Interest: nil
IRB Approval: Not applicable
Patient Consent: taken
References
1.Jeffry L, Kerrou K, Camatte S, et al.. Peritoneal tuberculosis revealed by carcinomatosis on CT scan and uptake at FDG-PET. BJOG 2003;110:1129–31.
2. Koff A, Azar MM. Diagnosing peritoneal tuberculosis. BMJ Case Rep. 2020 Feb 6;13(2):e233131.
3. Shen Y-C, Wang T, Chen L, et al.. Diagnostic accuracy of adenosine deaminase for tuberculous peritonitis: a meta-analysis. Arch Med Sci 2013;9:601–7.
4. Ogah I, Milne F, Zevin B. Peritoneal tuberculosis. CMAJ. 2021 Nov 1;193(43):E1664.
5. Chen IH, Torng PL, Lee CY, Lee KH, Hsu HC, Cheng WF. Diagnosis of Peritoneal Tuberculosis from Primary Peritoneal Cancer. Int J Environ Res Public Health. 2021 Oct 3;18(19):10407.
6. Bilgin T, Karabay A, Dolar E, Develio?lu OH. Peritoneal tuberculosis with pelvic abdominal mass, ascites and elevated CA 125 mimicking advanced ovarian carcinoma: a series of 10 cases. Int J Gynecol Cancer. 2001 Jul-Aug;11(4):290-4.
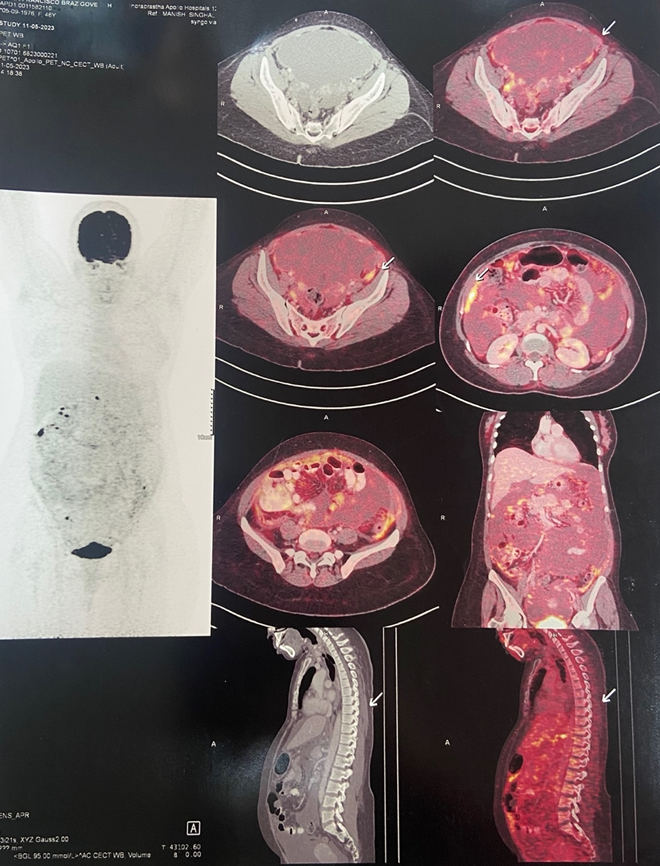
Figure 1
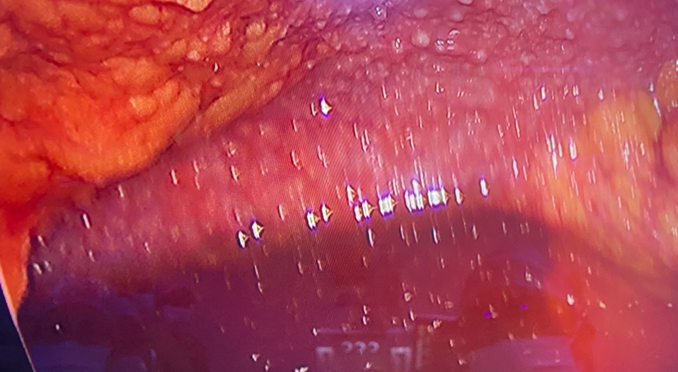
Figure 2
